10 Chapter 01 – Evidence-Based Research and Physical Therapy
Objectives
- Discuss current practice issues that are having an impact on the delivery of physical therapy.
- Discuss the importance of evidenced-based practice.
- Develop a beginning understanding of professional literature/scholarly evidence
You no doubt have heard the term ‘evidenced-based practice’ (EBP) used before. It is used so much it has become a buzz phrase all to itself. Maybe it is time that we unpack that phrase as it is, cliché or not, a very relevant term for the PTA. You will soon be an evidence-based practitioner, so let’s start at the beginning: What is EBP?
EBP is clinical practice that reflects the integration of the:
- The best available research
- The clinician’s expertise and
- The patient’s values & circumstances
To make any sense of this at all, we need to understand what ‘evidence-based’ means if we are to understand what “the best available research” means.
Evidence-based just means that we use the scientific method to gather our facts, not opinions or hunches. When we act based on a folk tales or other stories, say, of how someone’s cousin used garlic to grow taller or that alligators are aggressive because they have too many teeth, we are using anecdotal evidence.
Anecdotal evidence is not really evidence. It may be presented as evidence, but as anecdotes evidence is when conclusions are drawn from stories (personal testimony) rather than scientific evidence. This means that anecdotal findings cannot be objectively investigated by the scientific method; they are not repeatable.
Evidence-based research lets us confidently to choose a modality because peer-reviewed research studies have validated its efficacy. In other words, we can confidentially use ultrasound as a form of heat (making ultrasound a thermal modality) because research has been performed that objectively to measure the changes in blood flow and tissue temperature that occur in response to the ultrasound as well as the effects the ultrasound has on pain, range of motion (ROM), strength, etc.
The research studies on ultrasound offer us objective information, with measurable results, giving us data that is free from opinion. This does not mean it is without its flaws, but more on that in just a minute. Let’s continue unpacking this term of evidence-based practice.
If we are comfortable with the ‘evidence-based’ part of the term, what does the practice part mean? Well, it refers to the use of evidence in a way that is specific to the needs of the patient seated right before you. Huh? Well, as you will see in your library project, when you put in, for example, ultrasound and physical therapy as search terms, you may get thousands of hits. Whoa. Now what?
Well, you will learn strategies in the library as well as here to help you focus your search. You want to seek out a way to find just the studies most relevant to that patient before you. Part of that will be the use of a strategy that will help you find the best available research (meaning research as specific to your patient as possible).
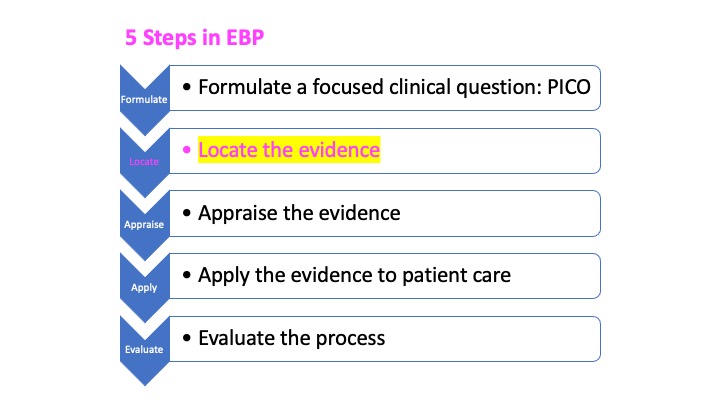
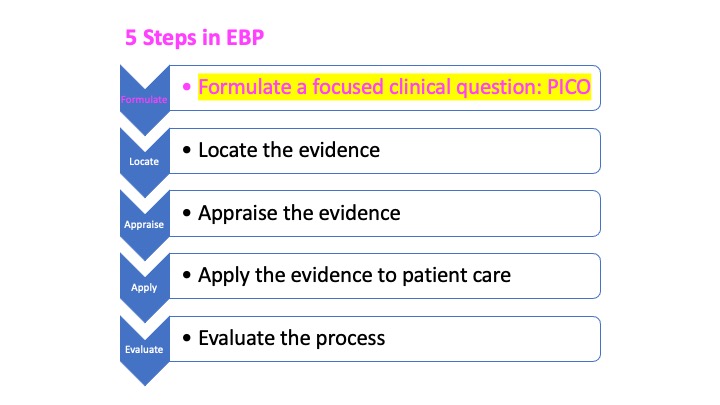
To do so, we will use the 5 steps found in EBP. We will spend most of our time here (this OER) on the first step. You will be spending most of your time at the library on the second step. We will then touch on the final steps at the end of this chapter.
-
Formulate a focused clinical question. To do this, we often use a PICO. Just a simple strategy (template) to help use narrow down our search to the “patient in front of us”.
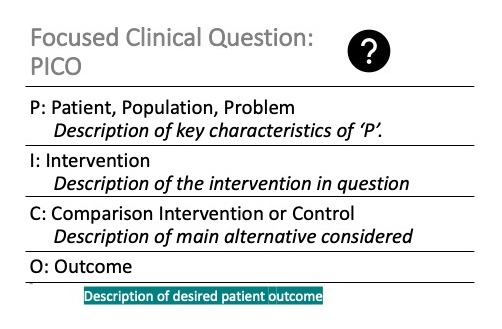
P: Represents the KEY CHARACTERISTICS of our patient: They may include:
The primary problem of patient
The age, sex, race, medications of the patient
The diagnosis of patient
It will help you to focus on the “Key” Characteristics of your patient…think A and B rather than A through Z
I: Represents the intervention you are researching. Interventions are procedures that we perform in an effort to cause a favorable change in the patient’s status.
EXAMPLES:
Therapeutic exercise, education, thermal / electro modalities, functional training, aerobic activities, gait training, balance training, transfer training, bed mobility…
C: Represents a Control group or a Comparison Intervention or group. This will be the main alternative intervention you are considering. It can be either one of the following.
- The typical treatment for the condition
- A placebo
- No intervention
O: Represents the desired patient outcome you seek as a result of the intervention.
Please note: It needs to be MEASURABLE
How about some examples for clarity?
Let’s use a formula or template for our PICO. Something like this will work for many PICOs.
For _______(P), would _____(I) compared with _________ ( C ) affect ______ (O)
Now we can fill-in the blanks with our P, I, C and O. For example, let’s say we want to know if regular exercise helps students do better in PT 100S. We might write a PICO like this:
Do college-aged adults (P), who exercise daily (I) compared to college-aged adults who do not exercise (C) score higher in PT100S (O)?
Or maybe you are on your first clinical and your clinical instructor (CI) asks you which balance test you think is better at detecting a fall risk for a patient with Parkinson’s Disease (PD). You might write something like….
For _______(P), would _____(I) compared with _________ ( C ) affect ______ (O)
In patients with PD (P), is the use of the Berg Balance Test (I) more accurate than the Timed up & Go Test (C) in assessing the risk for a fall (O)
Your friend has just returned from the doctor with a prescription for tramadol to help with back pain d/t to a HNP. You are surprised that the doctor did not include an order for physical therapy. How would you right a PICO to help you determine if your friend should request a PT referral.
For patients with back pain (P), would Physical Therapy (I) compared with Analgesics (C) decrease pain more effectively (O)
REFLECTION:Take a moment now to consider any clinical interests you have now. Can you create a PICO? This will be part of this assignment. Look over the diagnoses’ and interventions at the end of this chapter to get your ideas flowing.
I will trust that your library experience will cover this in great detail and in an enjoyable manner.
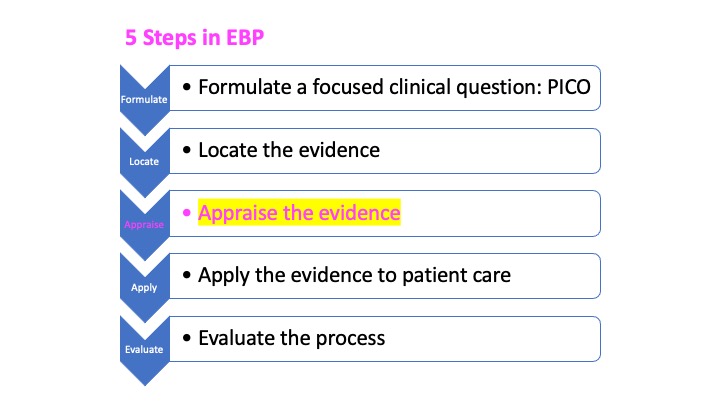
Appraising the evidence is simply the process of analyzing the evidence. We ask questions to see if the evidence presented in the study is valid and relevant to our patient. Questions like:
-
-
- Does the study address our specific clinical question?
- Do the subjects in the study have characteristics that are similar to my patient?
- Was the study published in a peer-reviewed medium or is it more anecdotal?
- Is the context of the study consistent with contemporary practice or is it outdated?
AND… - Is the evidence reliable and valid?
- — Let’s take look at these two important concepts
-
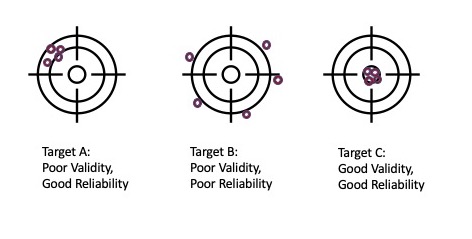
RELIABILITY IMPLIES CONSISTENCY:
-
-
- If you perform a “test” five times in a row, you should get roughly the same results every time.
- Reliability, then, is a measure of the stability, consistency or repeatability of a test.
- Sometimes tests (for example, goniometry – measuring ROM) have very good intra-rater reliability, but its inter-rater reliability, although good, is not as good. This means that when you measure your patient’s knee flexion PROM at 9:00am and then repeat it at 9:05 am, you will probably have the same reading. However, if another therapist were to measure the same patient’s knee flexion at 9:05 am, they would probably be a degree or two off from yours. That is due to the limited precision of a goniometer. It is rather good (and clinically more than reliable enough to be used as a measurement tool) as you will learn next semester, but not perfect.
- Please know the difference between intra (between you and yourself) and inter rater (between you and others) reliability.
-
A TEST IS VALID IF IT MEASURES WHAT IT IS SUPPOSED TO MEASURE.
-
-
- If a thermometer was a degree off, it would be reliable (it would give you the same results each time), but it would not be valid (because the thermometer wasn’t recording the correct temperature).
-
The answers to questions like this will let us know if we should consider the evidence in the research as applicable to our patient.
-
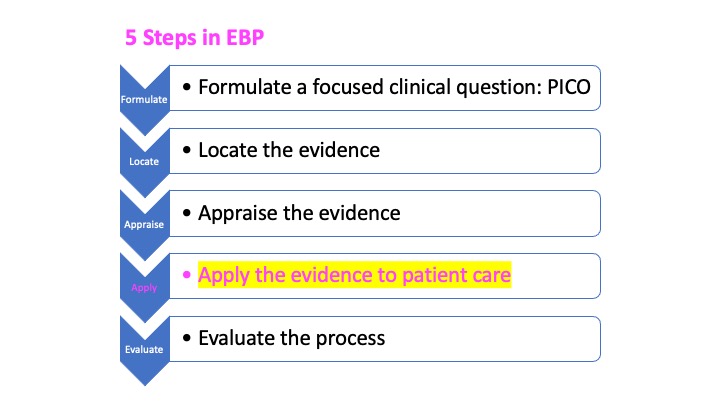
APPLY The EVIDENCE
So now that we think we found the best possible evidence-based research for our patient, you would think we can just apply it to our patient. We first, however, need to think back to the tenets of EBP. If you remember it had three parts and at this point, we only have addressed one. Let’s take a quick look at the other two.
To review: EBP is the integration of
- The best available research
- The clinician’s expertise
- The patient’s values & circumstances:
So, we have addressed the best available evidence: X
Next, we need to consider the: The clinician’s expertise. Does the clinician have any experience with the intervention(s) that the research studies suggest being most beneficial? Is the clinician competent? Does the clinician believe the research or is the clinician biased against the findings? Can the clinician remediate any of their barriers to success using the intervention(s)?
If the answers to these questions and others like it is no, then regardless of what the evidence suggests, the results for the patient cannot be expected to be as favorable. Make sense?
Finally, we can look in a similar manner to the patient’s values & circumstances. These include the patient’s: Life Experiences, Social Support, Personal Resources, Culture, Religion, Living Situation, Attitudes & Beliefs, Family Network.
If the patient’s circumstances do not support the intervention(s), favorable results cannot be expected. Let’s think on an example of how this may occur.
REFLECTION: Your research indicates that your patient’s back pain would improve if they were to receive a particular type of manual physical therapy. You are delighted to hear this because you have just completed a week of advanced training in this technique and you proudly have the certificate (and continuing education credits) to prove it. After explaining all of this good news to your patient, however, they look downcast. They explain that they will not participate in any manual therapy interventions.
Why might this be? Please consider the various criteria regarding a patient’s values and circumstances as you offer your reflection.
And now….once the best evidence is found, ther therapist is prepared and competent in all ways to deliver the intervention and the patient is appropriate to receive it….you can provide the intervention😊!
- The best available research: X
- The clinician’s expertise: X
- The patient’s values & circumstances: X
-
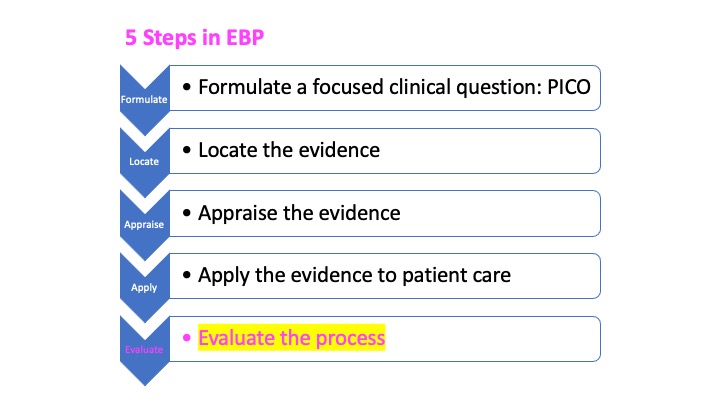
EVALUATE The PROCESS
Let’s assume for the moment that, after you discovered the reasons why your patient was declining your manual therapy interventions, you both were able to collaborate on a winning alternative. An alternative that resulted in the patient becoming painfree and returning to their prior life activities. At this point, you would go back and evaluate your process. This is just like the self-assessment you are doing in class (your Professional Behaviors form) and will do countless times as a clinician.
You will reflect on your process and, in so doing, learn not only how you could have improved some aspects of it, but what parts went right and helped you find success. This part of the process is very much like reviewing an exam to learn why you had the errors you did as well as to learn what parts of your study strategy were successful. All of this reflection will, in the end, save you valuable time and make you a far more effective clinician!
EBP ASSIGNMENT
Please create a PICO based on your research topic and submit it on canvas. Below is my example, but you can use images as well. Make it your own.
That worksheet will be submitted on canvas.
Format for your assignment (The database search will be done in the library with their staff assisting)
PICO: In patients with MS, is the use of the Berg Balance Test more accurate than the Timed up & Go Test in assessing the risk for a fall.
Most useful Database: CINAHL because it was it was easy to use and gave me the most relevant articles.
Most useful lesson learned: I had way too many hits with just balance tests. I needed to pick one. Even then, still too many hits so I needed to refine my patient population to a single diagnosis.
For patients with MS, is the use of the Berg Balance Test more accurate than the Timed up & Go Test in assessing the risk for a fall
Most useful Database: CINAHL because it was easy to use and gave me the more relevant articles.
Most useful lesson learned: I had way too many hits with just balance tests. I needed to pick one. Even then , still too many hits so I needed to refine my patient population to a single diagnosis – so I chose MS.
Common Diagnoses you will encounter in PT.
TBI: Traumatic Brain Injury
MS: Multiple Sclerosis
SCI: Spinal Cord Injury
CVA: Cerebral Vascular Accident
MI: Myocardial Infarction
CAD: Coronary Artery Disease
TKR: Total Knee Replacement
THR: Total Hip Replacement
ACL Tear
Spinal Stenosis
HNP: Herniated Nucleolus Pulposus
COPD: Chronic Obstructive Pulmonary Disease
CHF: Congestive Heart Failure
Rotator Cuff Tear
Cerebral Palsy
Muscular Dystrophy
Autism
Down’s Syndrome
A Few Common Interventions, based on diagnosis:
Therapeutic exercise.
Balance Training.
Ultrasound. Electric stimulation.
Neuromuscular stimulation.
Gait training.
Massage/ Soft Tissue Mobilization.
Aquatic therapy.
Cervical or Lumbar traction.