7 Lab 04: Vital Signs
_
TERMS
Click on each term to review what it means.
LAB OBJECTIVES
- Accurately measure STANDARD VITAL SIGNS including:
- Describe the physiological significance of:
- Body temperature
- Pulse
- Blood pressure
- Respiration
- Pain.
- Describe the physiological significance of:
- Body temperature, heart rate, blood pressure, pulse oximetry, and respiration rate.
- Identify normal values for:
- Body temperature, heart rate, blood pressure, pulse oximetry, and respiration rate.
- List possible causes of elevated and lowered values for:
- Body temperature, heart rate, blood pressure, pulse oximetry, and respiration rate.
- Describe the physiological significance of:
- PULSE RATE: Recognize and discuss the meaning of:
- Normal pulse rate, elevated pulse rate and lowered pulse rate.
- Locate and palpate a patient’s arterial pulse at various sites.
- Perform all activities required to measure a pulse.
- Accurately count and record the pulse rate in beats per minute.
- Use appropriate professional terminology to accurately describe a patient’s pulse in terms of rate, rhythm, and volume.
- PERFORM all activities required in the measuring of BLOOD PRESSURE:
- by the use of a sphygmomanometer.
- Discuss principles related to the use of equipment necessary for measuring blood pressure.
- ACCURATELY count and record the RESPIRATION RATE in breaths per minute.
- Use appropriate professional terminology to accurately describe a patient’s respiration in terms of rate, depth, and rhythm.
- Recognize the difference between thoracic and abdominal breathing and demonstrate each type of breathing pattern.
- EXPLAIN the various PAIN scales for patient use.
- COMPARE patient vital signs to normative values for a given case scenario
- Determine a patient’s response to change in position by measuring vital sign before and after the intervention.
- Using role play, respond effectively when a patient’s vital signs indicate the need for emergency intervention.
INTRODUCTION:
Welcome to one of our more medically interesting lab sections. While you will certainly feel like a “therapist” as we perform our transfer and gait labs, this week, you may begin to see yourself developing into a “clinician” as you learn to how to measure vital signs and understand their significance in the care of your patient.
Your ability to accurately measure and monitor vital signs before, during and after your patient treatment will allow you to:
-
Determine if the patient is appropriate for a given treatment:
Prior to treatment we measure baseline vital signs. We need to see if our patient’s vital signs all within acceptable limits before we can begin our care. Sometimes a patient may develop an illness while under our care, be experiencing an unfavorable reaction to one of their medications or have had any number of incidents occur to them since we last saw them (including the addition of a new medication).
Sometimes, a patient’s comorbidities (co-existing illnesses) may ‘act up’ due to the illness or injury that brought them to see us. Monitoring vital signs before we begin will let us know if our patient is safe for treatment…and if not, we will have information to share with the Physical Therapist to explain why. That information will help decide how to proceed: From just modifying the exercises to getting the patient to the emergency room.
-
Determine the impact treatment may have on the patient.
Our baseline measurements give us data for comparison later in our treatment. We can, after our patient completes an exercise or activity, measure their vital signs to determine if (and to what degree) our treatment impacted them. This will allow us to make a fact-based determination if we should continue, modify or terminate the treatment. This information is entered in the medical record and can be reviewed by others involved in the care of the patient. This method of documentation, of comparing a patient’s status from one not to another to make sound clinical decisions is, cleverly enough, referred to as comparative documentation.
REFLECTION:
Your patient has just had surgery on their knee two days ago (this is POD 2. “Post-Operative Day #2).
They had a total knee replacement (TKR). What impact could that surgery have on their vital signs? How might that information influence your treatment? We will come back to that in a bit.
PART I:
STANDARD VITAL SIGNS
The following are the vital signs that we will be measuring, monitoring and discussing:
- Body temperature
- Pulse
- Blood pressure
- Respiration (and Pulse Oximetry)
- Pain
We will need to know the physiological significance each as well as the normal values and possible causes for changes to the normal values. Let’s start with:
SIGNIFICANCE and NORMAL VALUES
BODY TEMPERATURE: Our normal body temperature is regulated by the hypothalamus. One of the many jobs of the hypothalamus is thermoregulation: the process of keeping the body temperature in a range between 99.7 – 99.5 degrees Fahrenheit despite the outside temperature. While 98.6 degrees is considered ‘normal’, individuals can vary a few degrees lower.
If you check your own temperature (at the same time of the day) for a week or so, you will get an idea of your normal temperature. If you do this three times a day (and are consistent with the days of day), you may see that it is lower in the morning and higher later in the day. When our bodies are responding to infection, illness, trauma or a host of other factors, an increase or decrease in our temperature may occur.
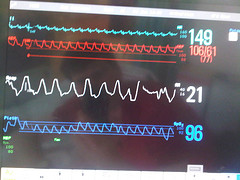
HEART RATE: Often referred to as our pulse or pulse rate, the speed of our heartbeat is measured by the number of contractions (beats) of the heart per minute (beats per minute or bpm). Our pulse, or heart rate, is an essential vital sign to monitor in virtually all of our patients; young or old, healthy or ill. It allows us to measure, objectively, how the patient is responding to their illness or injury as well as to activity. That is because our heart rate will respond to our body’s need for more oxygen: A demand that may come from a great many sources. We will note those shortly.
Accordingly to the American Heart Association:
The normal resting heart rate for an adult: 60–100 bpm.
The normal resting heart rate for a child: 80 – 120 bpm.
**Please put these heart rates to memory.
The term “tachycardia” is used when the RESTING heart rate is above the upper limit of ‘normal’. So, a RESTING heart rate of over 100 bpm (…while at rest) is considered tachycardic. You will see the prefix “tachy” used in other areas; again, it will mean ‘rapid, above normal’.
On the other end of the spectrum we have braycardia which refers to a slow RESTING heart rate. We will use the term bradycardia for a RESTING heart rate (…while at rest) that is below 60 bpm. If our patient has a resting heart rate of 52, we would say they are “bradycardic”. As with ‘tachy’, ‘brady’ is a term used to describe ‘slow, below normal’.
To note, you will encounter many types of rates when you are a clinician. Below are some descriptors that will match the type of rhythm and rates you will be monitoring. Of the ones we will discuss, special care is given to cases when the heart is not beating in a regular pattern: this is referred to as an arrhythmia. Arrhythmias (noted as “irregular” below) can be benign (harmless) or dangerous. You will learn more about that range next year. For now, appreciate that arrhythmias, or other abnormal heart rate responses, may sometimes indicate heart disease.
Pulse Descriptors:
- Strong and Regular : Each heartbeat is clearly felt
- Weak and Regular: Each heartbeat is clearly felt, but a bit faint.
- Irregular: An irregular heartbeat can actually have a regular pattern (skips every third beat, for example) or an irregular pattern (skips randomly). So we note it as: Regularly irregular or irregularly irregular.
- Thready: Note this descriptor when the heartbeats are not distinct; individual heartbeats hard to discern.
- Tachycardia: Greater than 100 bpm at rest.
- Bradycardia: Less than 60 bpm at rest
Pulse Measurement Sites:
We will perform pulse checks on ourselves and/or our lab partners on the highlighted pulse points.
Please check out this short video regarding the basics of taking someone’s pulse. It is short and a bit entertaining. It will help you prepare for class.
How to monitor and record the Radial Pulse
- Temporal
- Carotid
- Brachial
- Radial
- Femoral
- Popliteal
- Posterior Tibial
- Dorsal Pedal
- Apical
Review this image (This is a Creative Commons Attribution 3.0 Unported license image)

BLOOD PRESSURE: When we measure a patient’s blood pressure we are indirectly measuring the pressure inside their arteries. In other words, the pressure of their circulating blood against the walls of their blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. Blood pressure is reported in terms of the systolic pressure “over” the diastolic pressure in millimeters of mercury (mmHg) above the surrounding atmospheric pressure. If you remember from our key terms, systole refers to the contract of the ventricle so systolic pressure is the pressure at the time of the contraction of the ventricle. Diastole refers to the relaxation phase of the heart; when the ventricles are re-filling. So, the diastolic pressure refers to the pressure during the time of rest between contractions. This is a very important phase of our heartbeat.
If the left ventricle does not relax sufficiently, as noted by an elevated blood pressure reading (the diastolic number will be above the ‘normal’ value), the heart undergoes stress. You may be thinking that, well, isn’t the heart a muscle. And right you are. You may then think, well, won’t it just get bigger and stronger like my biceps get when I go to the gym. Again, you are right – but here’s the catch. The larger the left ventricle gets, the smaller its inside volume. Consequently, that ventricle begins to pump less and less blood out (referred to as stroke volume) with each pump.
So, what happens next?
Right, the heart must pump more often and with more force to supply the body with the blood it needs. This leads to what?
Again, you are right: More hypertrophy of that left ventricle. This is a cycle we do not want anyone to be in, but unfortunately, many of our patients will be in. That is enough pathophysiology for now😊
Normal Ranges:
Normal resting blood pressure, in an adult is approximately 120 millimeters of mercury systolic over 80 millimeters of mercury diastolic: but you and I would just report this as: “120/80”.
Blood Pressure: Normal Ranges
| ADULT RANGES: | SYSTOLIC | DIASTOLIC |
|---|---|---|
| Normal | 100 – 120 | 60 – 80 |
| Pre-HTN | 120 – 139 | 80 – 89 |
| Stage 1 HTN | 140 – 159 | 90 – 99 |
| Stage 2 HTN | 160 – 179 | 100 - 109 |
We will note the factors that can influence our blood pressure shortly. For now, it is important to note that when blood pressure falls out of its normal range, it will impact the body. Something we need to be keenly aware of as clinicians.
We have noted that elevated diastolic blood pressure may lead to hypertrophy of the left ventricle. However, if our blood pressure is too low or drops when we move about, that can be a problem too.
When the blood pressure that is below the normal values, we call it hypotension. Individuals with hypotension are especially at risk to become dizzy or lightheaded when they change position, first stand up or move too quickly. Even bed mobility activities may elicit a sense of dizziness. This probably doesn’t surprise you.
However, even individuals with blood pressure that is within the normal limits (WNL) at rest may experiences a sudden drop in blood pressure when they stand up. This is especially true if they are taking medications for blood pressure control or pain. We call this sudden drop in blood pressure that is related to a change in position as orthostatic hypotension. The patient will feel a bit woozy and may report they need to sit down or that they feel faint. Technically, we say someone is orthostatic when they experience a drop of 20 mmHg from their systolic blood pressure and a drop of 10 mmHg from their diastolic. However, even if a patient’s drop-in blood pressure is not that significant, if they report feeling lightheaded upon rising, we need to report it and document it.
And just to circle back with a final note on hypertension. To be sure, there are any number of factors that may, temporarily, raise someone’s blood pressure (scary movie, exciting sporting event, good news, bad news, etc.). Hypertension, however, refers to blood pressure that stays at that elevated level and is not just situational. Long-term hypertension increases the risk for many diseases, including heart disease, stroke and kidney failure.
Taking a Patient’s Blood Pressure:
We will be performing all aspects of learning how to take a blood pressure in lab. You will need to have viewed this video beforehand. It is short, clear and a lovely example of to take a blood pressure.
Korotkoff’s Sounds
- First faint, clear tapping. Systolic Reading.
- Murmur-like sounds
- Clear and crisp
- Abrupt muffling
- Sound disappears. Diastolic number.
RESPIRATION RATE: A person’s respiratory rate is the number of breaths they take per minute.
The normal respiration rate for an adult at rest is 12 to 20 breaths per minute. A respiration rate under 12 or over 25 breaths per minute while resting is considered abnormal. If a patient was breathing at a rate of 25 breaths per minute at rest this would be considered tachypnea. If a patient was breathing at a rate of 8 breaths per minute, this would be considered ___________ pnea.
Pulse Oximetry: The purpose of pulse oximetry is to check how well the heart is pumping oxygen through the body. It may be used to monitor the health of individuals with any type of condition that can affect blood oxygen levels as well as
- To monitor oxygen levels during or after surgical procedures that require sedation
- To determine how effective supplemental oxygen therapy is, especially when treatment is new
- To assess someone’s ability to tolerate increased physical activity
- To evaluate whether someone momentarily stops breathing while sleeping — like in cases of sleep apnea — during a sleep study
Pulse oximetry works by placing a small clamp-like instrument on the patient’s finger, earlobe, or toe. Small beams of light pass through the blood in the finger, measuring the amount of oxygen. It does this by measuring changes of light absorption in oxygenated or deoxygenated blood. This is a painless and very easy procedure. Most, if not all pulse oximeters, will also display the individual’s heart rate as well.
NORMAL VALUE: 95 – 100%. When it is below 90%, we do not perform exercise with our patient.
Note: It can be difficult, however, to get readings from patient’s with cold fingers. More on this in our lab.
RESPIRATION ASSESSMENT:
In addition to the rate of respiration, we also note:
How to monitor Respiration Rate:
Please view this very short, but clear, video. You will be replicating this skill in lab.
How to Monitor Respiration Rate
PAIN RATING AND RELATED FACTORS
For our purposes here in PT100S, we will just be overviewing the basics of pain assessment. This is a rather large topic, far greater than you may imagine. However, for now, we will just focus on:
Pain Location (s): Often, when pain is strong enough, it will radiate to other body parts. We need to ask questions to determine where the epicenter of the pain is as well as where it radiates to when it is ‘bad’.
Pain Range: We will be asking our patient’s subjectively to report their pain range from 0 – 10 with 10 being the worst imaginable pain.
Pain Variation: We will ask our patient when their pain is at its worst and when is its at its least. We will pay attention to the positions and activities described in their answer as well as the role of medications and time of day.
PART II: POSSIBLE CAUSES OF CHANGES TO NORMAL VALUES:
You will hear us (your instructors) that you are not “technicians”, but “clinicians”. We say this meaning that your job is not to ‘blindly’ put your patient through the given exercises, gait activities or modalities, but rather to always be using your best clinical judgment in applying your interventions.
As PTAs, you are required to always be monitoring your patient’s status and performance – so you can adapt, modify or discontinue an intervention.
- Part of that monitoring process incudes, of course, monitoring vital signs.
- Part of monitoring vital signs is knowing their normal values.
- Part of monitoring vital signs includes understanding what may cause a given vital sign to be outside of the normal range. Later in the PTA Program we will discuss more deeply how we manage the array of aberrations (deviations from the normal) that you will encounter. For now, let’s just offer possible reasons a vital sign may not be WNLs.
FACTORS AFFECTING BODY TEMPERATURE:
TERMS for temperature aberrations:
FACTORS: Temperature aberrations
- Time of Day: Typically, lower in the am; higher during the day.
- Age: May be slightly higher with stages of life associated with higher metabolism
- Infection: Typically elevates our temperature
- Physical Activity: Will increase our core body temperature
- Emotional status: Depends on the emotion and the individual. Strong emotions such as anger, anxiety or frustration may increase body temperature whereas chronic depression may lower it.
- Site of measurement: Oral verses rectal verse axilla.
- Menstrual cycle
- Pain: Acute pain will often increase body temperature; chronic pain may, but tends to
Have less of an impact of body temperature. - Physical or Emotional Trauma: Will cause an increase. Post-surgical patients tend to run a low-grade fever the first few nights after a surgery.
- Oral Cavity Temperature: For an accurate temperature reading, one should not eat or drink
for 30 minutes prior to taking one’s temperature with an oral thermometer. - Environmental Temperature: Fairly obvious here, right?
FACTORS AFFECTING HEART RATE:
- Age: Normal Values:
- Infants (6 – 12 months old): 80 – 120 beats per minute.
- Children 1 – 10 years: 70 – 130 beats per minute.
- Children over 10, adults 60 – 100 beats per minute.
- Well-trained athletes: 40 – 60 beats per minute.
- Gender: Females tend to run higher than men.
- Environmental Temperature: Higher temperatures tend to increase heart rate (especially for those with heart disease)
- Infection: Tends to increase resting heart rate as well heart with activity
- Physical Activity: No surprise;
- Emotional Status:
- Medications:
- Cardiopulmonary disease:
- Physical Conditioning: One of the benefits
ABNORMAL RESPONSES EXHIBITED BY PULSE:
- Increases slowly with activity
- Does not increase with activity
- Continues to increase/decrease as exercise plateaus
- Slowly declines after activity seizes
- Does not decline after activity seizes
- Declines before activity seizes
- Increases beyond expected level
- Becomes irregular: Dysrhythmias.
FACTORS AFFECTING BLOOD PRESSURE:
- Age: Tends to rise over the lifespan
- Physical Activity: A normal response would be an increase in the systolic pressure with minimal change to the diastolic pressure. An increase of greater than 10mmHg with the diastolic reading is cause to terminate an exercise session.
- Emotional Status:
- Medications: Many medications impact blood pressure; most decreasing it, but some (like those for breathing impairments) increase it.
- Artery Integrity: With age, our vessels are less efficient ‘pushing’ the blood through our bodies causing the heart to pump harder to get the blood circulated.
- Arm position: We may get an inaccurate reading if the arm is above or below the level of the heart.
- Blood volume: When our blood volume decreases, so does our blood pressure.
- Dehydration: Causes a decrease in blood pressure.
- Impaired cardiac output: Causes an increase in blood pressure.
- Site of Measurement (left > right): It is not uncommon for individuals to have different readings between their arms.
ABNORMAL Responses of Blood Pressure
- Systolic rise to rapid with activity
- Systolic does not rise with activity
- Systolic increases / decreases after activity plateaus
- Systolic decline is too rapid after exercise seizes
- Systolic does not decrease after activity seizes
- Systolic declines below baseline after activity
- Systolic declines before activity declines
- Systolic rise is excessive for the activity
- Diastolic rise > 10 – 15 mm Hg during activity
FACTORS AFFECTING RESPIRATION:
- Age:
- Adults: 12–18 breaths per minute.
- Elderly ≥ 65 years old: 12–28 breaths per minute.
- Elderly ≥ 80 years old: 10-30 breaths per minute.
- . Physical Activity: Increases to supply the demand of 02 to the body.
- Emotional Status: Increases during periods of stress
- Air Quality: As the amount of 02 in the ‘air’ decreases, the respiration rate increases.
- Altitude: As the amount of 02 in the ‘air’ decreases, the respiration rate increases.
- Disease: Often results in labored and/or inefficient breathing.
ABNORMAL Responses of RESPIRATORY RATE (RR)
- RR increases too slow for activity
- RR does not increase for activity
- RR increases after plateau
- RR decreases too slowly after activity seizes
- RR does not decline after activity seizes
- RR decreases prior to activity terminating
- RR is excessive for given activity
- Irregular rhythm
REFLECTION II (Please complete and bring to lab this week)
Now, let’s return to you patient who has just had a right TKR surgery ago:
They are s/p (status post) RTKR POD2. You are seeing them for treatment in a rehab hospital setting. They are in a wheelchair ready for you to begin your care. They tell you their knee hurts “like crazy” (8/10) and that they are really scared to start this “physical therapy stuff”.
-
- How to you introduce yourself?
- What do you check on their wheelchair?
- Before you begin care, you need to check their vital signs. Can you list what impact that surgery may have had on the following vital signs?
- Body temperature:
- Pulse:
- Blood pressure:
- Respiration:
- Pain:
- You check your patient’s heart rate and find it is 104 bpm:
- What is the term for that rate?
- What is the normal range for a resting heart rate?
- Your patient’s blood pressure is 140/85
- The term for this low reading is:
- After your talk to your patient to reassure them you won’t hurt them, you re-check their blood pressure and find it to be 125/80 and that is considered WNL.
WNL is an abbreviation for: - When your patient stands up to begin their gait training, they become lightheaded. Why might this be and what is the term for this phenomenon
- ___
- You are monitoring your patient’s heart rate. You count 28 beats in a 30 second period of time.
- What is the patient’s pulse rate?
- What is the term we use for that type of rate?
- What effect would a hot environment have on a patient’s heart rate if the patient had heart disease?
- ___
- What effect could dehydration have on a patient’s blood pressure?
- ___
- You have just completed your treatment with your patient. They are feeling great. They tell you they are far less anxious than when they arrived earlier. Their pain is much better (it is just a 2/10 now) and they are really happy to come back to see you. How might these factors influence their:
- Blood pressure:
- Heart Rate:
No heartbeat
The relaxation phase of the heartbeat: The ventricles fill with blood
A sustained elevation in resting blood pressure (HTN)
A condition of low resting blood pressure
A condition in which one cannot breathe efficiently unless upright.
A unfavorable drop in blood pressure related to position change
Measures the percentage of 02 saturationin the blood
Instrument to measure blood pressure
Loss of consciousness; fainting
The contraction phase of the heart: The ventricle pump out the blood filled during the diastole period.
Temperature, Heart Rate, Respiration Rate, Blood Pressure and Pain
co-existing illnesses
Is the breathing smooth or is it arrhythmic
Are the breaths full or shallow
Are the breaths labored: Does the patient wheeze or struggle to breathe?
Thoracic verse abdominal breathing. The latter is highly desirable and indicates that the individual is breathing through the use of their primary muscle of inspiration: The diaphragm.
A temperature of 100 degrees Fahrenheit (F) or greater
A temperature of 106 degrees (F) or greater
A temperature below 95 degrees F

