17 Chapter 07 – Lecture Unit 7: Cardiopulmonary Conditions
Cardiopulmonary Conditions
Link to visit the Cardiopulmonary Conditions Chapter
Welcome to another scavenger hunt!
This week, we will be searching through your pathophysiology OER Text to seek out terms and concepts related to cardiopulmonary conditions. As we did last week, there will be activities along the way for you to complete to reinforce your learning. Your knowledge of cardiopulmonary conditions will be crucial for your success in the clinic as well as in this PTA Program and when you take your licensure exam.
Let’s begin by looking at a schematic of cardiac circulation (below). Please take a moment now, before we begin, to review the circulation of blood through the heart. You will want to know this chart cold; so you can draw this chart from memory. This will greatly enhance your understanding of the pathologies that might befall the heart.
Insert The heart square image drag and drop?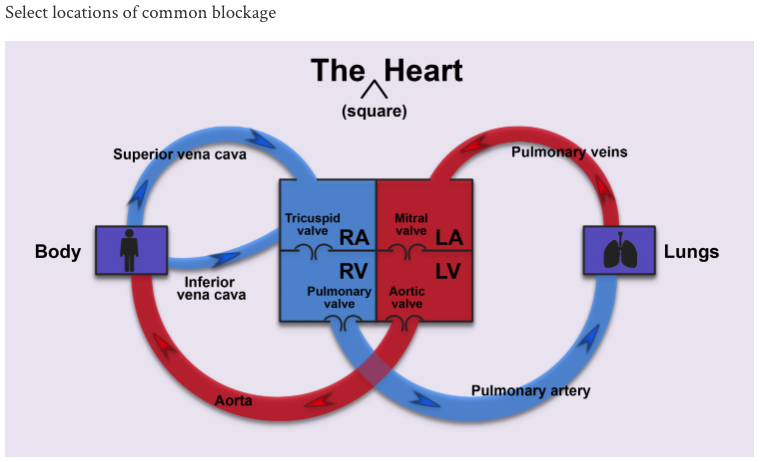
Select locations of common blockage
h5p id=”14″ from renee’s oer?
Earlier this semester, we looked at vital signs. At that time, we noted the monitoring vital signs is crucial during patient care. Do you remember why? Well, we noted that being aware of our patient’s vital signs before treatment allows us to know if the patient is ‘safe enough’ and/or appropriate for PT. For example, would a patient with a resting heart rate of 64 bpm be safe for treatment? Hmm.
Well, yes indeed as that heart rate is WNL. However, if the resting heartrate was 120, well, now we have an issue requiring immediate follow up with your Clinical Instructor or supervising PT. We can say the same for all of the other vital signs (pain, respiration rate, blood pressure and temperature). Likewise, our post-treatment assessment of vital signs allows us to know if the patient’s response to our treatment was WNL (favorable) or outside of the normal limits (and unfavorable).
It is this unfavorable response that we want to be especially careful managing as unfavorable cardiopulmonary responses could lead to terrible patient consequences. For example:
Worldwide there are 32,000,000 myocardial infarctions and CVAs annually. In the US, we have 1,500,000 heart attacks/year. Another way to say it is that someone in the US will have a heart attack every 40 seconds. Wow, huh?
Not only do we need to protect our patients from having a heart attack (MI) during our treatment, but we also need them to understand how they can be part of the heart attack prevention-process. To meet these two goals for our two roles: therapist and educator, we need to develop our understanding of the heart and its pathologies’.
First, to clarify: Coronary artery disease (CAD) is responsible for 50% of all deaths caused by Cardiovascular disease. CAD is a disease of the coronary arteries d/t plaque buildup on the inner walls of arteries.
This plaque causes the arterial lumen, through which blood flows, to narrow. As plaque builds up in one area, a clot (thrombus) is formed. When a thrombus is in the coronary arteries it impairs the blood supply to that area of myocardium. As the blood supply decreases (ischemia), oxygen supply decreases (anoxia), and the heart muscle becomes less able to contract
Angina pectoris and myocardial infarction may be the result.
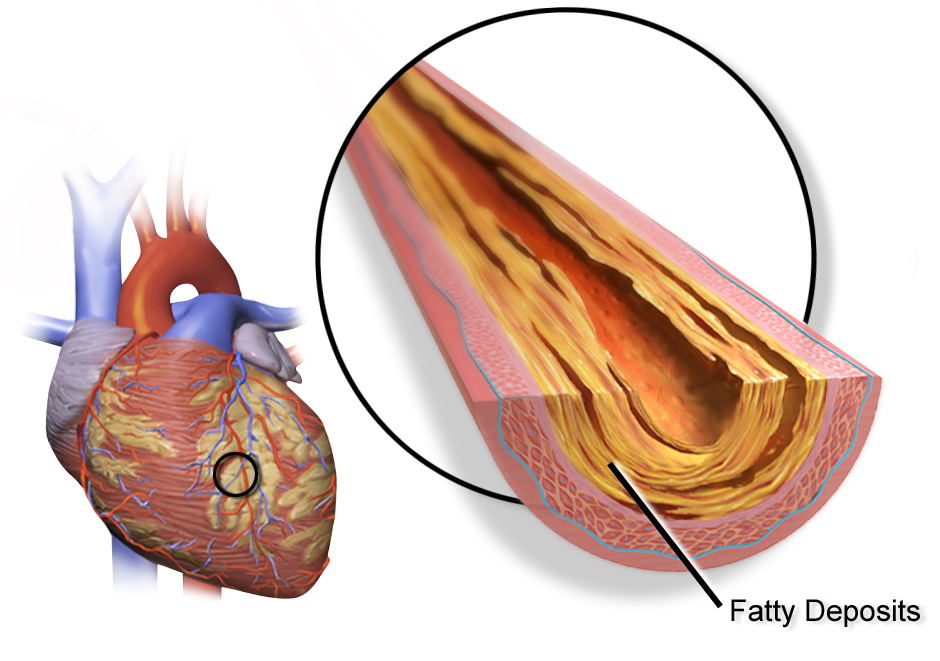 Fatty Deposits – “File:Blausen 0257 CoronaryArtery Plaque.png” by BruceBlaus, Blausen.com is licensed under CC BY 3.0
Fatty Deposits – “File:Blausen 0257 CoronaryArtery Plaque.png” by BruceBlaus, Blausen.com is licensed under CC BY 3.0
The risk factors for CAD fall into two categories:
- Those we cannot change (Immutable).
- Those we can change (mutable)
IMMUTABLE
- Age
- Gender
- Ethnicity/ Heredity
MUTABLE
- Smoking
- Obesity
- Diet
- Exercise
- Sleep
- Blood Pressure
- Diabetes
- Cholesterol Levels
- Stress
- Alcohol Use
As we work to educate our patient, our knowledge of these risk factors can help us provide strategies to our patients that may lower their risk for CAD or for a second MI.
Time to visit your pathophysiology book: Please use the link above to find the answers to the following (10) questions:
_________________________________________________
_________________________________________________
_________________________________________________
Reflect: What are some of the warning signs (“red flags”) that would alert a PTA to stop or modify PT interventions with patients with CHF?
_________________________________________________
_________________________________________________
_________________________________________________
Pulmonary (Respiratory) Conditions
Link to the chapter in the Patho OER…
TERMINOLOGY AND CONCEPTS:
When we hear the word ‘cardiopulmonary’ it is easy to just focus on the cardio part. However, pulmonary disease, specifically lower respiratory pulmonary diseases, are the third leading cause of death in the US. Wow: The third leading cause. Sound important, does it not?
General signs of pulmonary system condition or disease
- Sneeze: irritation or inflammation of nasal passages
- Cough:
- Irritation due to nasal discharge
- Inflammation, foreign material, or tumor in lower respiratory tract
- Effectiveness is determined by strength of respiratory muscles
- Productive or unproductive
- Hemoptysis
- Dyspnea: Subjective feeling in which the patient feel unable to inhale enough air
- Orthopnea: dyspnea in supine
- Tachypnea: breathing at a faster rate than expected
- Bradypnea: breathing at a slower rate than expected
- Chest pain: may radiate to shoulder or arm
- Cyanosis
- Central: mucous membranes of mouth, lips
- Peripheral: nail beds, nose, ends of fingers, toes
- Altered or irregular breathing patterns
- Clubbing of fingernails: shape of nailbed changes; angle is decreased; seen in pulmonary and cardiovascular disorders
study
Conduction of Airways:
The Upper and Lower Respiratory Systems
Upper
- Nose
- Pharynx
- larynx
Lower
- Trachea
- Bronchiole System:
- Tubes that branch out from the main bronchus and become the bronchiole trees which are where the Alveoli exist.
- Alveolus: where gas exchange occurs: Os and CO2 enchanged. Re-oxygenated blood going back to the left atria.
DISEASE:
In general, there are either obstructive or restrictive pulmonary diseases.
- OBSTRUCTIVE Diseases are pathologies that cause
-
- An ABNORMALITY IN AIRFLOW through the bronchial tubes.
OBSTRUCTIVE — COPD.
Symptoms:
- Chronic productive cough.
- Excessive mucous production.
- Dyspnea
As the disease progresses, it results in Hypoxemia: Decreased O2 in blood.
Disorders:
- Chronic bronchitis
- Emphysema
- Asthma
- Cystic fibrosis
CHRONIC HYPOXEMIA results in cardiac and BP changes and the ‘Thichness’ of the blood. Eventually, respiratory failure
- RESTRICTIVE: Pathological changes that cause
-
- The VOLUME OF AIR IN THE LUNGS to be reduced.
RESTRICTIVE Lung Disease:
Diseases that cause a decrease in the ability of the lungs to expand.
Etiology
- Idiopathic
- Chronic inhalation of air pollutants / coal dust
- Infections: pneumonia, Lung CA, Cardiac function changes
- Diseases / trauma
Signs / Symptoms
- SOB / dyspnea
- Chronic, non-productive cough
- TACHYPNEA – resulting in excessive use of accessory muscles of respiration and excessive energy expenditure – results in weight loss.
SHORTNESS OF BREATH
Shortness of breath: A key feature for both Obstructive and Restrictive Lung Disease. However, the causes are different. As a PTA, you need to know these key differences and the rationale (pathophysiology) for each.
In Obstructive Disease: The bronchi are narrowed and obstructed by excessive mucus. This means it takes a longer time to exhale than it does to inhale. The narrower the bronchi and the more obstructed they are, the longer it takes to exhale.
Restrictive Lung Disease: Restrictive lung disease decreases the ability to expand the lungs making it difficult to fully inhale.
PRACTICE: There are 2 multiple choice Questions in this practice quiz.

