Chapter 6: The Cardiovascular System
Learning Objectives
After completing this chapter, the student should be able to:
- 1. Identify data collection techniques regarding cardiovascular functioning, particularly those commonly used by PTAs.
- 2. Review the blood flow through the heart, coronary circulation, and the conduction system of the heart.
- 3. Discuss risk factors for Diseases and Conditions Affecting the Heart and General Circulation
- 4. Discuss heart failure: causes, effects, basics of disruption in filling and pumping mechanisms.
- Systolic vs diastolic
- Left-sided vs right-sided
- 5. Discuss cardiac circulation, coronary artery disease, angina pectoris, and myocardial infarction.
- 6. Discuss conditions affecting cardiac conduction.
- Arrhythmia
- 7. Discuss conditions affecting the blood vessels.
- Hypertension
- Atherosclerosis and arteriosclerosis
- Peripheral vascular disease
- Deep venous thrombosis and phlebitis
- Aneurysm
- 8.Describe the mechanism of dysfunction and results of the congenital conditions:
- ASD
- VSD
- Tetralogy of Fallot
- Transposition of the Great Vessels
- 9. Describe the mechanism of dysfunction and results of Cardiomyopathy
- 10. List several drugs commonly used to treat various cardiovascular conditions, and describe possible side effects.
- 11. List common surgical procedures for cardiovascular disorders and post-operative recovery concerns.
- 12. Discuss the role of the PTA in the medical and post-operative treatment of patients with cardiovascular conditions.
Chapter Contents
- 6.0 Introduction to Cardiovascular Conditions
- 6.1 Review of Blood Flow Through the Heart
- 6.2 Data Collection Techniques
- 6.3 Risk Factors for Diseases and Conditions Affecting the Heart and General Circulation
- 6.4 General Signs and Symptoms of Cardiac Problems
- 6.5 Heart Failure
- 6.6 Cardiac Circulation
- 6.7 Coronary Artery Disease and Related Disorders
- 6.8 Cardiac Conduction, Arrhythmia/Dysrhythmia
- 6.9 Disorders Affecting the Blood Vessels
- 6.10 Congenital Conditions of the Heart
- 6.10.1 Atrial Septal Defect
- 6.10.2 Ventricular Septal Defect
- 6.10.3 Tetralogy of Fallot
- 6.10.4 Transposition of the Great Arteries
- 6.11 Cardiomyopathy
- 6.12 Mediations Used to Treat Disorders of the Heart and Blood Vessels
- 6.12.1 Angiotensin-converting enzyme (ACE) inhibitors
- 6.12.2 Angiotensin-2 Receptor Blockers
- 6.12.3 Anticoagulants
- 6.12.4 Antiplatelet (Antithrombotic) Agents
- 6.12.5 Beta Blockers
- 6.12.6 Calcium Channel Blockers
- 6.12.7 Cholesterol-Lowering (Antihyperlipidemia) Medications
- 6.12.8 Diuretics
- 6.12.9 Digitalis Preparations (Positive Inotropic Agents)
- 6.12.10 Vasodilators
- 6.12.11 Immunosuppressive Medications
- 6.13 The PTA and Cardiovascular Conditions
6.0 Introduction to Cardiovascular Conditions
6.1 Review of Blood flow through the heart
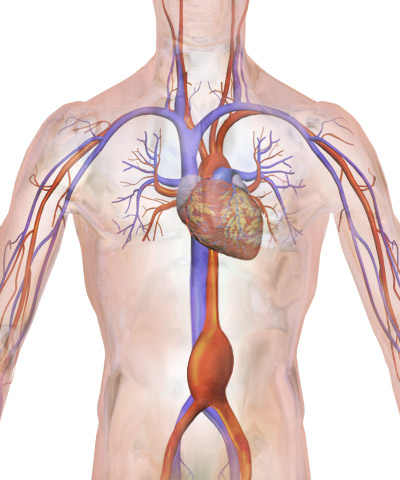
- Deoxygenated blood returns to the heart from the superior and inferior venae cavae and enters the right atrium.
- From the right atrium, it flows through the tricuspid valve into the right ventricle.
- From the right ventricle, it flows through the pulmonary valve and out of the heart through the pulmonary arteries.
- The pulmonary arteries carry the blood to the lungs, where they give up CO2 and pick up O2.
- The pulmonary veins carry oxygenated blood back to the heart.
- The oxygenated blood enters the left atrium.
- From the left atrium, the blood flows through the mitral valve and into the left ventricle.
- From the left ventricle, the blood flows through the aortic valve, into the aorta, and out to the body.
Blood flow through the heart is achieved through the pumping mechanism of the contraction and relaxation of cardiac musculature and pressure gradients between the chambers of the heart. The blood always flows from an area of greater pressure to an area of lower pressure.
A simpler diagram to help understand blood flow is below. You should remember it and be able to recreate it. This picture will be helpful as you consider areas of the heart that are damaged, blocked or malfunctioning.
6.2 Data Collection Techniques
- Heart rate (HR): pulse taken, most often taken at radial artery in wrist; can also be taken over other arteries, as shown:
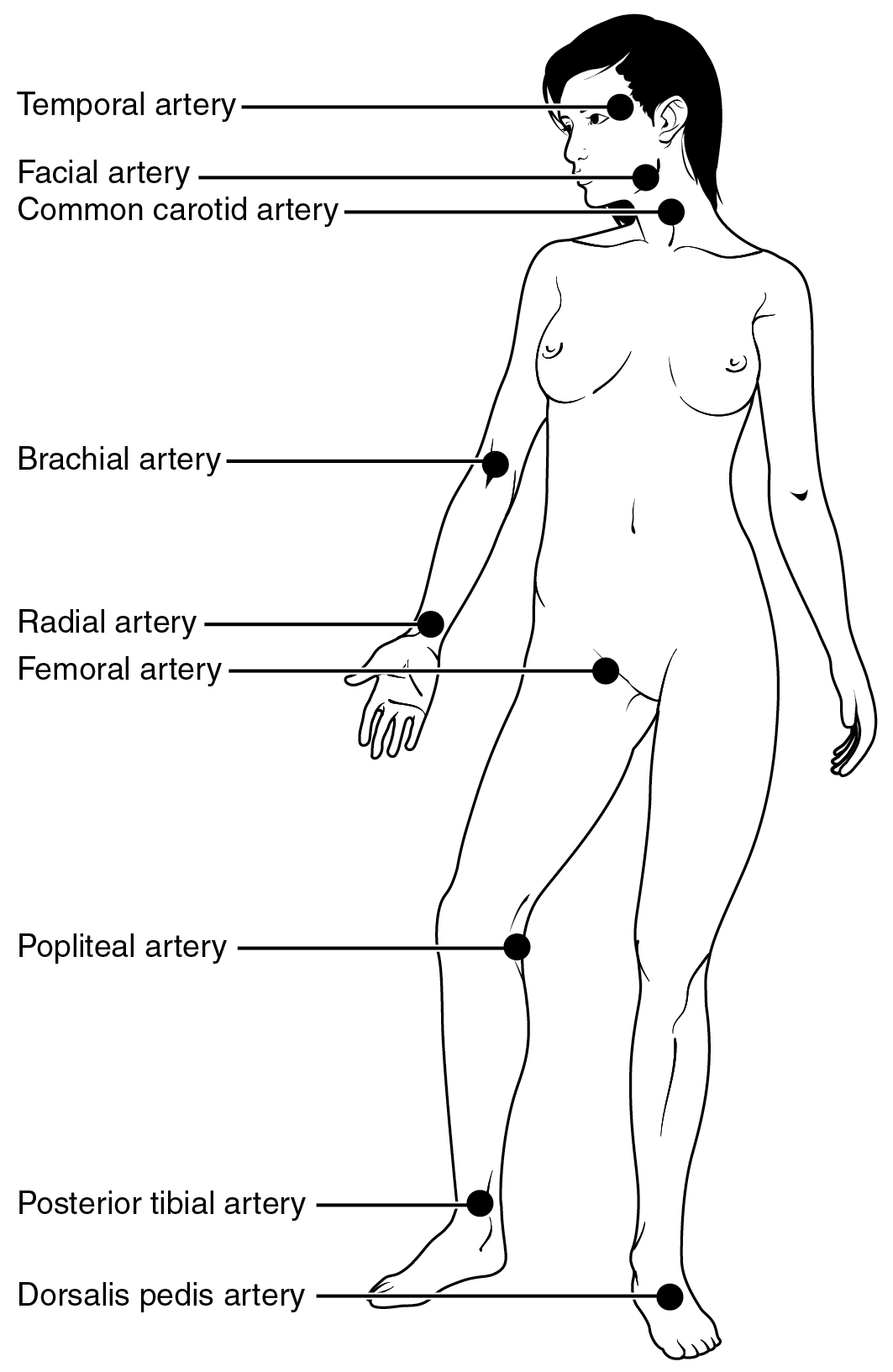
Heart Rate Pulse Sites, OpenStax College, CC BY 3.0, via Wikimedia Commons Long Description
Pulse sites
- Temporal artery (Temple)
- Facial artery (Side of chin)
- Common carotid artery (Neck)
- Brachial artery (Elbow)
- Radial artery (Wrist)
- Femoral artery (Groin)
- Popliteal artery (Back of knee)
- Posterior tibial artery (Ankle)
- Dorsalis pedis artery (Top of foot)
- Normal rate for adults: 60-100 bpm
Normal rate for small children is much higher:- Newborns 100-165 bpm;
- 2 year olds: 70-110 bpm;
- 10 year olds: 60-95 bpm
- Blood pressure (BP): most often taken using a sphygmomanometer and stethoscope over the brachial artery; automatic blood pressure monitors also provide an accurate measure of blood pressure; can be taken over the femoral artery in the lower extremity
- Normal for adults: systolic 90-120 mmHg; diastolic 60-80mmHg
- Normal for children is lower than for adults
- Oxygen saturation: most common tool for test is pulse oximeter
- Normal rates for SpO2: 95-100%
- Auscultation: listen for heart sounds, most often with a stethoscope: “lub-dub” is normal. “Whoosh” could mean a defect in the septum between the right and left sides of the heart or a problem with a cardiac valve.
- Rate of Perceived Exertion (RPE) scale: subjective self-assessment that measures rate of perceived exertion (RPE)
-
-
- 6-20 is original Borg scale
- numbers correlate to heart rate; RPE value x 10 = approximate heart rate; so if a patient reports their RPE is “9,” their heart rate is likely around 90 beats per minute
6.2 – Resource 02 – Level of perceived exertion scale
Original RPE Scale Number Original RPE Scale 6 No exertion 7 Very, very light 8 – 9 Very light 10 – 11 Light 12 – 13 Somewhat hard 14 – 15 Hard (heavy) 16 – 17 Very hard 18 – 19 Extremely hard 20 Maximal Revised RPE Scale Number Revised RPE Scale 0 Nothing at all 0.5 Very, very weak 1 – 2 Very weak 3 – 4 Somewhat strong 5 Strong 6 – 7 Very strong 8 – 9 – 10 Very very strong – – – – – –
- numbers correlate to heart rate; RPE value x 10 = approximate heart rate; so if a patient reports their RPE is “9,” their heart rate is likely around 90 beats per minute
- 6-20 is original Borg scale
-
-
- Body weight: sudden increase in body weight can mean fluid retention associated with congestive heart failure. More than 2-3 lbs. in a day or 5 lbs. in a week is suggestive of worsening heart failure
- Chest radiography (x-ray): used to visualize heart, blood vessels, lungs, airways, ribs, bones of chest and spine. Contrast dyes may be used to improve imaging.
- Cardiac catheterization: narrow, flexible tubing that is inserted in the groin area or upper arm through the venous system and into the heart. Used for insertion of dye to visualize blockages or narrowing of blood vessels when combined with diagnostic imaging (x-ray, sonogram). Catheters can also be used to take blood samples or to perform surgeries inside the heart.
- Electrocardiogram (EKG or ECG): monitors the electrical activity of the heart. Can help diagnose arrhythmia, myocardial infarction.
- Echocardiogram: ultrasound that can help diagnose problems with the valves or muscle of the heart because it is able to show the movement of the heart and its structures.
- Magnetic Resonance Imaging (MRI): uses magnetic waves to obtain clear pictures of the heart and its inner chambers.
- Arterial blood gas (ABG): determine amounts of oxygen and carbon dioxide in the blood, and quantify the pH of the blood (normal range for pH: 7.35-7.45).
- 6-Minute Walk Test/ 3-Minute Walk Test: patient walks as far as they are able in 6 minutes/ 3-minutes; tester records distance walked.
- Exercise stress test: ECG, HR, BP and symptoms are monitored while patient is exercising.
Test Your Knowledge
- Which of the above data collection techniques are PTAs able to perform in the clinic?
- Why would a PTA be interested in the information obtained by these tests?
- How might a PTA alter a patient’s treatment session, depending upon findings from these tests? Give at least 2 examples.
- If a PTA is performing gait training activities with a patient in the early stages of a cardiac rehabilitation program, and they report an RPE of 15 on the Borg scale, what should the next steps be for the PTA?
6.3 Risk Factors for Diseases and Conditions Affecting the Heart and General Circulation
There are many disorders of the cardiovascular system described below. In general, except for congenital heart conditions, most cardiovascular disorders share a common list of risk factors. These risk factors can be placed in one of two categories: non-modifiable and modifiable.
Non-Modifiable Risk Factors
- Age
- Gender
- Ethnicity/ Heredity
Modifiable Risk Factors
- Smoking
- Obesity
- Diet
- Exercise
- Sleep
- Blood Pressure
- Diabetes
- Cholesterol Levels
- Stress
- Alcohol Use
6.3 – Resource 01 – Risk factors for cardiovascular disorders table
6.3.1 Non-Modifiable Risk Factors
Age: The risk of heart disease increases with age. Since heart disease is highly associated with atherosclerosis, which starts in the second decade of life, it seems likely that the groundwork for heart disease is laid many decades before most Americans experience symptoms.
Gender: Both men and women are at risk for developing heart disease. One in three men and one in three women will die from heart disease, which is the most common cause of death among all people in the United States (NIH, CDC). Premenopausal women are at a lesser risk than are menopausal and postmenopausal women, who are at equal risk with men of the same age.
Ethnicity and Hereditary factors: There are some genetic conditions that cause people to maintain high LDL levels and low HDL levels, and, without medical intervention, these people are at risk for heart attacks and death at an early age. There may be other familial conditions that put a person at risk, but it is very difficult to identify true genetic links from cultural diets and activities. Hypertension, coronary artery disease, and heart failure are more common in African-Americans, Hispanic-Americans, and Native Americans than in Caucasians or Asians.
6.3.2 Modifiable Risk Factors
Smoking: The chemicals in smoke damage the insides of the blood vessels. The damaged areas attract fatty deposits, platelets, and other particles from the blood. This decreases the lumen size of the vessels and makes the vessels stiff, causing greater peripheral resistance for the heart to pump against. Also, smoking damages the respiratory system, which is closely tied to the cardiovascular system.
Obesity: Obesity is defined as a body mass index (BMI) or 30 or greater. About 1/3 of American adults are obese by this standard and are at risk for cardiovascular disease and other health issues such as diabetes, and high levels of cholesterol and triglycerides. Also, increased body mass creates more work for the heart. All of these are closely related to cardiovascular status.
Diet: It is recommended that people with many forms of heart disease decrease sodium and add potassium to their diets. This is especially true in the case of hypertension. Sodium attracts water, so extra sodium in the blood pulls water from the interstitial spaces into the blood stream. This increases blood volume, causing greater pressure inside the blood vessels. Potassium helps relax blood vessels and helps the kidneys eliminate sodium. Too much potassium can be harmful to someone with kidney disease, so this needs to be considered.
Exercise: The heart is a muscle that needs to be exercised. Regular exercise increases stroke volume, and decreases heart rate and blood pressure. When blood is actively moving throughout the circulatory system, as in exercise, it is less likely to pool in the extremities. Blood that is stagnant is prone to thrombus formation. Lack of physical activity is associated with increased BMI, hypertension, and obesity, all of which are associated with cardiovascular vulnerability.
Sleep: Researchers found that sleep issues, especially not sleeping enough, obstructive sleep apnea and insomnia can influence the risk of obesity, high blood pressure, Type 2 diabetes, stroke, coronary heart disease and overall cardiovascular disease. For more information on sleep and its effects on blood pressure, the heart, and brain health, check out these articles:
- sleep apnea video (sleep apnea) found at https://www.youtube.com/watch?v=LeOYEMg_EVE&t=2s
Hypertension: If the heart has to pump blood through vessels that are narrow and constricted due to hypertension, the work of the heart increases, leading to hypertrophy of the left ventricle. High blood pressure is a cardiovascular issue by itself, but a person who has elevated blood pressures is at risk for many other cardiovascular disorders. These include coronary artery disease, heart attack, and heart failure.
Diabetes: Diabetes is highly associated with atherosclerosis and heart disease. The extra glucose in the blood causes the blood to move more slowly and makes the cellular components of the blood “stickier.” This creates a situation where vessel walls can become thicker and stiffer and become a more welcoming surface on which to form thrombi.
Cholesterol: High levels of Low Density Lippoproteins (LDL) and low levels of High Density Lippoproteins (HDL)are linked to cardiovascular disease.The extra fatty substances in the blood are thought to damage the inner lining of arterial walls or stick to an existing thrombus, increasing the effects of atherosclerosis. The HDLs (good cholesterol) are believed to adhere to the LDLs and carry them to the liver for processing and removal.
Stress: The correlation between stress and cardiovascular disease has not been clearly demonstrated, but is it clear that stress can lead some people into unhealthy lifestyle choices, which are associated with hypertension and vascular damage. Some people drink alcohol when under stress. Some people make less-healthy food choices, have trouble sleeping, smoke cigarettes, or decrease their physical activity. All of these activities can lead to cardiovascular problems.
Alcohol use: Drinking too much alcohol can damage the blood vessels, liver and kidneys. Damage to these areas is highly associated with high blood pressure and heart disease.
6.4 General Signs and Symptoms of Cardiac Problems
The signs and symptoms of cardiac problems can be very obvious, but often, particularly in early stages of chronic conditions, they are not. It is important to check a patient’s medical history for information regarding cardiac problems, and to monitor vital signs during physical therapy interventions. A good PTA pays attention to a patient’s subjective reports and to objective signs and acts quickly if problems involving the heart are suspected. Some general signs and symptoms are listed below:
- Change in heart rate
- Change in blood pressure
- Fatigue
- Shortness of breath
- Edema, especially in the feet and ankles
- Dizziness, light-headedness, syncope
- Chest pain, or pain in arm, neck, jaw
- Sweating
- Cyanosis
- Sudden weight gain, due to fluid retention
6.4 – Resource 01 – General signs and symptoms of cardiac problems
6.5 Heart Failure
Heart failure, also known as congestive heart failure (CHF) is a condition in which the heart is unable to keep up with its job of pumping blood throughout the body. Risk factors for the development of CHF include: hypertension, age, obesity, smoking, physical inactivity, diabetes mellitus, and metabolic syndrome.
6.5 Resource 01 – What is heart failure? – Khan Academy Medicine – What is heart failure?
Congestive heart failure is categorized into systolic failure and diastolic failure and left-sided failure and right-sided failure. These labels refer to the side of the heart that is first affected, and the signs and symptoms are reflective of the area of the heart that is damaged or defective.
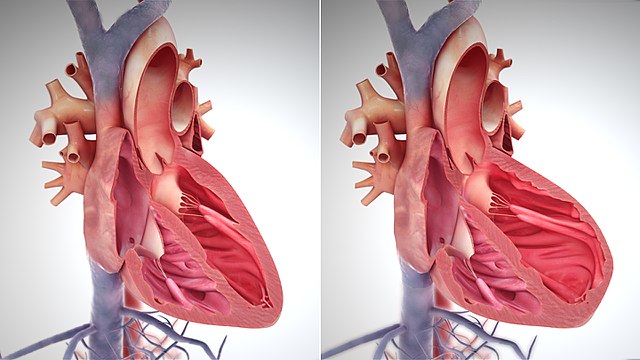
6.5.1 Systolic Failure
Systolic failure occurs when there is a problem with the pumping mechanism of the heart. Often cardiac muscle is damaged or weak because of ischemic heart disease, in which oxygen to the heart muscle is diminished. Without adequate oxygenation, the cardiac muscle becomes weak and can die. If the heart is unable to generate enough force to pump out an adequate amount of blood with each beat, the extra blood in the heart causes the ventricles to expand and the walls of the heart become thinner. The over-stretched muscles are able to contract with less force, so the condition worsens over time.
6.5.2 Diastolic Failure
Diastolic failure occurs when the heart is not receiving an adequate volume to fill the heart and expand it enough to elicit a strong contraction. A thickening, or hypertrophy, of the ventricular walls is most often the main problem in diastolic failure. In the left ventricle, hypertrophy most often occurs as a result of long-standing hypertension. The hypertension creates increased resistance for the heart to pump against, and the heart muscle size increases in response to the extra work. Other causes for thickening of the left ventricle include aortic stenosis and congenital cardiac hypertrophic cardiomyopathy. Diastolic failure in the right side of the heart is most often caused by stiffening or thickening of the right ventricular walls, which could be due to pulmonary edema (often a result of left-sided heart failure), pulmonary valve stenosis, pulmonary hypertension, or resistance in the lungs from respiratory disorders.
6.5.3 Left-sided Heart Failure
In left-sided CHF, the problems occur in the mitral valve, left ventricle or aorta and peripheral arteries. The heart muscle itself can be damaged or not functioning properly over the left atrium or left ventricle. The mitral valve can be either stenotic, or very floppy (prolapsed). In the case of mitral valve stenosis, the stiff valve does not allow adequate blood to flow into the left ventricle, so blood backs up into the left atrium, pulmonary veins, and lungs. If the valve is prolapsed, there may be too much blood entering the left ventricle, causing it to become distended and overworked. Blood will again continue to back up into the pulmonary veins and lungs. In the case of high blood pressure (hypertension), the peripheral arteries are narrow and stiff, which creates resistance to blood pumping from the left ventricle. This also leads to left-sided heart failure and excess fluid in the lungs. This back-up of blood and fluid in the lungs is what causes the most common symptoms of left-sided CHF: shortness of breath, persistent cough, orthopnea, fatigue, dizziness and syncope, tachycardia, palpitations, and reduced urine output.
It is very common for the left side of the heart, particularly the left ventricular wall, to become thin and overstretched, leading to weakness if the left ventricle is over-filling and/or under-emptying. This decreases contractility of the cardiac muscle and leads to further decrease in blood ejection from the left ventricle. Sometimes, the left ventricle becomes hypertrophied in this condition, due to the constant increased workload of the left ventricle. The longer this condition persists, the more distended the walls of the heart become and the thicker the left ventricle musculature becomes. The heart becomes less and less efficient at pumping blood to the body, creating greater problems throughout the body.
As left-sided heart failure progresses, the flow of blood through the heart becomes more and more difficult, and eventually the right side of the heart also fails.
6.5.4 Right-sided Heart Failure
In right-sided CHF, the problems occur somewhere between the right heart and the lungs. Often, the pulmonary valve is stiff, or stenotic, or pulmonary hypertension exists because of narrowed lumens in the pulmonary arteries. The result is that blood cannot be efficiently pumped out of the right side of the heart and into the lungs. The blood backs up in the right side of the heart, and into the venous circulatory system. Another cause of right-sided heart failure is a septal defect, either between the atria or between the ventricles. Since the pressure is greater in the left side of the heart than the right, if there is an opening between the two sides of the heart, blood will flow from left to right, over-filling the right side of the heart.
In right-sided heart failure, edema is often present in the periphery, especially in the legs of a patient who is upright, and in the sacral area in a patient who is predominantly in the supine position. This is known as “dependent edema,” because it is dependent upon the patient’s positioning in relation to gravity. “Pitting edema” can be detected by pressing into the edematous extremity. If it is pitting edema, the indentation will remain visible for several seconds or minutes.


Venous distension is also frequently present in the jugular veins in the neck. As the right-sided CHF progresses, abdominal swelling (ascites) can develop, and the patient might also develop kidney and liver problems. Other issues associated with right-sided CHF include oliguria (frequent nighttime urination), blood clots, and liver and kidney failure.
The right side of the heart often becomes stretched out if blood cannot be pumped out of the right ventricle. This causes enlargement of the right side of the heart, either from stretching and thinning of the walls of the right ventricle or from right ventricle hypertrophy, as the heart muscle is being overworked in pumping blood to the lungs against increased resistance. Over time, the body’s compensations for right-sided heart failure lead to left-sided heart failure, too.
To learn more about classification systems for heart failure, refer to the charts and explanations from the American Heart Association at this site.
6.5.5 Interventions for Heart Failure
Heart failure cannot be cured, but it can be managed as a chronic illness. Prevention of heart failure is certainly more desirable than treatment once it is identified, but management is possible, and the effects can be minimalized through important lifestyle changes. Maintaining a normal blood pressure, maintaining a normal weight, consuming a diet that is low in sodium, fat, and cholesterol, and exercising regularly will all be beneficial in controlling heart failure. Most people who are diagnosed with heart failure will be prescribed several medications.
These could include ACE inhibitors, beta-blockers, diuretics, and cholesterol-reducing medications. If heart failure is significantly impacting the pumping of the heart and medications are unable to effectively control cardiac output, surgical intervention might be necessary.
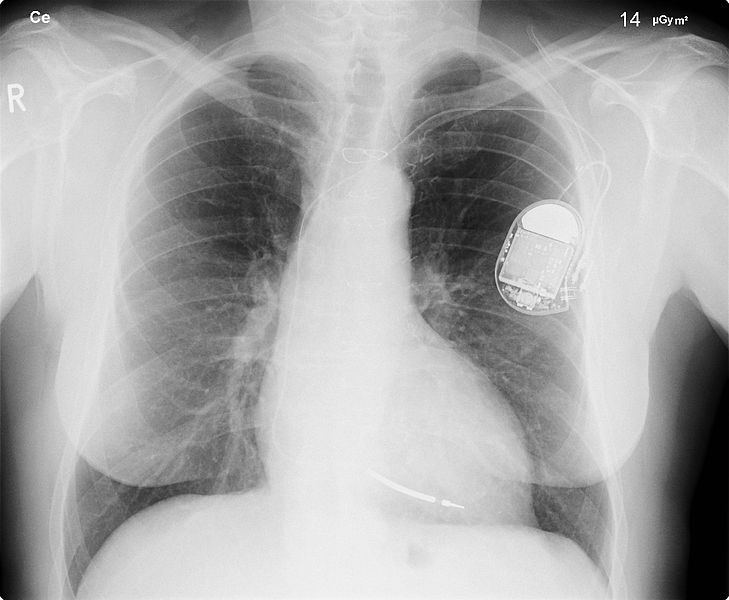
An artificial cardiac pacemaker might be implanted if the heart rate is slow or the conduction from the atria is weak. The device consists of a pacemaker unit that is implanted under the skin in the chest or abdomen which connects to wires and electrodes placed on the heart.
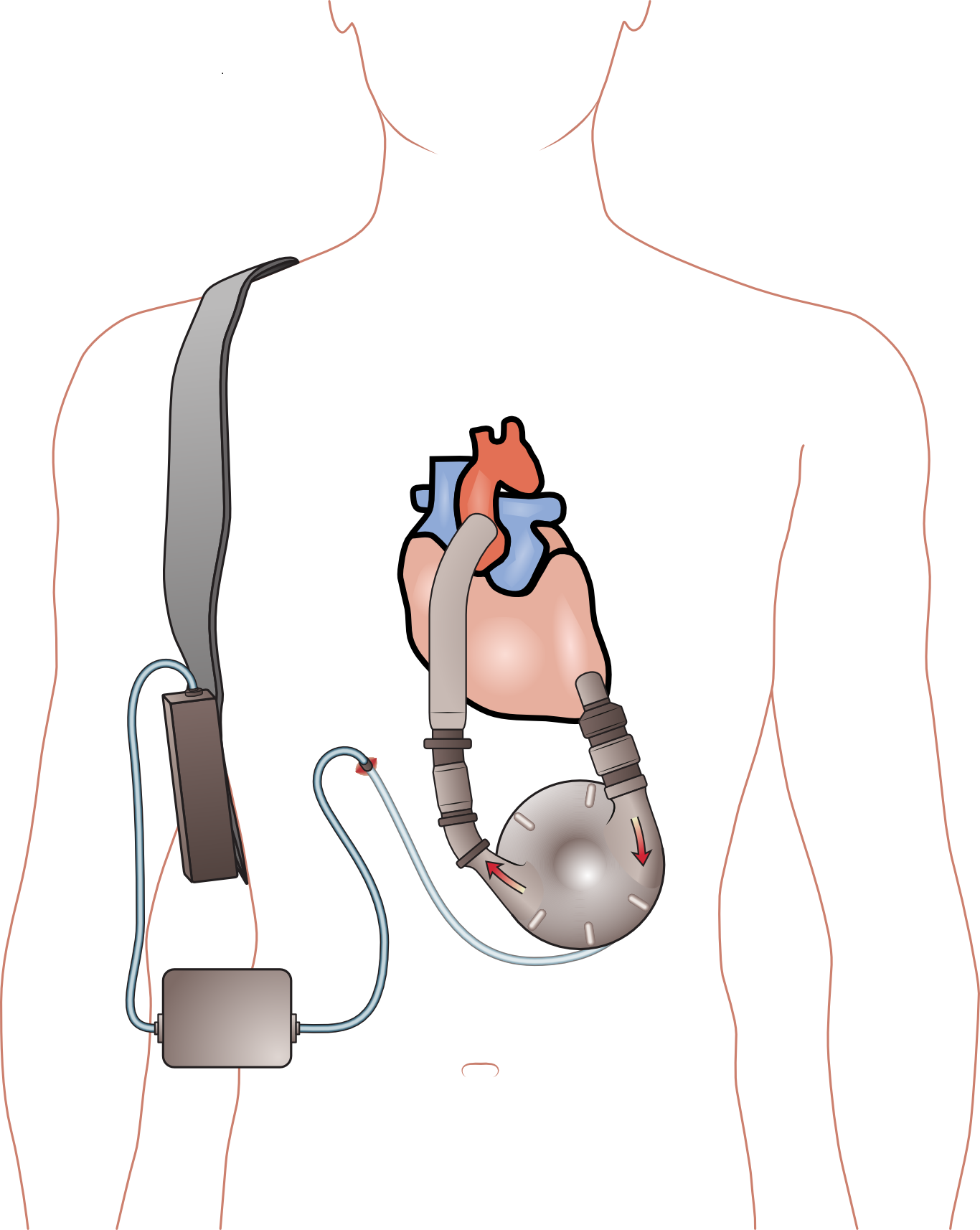
If the ventricles are weak and need assistance in fully ejecting blood, a ventricular assistive device (VAD) can be implanted. These are often used as a temporary bridge in a failing heart until a heart transplant is possible. In these cases, if a heart transplant is possible, either a human cadaver heart or an artificial heart could be surgically implanted.
Think about this….
When a patient develops congestive heart failure, their body will try to compensate for the lack of oxygen being carried to the organs. Consider each of these compensations, and explain why each of these compensations occur. (Hint: Think about CO = SV x HR and the Frank-Starling mechanism discussed in the Kahn Academy video). Also, consider why each might ultimately make the problem worse.
- Tachycardia
- Increased blood volume
- Increased cardiac filling pressure
- Increased cardiac muscle mass
Exercises
- Why is a bathroom scale a useful diagnostic tool for a PTA when working with patients who have CHF?
- Would compression therapy be indicated or contraindicated to help reduce edema in the lower extremities of a patient with CHF? Why or why not?
- A patient with CHF might be prescribed many different medications. Three common ones are Lasix, Vasotec, and Lopressor. For each drug, list the drug type (ACE inhibitor, Beta Blocker, etc.) and describe possible side effects and how the side effects might affect physical therapy treatments.
- How could physical therapy be helpful to a patient with CHF? Describe a few possible interventions.
- What are some “red flags” that would alert a PTA to stop or modify PT interventions with patients with CHF?
- Is the ejection fraction (EF) more likely to be abnormally low in a patient with systolic or diastolic heart failure? Why? (This would be a good time to review normal EF values.)
- For patients taking beta blockers, a rate of perceived exertion (RPE) scale is often used in place of measurement of heart rate to determine how hard a patient is working. Why is heart rate not that useful?
- Why are patients with CHF often encouraged to maintain a diet that is low in sodium?
Activities
- Draw a box diagram of the heart to show the area of dysfunction and results in the heart if a patient has a pulmonary valve stenosis. List signs and symptoms of the resultant type of heart failure.
- Do the same for an aortic valve stenosis.
6.6 Cardiac Circulation
The myocardium (heart muscle) needs oxygen and other nutrients in order to maintain its constant pumping in order to supply oxygen to all areas of the body. Waste products, including carbon dioxide also need to be carried away. The exterior of the heart has a network of coronary arteries which arise from two main coronary arteries, the right and left coronary arteries. Each vessel has many branches to supply all areas of the heart with blood and essential oxygen and nutrients.
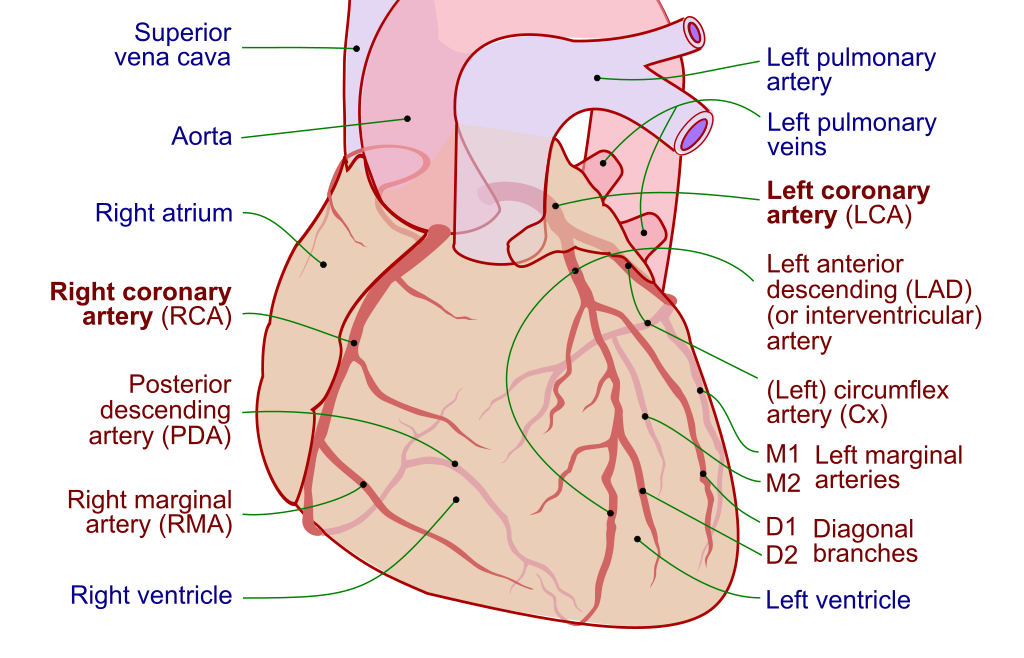
Long Description
Text with lines pointing to the locations of the following:
On the left side:
- Superior vena cava
- Aorta
- Right atrium
- Right coronary artery (RCA)
- Posterior descending artery (PDA)
- Right marginal artery (RMA)
- Right ventricle
On the right side:
- Left pulmonary artery
- Left pulmonary veins
- Left coronary artery (LCA)
- Left anterior descending (LAD) (or interventricular) artery
- (Left) circumflex artery (Cx)
- M1 Left marginal
- M2 arteries
- D1 Diagonal
- D2 branches
- Left ventricle
6.7 Coronary Artery Disease and Related Disorders
Plaque can build up on the inner walls of arteries, causing the lumen through which blood flows, to be narrowed. If this process affects the coronary arteries, this is coronary artery disease (CAD). If plaque builds up in a particular area, a clot, called a thrombus or atheroma, can form. If a thrombus forms in in any of the coronary arteries, blood supply to areas of the myocardium can become compromised. As the blood supply decreases (ischemia), oxygen supply decreases (anoxia), the heart muscle becomes less able to contract, and angina and myocardial infarction can be the result.
Risk factors for the development of CAD include smoking, obesity, lack of physical activity, high blood pressure, diabetes mellitus, high cholesterol, depression, excessive alcohol use, and genetic factors.
According to the Centers for Disease Control and Prevention (CDC), CAD is the most common cause of death in the US. Many people do no know they have CAD and the first sign could be a heart attack.
If the coronary circulation is compromised, the heart muscle might have difficulty keeping up with the demands for oxygen for the rest of the body. This can lead to chest pain known as angina pectoris. If the blood supply is completely occluded in a coronary artery, part of the heart muscle might die. This is known as a heart attack or myocardial infarction (MI), and can be very serious or fatal.
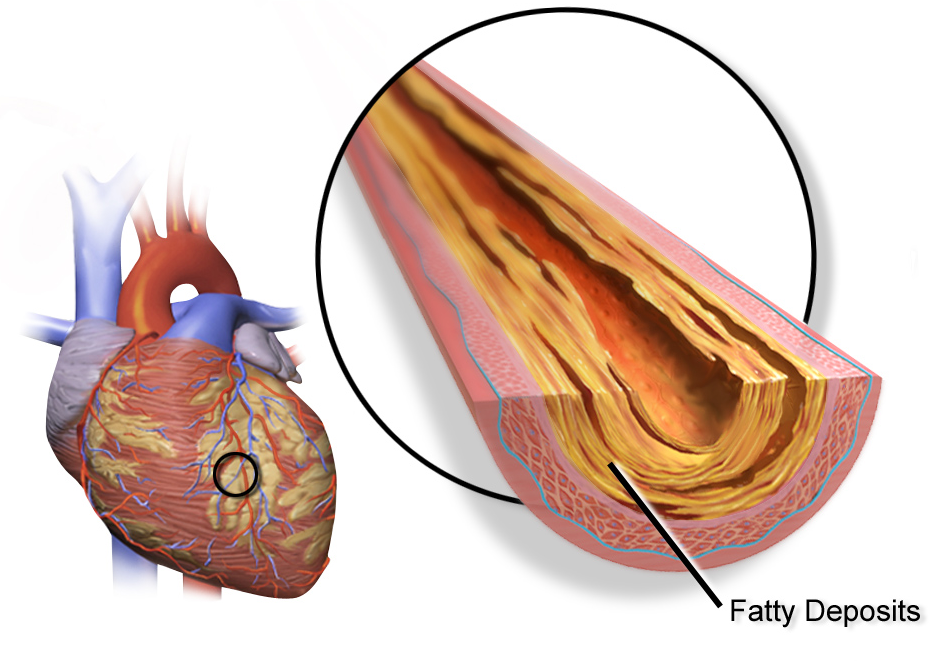
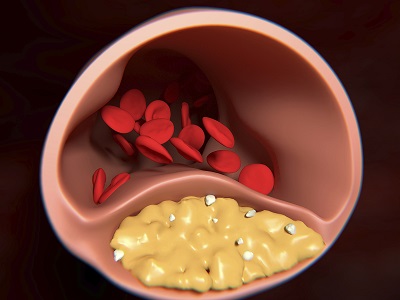
Coronary artery disease is caused by plaque buildup in the wall of the arteries that supply blood to the heart (called coronary arteries). Plaque is made up of cholesterol deposits. Plaque buildup causes the inside of the arteries to narrow over time. This process is called atherosclerosis. Source CDC: Coronary artery disease
6.7 – Resource 03 – Khan Academy – What is coronary artery disease?
6.7.1 Angina Pectoris
Angina pectoris is chest pain that is associated with a sudden decrease in oxygen supply to the myocardium. It occurs in the presence of coronary artery disease, as the lumen of the coronary arteries become smaller, with the build-up of plaques on the inner walls of the arteries. An episode of angina includes chest pain or pressure, and generally last a few minutes. In most cases, it does not cause damage to the heart. Rather, it is a warning sign of potential for myocardial infarction (MI, or heart attack). Angina generally occurs in predicable patterns, often with exertion or stress, or after eating. This is known as stable angina. Acute episodes of angina are relieved by the use of nitroglycerin tablets, which are administered under the tongue (sublingual). Most patients who have been diagnosed with angina are also prescribed statins (e.g. Lipitor, Crestor), beta blockers (e.g. Carvedilol, Propanolol), calcium channel blockers (e.g. Amlodipine (Norvasc), Nicardipine (Cardene), and anti-platelet drugs (e.g.. aspirin, Plavix).
If angina occurs at rest or at times when it would not be expected, it is called unstable angina. This kind of angina is considered to be more dangerous than stable angina.
6.7.2 Myocardial Infarction
Myocardial infarction, or heart attack, occurs when heart muscle becomes deprived of oxygen through ischemic heart disease (CAD), and dies, leaving an area of the heart damaged. Ischemia, or lack of blood supply, causes anoxia, or lack of oxygen to tissues that are normally supplied by the occluded blood vessel. This area of infarction undergoes necrosis, or cell death, and is replaced with scar tissue, which maintains the integrity of the structure of the heart, but does not have the ability to contract as cardiac muscle does. The most common cause for heart attack is a complete blockage of a coronary artery due to atherosclerotic changes (thrombus formation) and/or vasospasm and/or embolism. A large thrombus can decrease blood supply to areas of the heart, so that not enough oxygen is available for necessary heart function, especially during periods of physical exertion or stress. Blood vessels can also constrict (vasospasm) because of the thrombus, further narrowing the lumen through which blood can flow. Sometimes, a piece of a thrombus, or the entire thrombus, can break loose and be carried into smaller vessels in the blood. If this occurs, the clot is called an embolus. As the embolus travels into smaller and smaller arteries, it can become lodged between the vessel walls, blocking blood supply to areas beyond.
The most common area for MI is over the left ventricle, and occurs with blockage of a branch of the left coronary artery.
6.7 – Resource 04 – Khan Academy – Heart Attack Pathophysiology
6.7.2.1 Signs and symptoms of heart attack
A person experiencing a heart attack or myocardial infarction might feel the classic symptoms of crushing pain in the chest and into the left shoulder and arm, or they might not. Sometimes, the symptoms include jaw pain, shortness of breath, nausea or feeling of indigestion, dizziness, diaphoresis, exhaustion, anxiety, irregular heartbeat, and lingual pain. Women, in particular, are less likely to experience the classic chest pain in association with a heart attack, and are more likely to feel anxious or to complain of indigestion.
6.7.2.2 Interventions for Heart Attack
It is imperative that a person experiencing the symptoms described above get immediate medical attention. Tests, such as electrocardiogram (ECG) and blood enzyme levels, need to be administered as soon as possible to diagnose a heart attack and allow treatment to begin. Certain enzymes, such as creatine phosphokinase (CPK), aspartate transferase (AST), and lactic dehydrogenase (LDH) can be drastically altered following and MI and are very helpful in making the diagnosis.
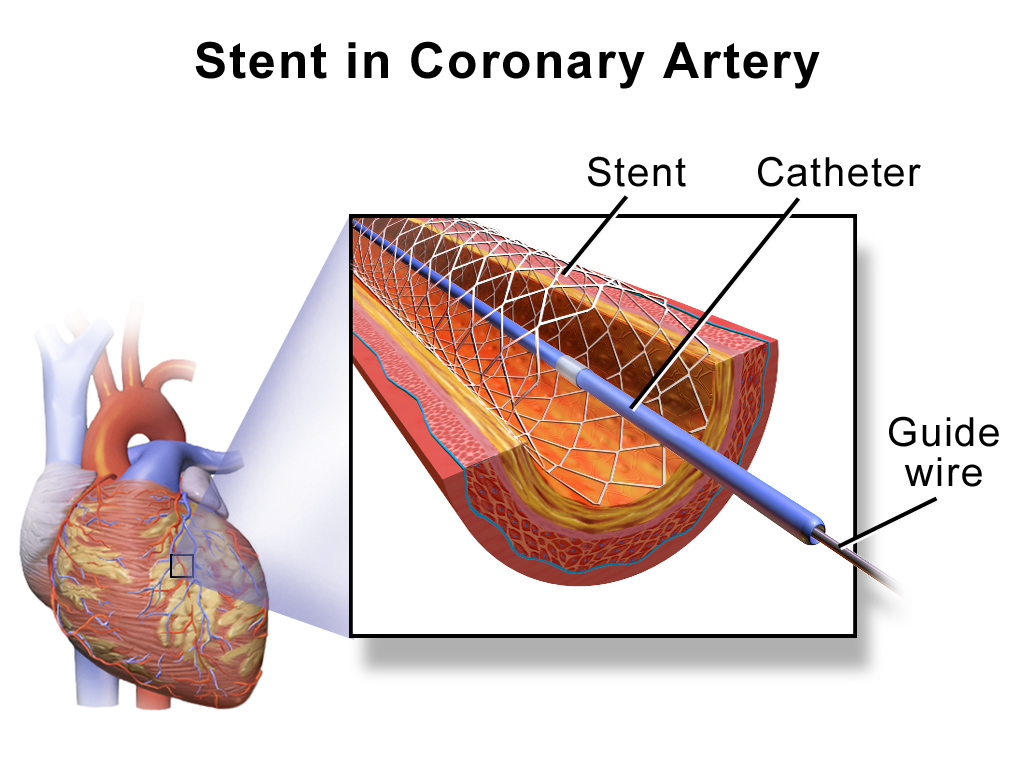
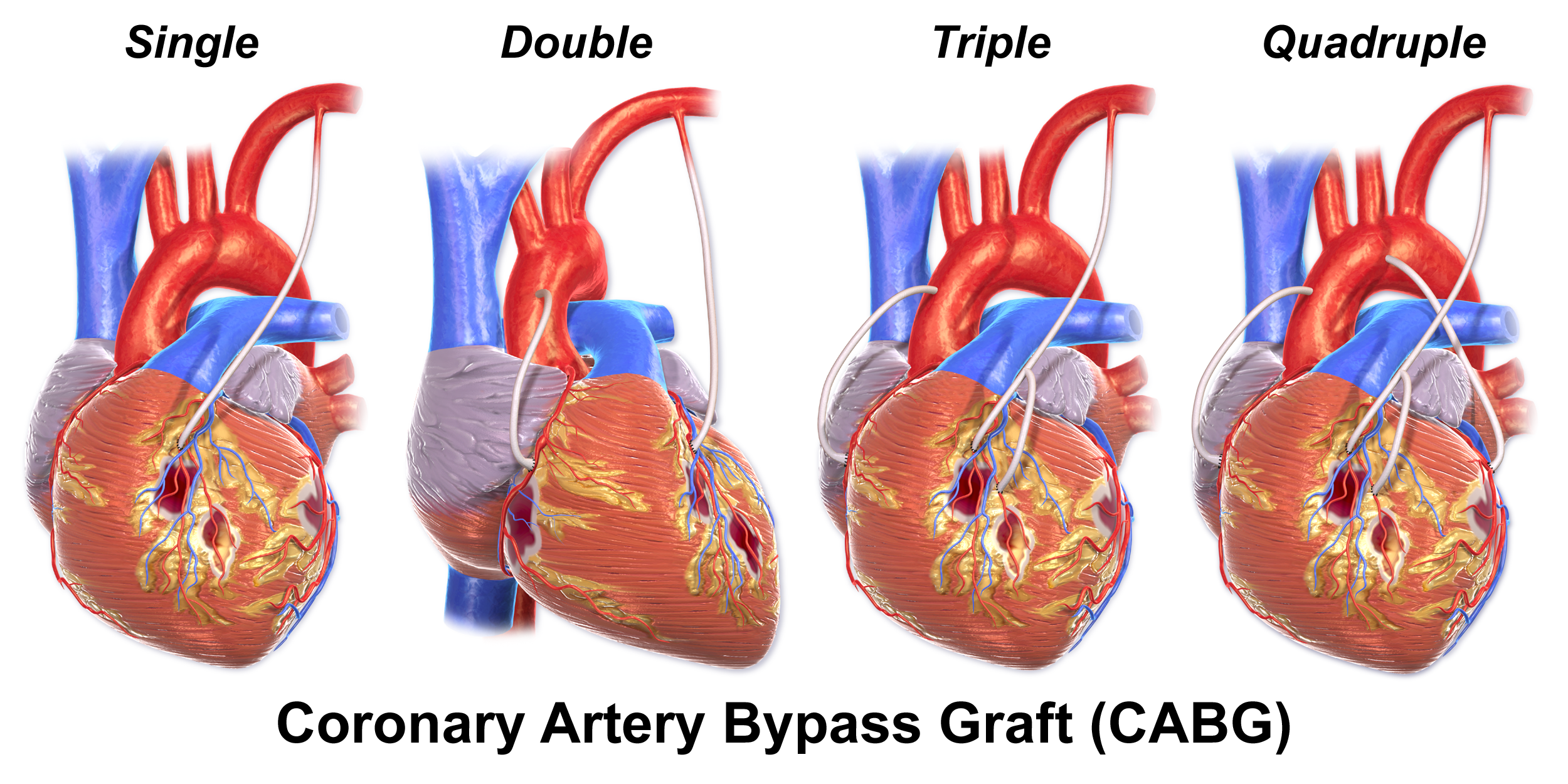
Treatment immediately following an MI can vary, but it usually includes administration of medications to decrease coagulation of blood and reduce thrombus formation, so that the chances of a second cardiac event are lessened. Patients are also generally prescribed pain relievers, antihypertensives, and cholesterol-lowering medications. Some patients require surgical intervention, which might be an angioplasty with stenting or coronary artery bypass surgery. In a stenting procedure, a small stent is inserted into a coronary artery in a percutaneous coronary intervention (PCI), known as an angioplasty. The surgeon makes a small incision in the groin, upper arm or neck of the patient, and inserts a catheter into a vein. The surgeon then threads the stent, which is a small mesh tube, through the venous system into the appropriate coronary artery. If the blockage is very large, a coronary bypass graft (CABG)might be necessary. In this procedure, the surgeon uses a vein, usually from the leg, to build a blood vessel in the heart that will bypass the occluded area. This might need to be performed on several affected arteries (e.g. triple or quadruple bypass).
6.7.2.3 Cardiac Rehabilitation
Outcomes following a myocardial infarction vary greatly, depending upon the area of the heart that was damaged, the extent of the damage, timeliness and appropriateness of care, and the general condition of the individual. Patients should progress through a cardiac rehabilitation program, starting with the cardiac care unit (CCU), and progressing throughout the hospital stay and home. The program should include monitoring of heart function and vital signs, gradually increasing activity, and patient education. Learning to identify and diminish risk factors and recognizing warning signs are important in a patient’s success in managing their cardiac condition and decreasing the risk for a future cardiac event.
Discussion Questions
- Consider the following patient: 60 year old post-menopausal female suffered an MI one week ago. Her co-morbidities include Type 2 DM for 10 years, controlled with oral medication; cigarette smoker 1 pack per day for 40 years; hypertension (Stage 2) diagnosed 3 months ago. Social history: Works full-time, local bank branch manager; divorced 2 years ago after 35 years of marriage, no children; lives alone in a 2 story home; reports little or no physical activity daily. Medication list: Plavix, Zestril, Coumadin, Inderal, Lipitor, Metformin
- The patient asks you why she “is on all these medications.” Discuss how you would talk with her about her meds.
- The patient reports she is worried she will have another heart attack and asks what she can do to help decrease her chances of a second MI. What would you tell her?
- Consider this patient: a 70-year old male is recovering from a THA (total hip arthroplasty). He was diagnosed with CAD when he was 58 years old, and has tried to control his risk factors and has remained active with yard work and swimming 3 days per week.
- What kinds of precautions should a PTA take in caring for this patient?
- What signs and symptoms should a PTA be watching for during the PT for his THA? Think of examples that are “watch and see” and those that might be considered “red flags.”
6.8 Cardiac Conduction: Arrhythmias/Dysrhythmias
For a review of the conduction system of the heart, watch the video below:
6.8 – Resource 01 – Khan Academy – Electrical System of the Heart
There are various problems that can occur in generating and conducting electrical impulses in the heart. Some of the most common arrhythmias, or dysrhythmias are explained below.
6.8.1 Premature contractions
Premature atrial contractions can occur in the atria or ventricles. Premature atrial contractions (PACs) or premature ventricular contractions (PVCs) are fairly common and generally considered to be harmless in otherwise healthy people. They are described as a fluttering feeling in the chest or a skipped heartbeat. Premature contractions can be cause by too much caffeine, potassium imbalance, stress, or exercise. They can also be associated with some other cardiac conditions.
6.8.2 Supraventricular arrhythmias
Supraventricular arrhythmias cause fast heart rates, or a condition called tachycardia. These are generated in the atria or A-V node and include several types: atrial fibrillation (AF), atrial flutter, paroxysmal supraventricular tachycardia (PSVT), and Wolff-Parkinson-White (WPW) syndrome.
6.8.2.1 Atrial Fibrillation (AF)
Atrial fibrillation is a potentially serious condition that occurs when the heart’s electrical conduction system is not working properly. Electrical impulses are generated at or near the A-V node and spread over the atria and travel to the ventricles in fast and irregular patterns. The atria quiver instead of contracting normally, and the ventricles contract rapidly with decreased force. Without normal contractions in the atria, the ventricles fail to fill completely, so less blood gets pumped out of the heart. The two serious effects of AF are stroke and heart failure. Stoke occurs if the slow blood in the heart allows clots to form, which can travel to the brain and occlude a small artery there. Heart failure occurs when the heart is not pumping an adequate volume, and the blood backs up into the lungs and periphery. AF sometimes has an unknown etiology, but it is also associated with hypertension, CAD, diabetes mellitus, and rheumatic heart disease. Hyperthyroidism and alcohol use are also associated with the development of AF.
Conduction
6.8 – Resource 02 – Sinus Rhythm – “File:Heart conduct sinus.gif” by is licensed under CC BY-SA 3.0 – Arterial Fibrillation – “File:Heart conduct atrialfib.gif” by is licensed under CC BY-SA 3.0 – Love this animation of AF
6.8.2.2 Atrial Flutter (AFL)
Atrial flutter also occurs when the atria contract rapidly and irregularly due to cardiac conduction abnormalities. It is much less common than AF, but also causes the atria to quiver, leading to the same complications as AF. AFL often progresses to AF. AFL is most common in people with known heart disease or condition, although it can occur in healthy individuals.
6.8.3 Paroxysmal Supraventricular Tachycardia (PSVT)
Paroxysmal supraventricular tachycardia occurs when the conduction system between the atria and ventricles fails to operate correctly and electrical signals are transmitted to the ventricles and return to the atria. The result is a sudden rapid heart rate, which is usually self-limiting. This type of tachycardia most often occurs in young individuals during periods of physical activity and is not usually considered dangerous. Symptoms can include palpitations, and syncope. A particular type of PSVT is quite serious, however.
6.8.4 Wolff-Parkinson-White (WPW) Syndrome
Wolff-Parkinson-White (WPW) syndrome can be a life-threatening form of PSVT in which electrical signals are transmitted along extra conduction routes (the Bundle of Kent) to the ventricles, causing extra heart beats and ineffective pumping mechanisms. The reason for the extra conduction fibers in the heart is unknown, and many people may have a Bundle of Kent and never exhibit symptoms, which can include PSVT, syncope, shortness of breath, palpitations, and rarely, cardiac arrest.
6.8.5 Ventricular arrhythmias/dysrhythmias
Ventricular arrhythmias are conduction abnormalities in which the electrical disruption occurs in the ventricles. Myocardial infarction, heart failure, coronary artery disease, and other heart conditions can cause ventricular arrhythmia, which can be life-threatening. The two types of ventricular arrhythmia are ventricular tachycardia and ventricular fibrillation.
6.8.5.1 Ventricular tachycardia (V-tach)
Ventricular tachycardia is a fast, regular heartbeat. An episode can last only a few seconds, which is not dangerous. If the episode lasts several minutes or longer, it can be very dangerous, progressing to ventricular fibrillation, which can be fatal.
6.8.5.2 Ventricular fibrillation (V-fib)
Ventricular fibrillationis a very serious condition where the ventricles quiver, unable to adequately eject blood. This can occur during a heart attack or other cardiac event. If this condition is not treated immediately with defibrillation, sudden cardiac arrest and death may be the result.
6.8.6 Bradyarrhythmia
Bradyarrhythmia or bradycardia occurs when the heart beats more slowly than normal. A normal heart rate for an adult is 60-100 beats per minute. A heart rate lower than 60 bpm is considered atypical, unless the individual is very fit, where a lower heart rate is normal. For people with bradycardia, symptoms may include vertigo, hypotension, and syncope, all of which indicate decreased blood flow to the brain. Bradycardia can occur following heart attack, or in the presence of chemical (potassium) imbalance, hypothyroidism, or as a side effect of medications, such as beta blockers, calcium channel blockers, some anti-arrhythmia medicines, and digoxin. It is interesting to note that some of these medications limit the normal increased heart rate than typically accompanies physical exertion; therefore, a patient’s rating of perceived exertion could be a better indicator of exercise intensity than heart rate.
6.8.7 Treatments for Arrhythmia/Dysrhythmia
Many arrhythmias are mild and unlikely to cause any serious problems, and these are often left untreated. In a life-threatening situation with a volatile arrhythmia, such as ventricular fibrillation, defibrillation can be used to shock the heart into a normal rhythm. Medications can be administered to help correct an arrhythmia or to help maintain a normal cardiac rhythm. Beta blockers, calcium channel blockers, or digitalis preparations are the types of drugs most commonly used to treat arrhythmias. For arrhythmias not able to be controlled by medications, surgical interventions can be employed. Cardiac ablation is a surgical procedure that destroys a small amount of cardiac tissue, blocking the path for unwanted electrical impulses through the heart muscle. It can be helpful in regulating heart rates, especially in the case of supraventricular arrhythmia. For bradycardia or blockage of the normal conduction routes for electrical impulses in the heart, an artificial cardiac pacemaker can be surgically implanted.
6.9 Disorders affecting the blood vessels
For a short refresher on blood pressure and what the systolic and diastolic numbers mean, watch the video below.
6.9 – Resource 01 -What is Blood Pressure? – Khan Academy – What is Blood Pressure?
6.9.1 Hypertension
Hypertension (HTN), or high blood pressure, is a condition that affects many people world-wide and is an established risk factor for coronary artery disease, stroke, heart failure, peripheral vascular disease, kidney disease, blindness, and dementia. Hypertension is defined as an arterial systolic blood pressure of 120 or higher and a diastolic pressure of 80 or higher. The categories of blood pressure values are listed in the chart below.
The categories of blood pressure values that were established by the American College of Cardiology and the American Heart Association in 2017 are listed in the chart below.
| Blood Pressure Category | Systolic mm Hg (upper#) |
And/Or | Diastolic mm Hg (lower#) |
|---|---|---|---|
| Normal | less than 120 | and | less than 80 |
| Elevated | 120-129 | and | less than 80 |
| High Blood Pressure (Hypertension) Stage 1 |
130-139 | or | 80-89 |
| High Blood Pressure (Hypertension) Stage 2 |
140 or higher | or | 90 or higher |
| Hypertensive Crisis (Seek Emergency Care) |
higher than 180 | and/or | higher than 120 |
6.9 – Resource 02 – Blood Pressure Stages – “Blood Pressure Categories” by The American Heart Association is licensed under All rights reserved (2018).
- Stop smoking or using any tobacco-related products
- Lose weight, if necessary
- Improve diet by decreasing sodium, increasing potassium (can be contraindicated in the presence of kidney disease); general dietary instructions: eat more vegetables, fewer sweets and fatty foods
- Exercise regularly
- Sleep regularly and adequately (8 hours per night)
- Decrease stress
6.9.2 Hypotension
Blood pressure that is lower than the recommended values (see chart above) is also dangerous. In general, adults with a systolic pressure below 90 mm HG or a diastolic pressure below 60 mm Hg are considered to have hypotension. The effects of hypotension include light-headedness, dizziness, and fainting. Orthostatic hypotension, or positional hypotension, is associated with a change of position, especially rising from supine to sitting or from sitting to standing. Patients who have been in bed for an extended period are at especially high risk for orthostatic hypotension. Other associated risk factors for hypotension include low blood volume, cardiac condition, or other condition that causes the blood vessels to excessively dilate or the heart to be an inefficient pump for blood.
The cause of hypotension needs to be determined and treated, as hypotension is almost always a symptom of an underlying condition.
Discussion Questions
- What steps should a PTA employ to help decrease the risk of a fall because of orthostatic hypotension when assisting a patient out of bed for the first time after a long period of bed rest?
- If a patient feels dizzy while ambulating, what should a PTA do?
6.9.3 Atherosclerosis and Arteriosclerosis
Arteriosclerosis is a general term that is used to describe arterial changes that include stiffening and thickening. This occurs as a process of aging, and particularly in people who smoke or have elevated cholesterol levels. Arteriosclerosis leads to atherosclerosis and hypertension.
Atherosclerosis is a specific type of arteriosclerosis which includes the build-up of fatty deposits, or plaques, in the arteries. Atherosclerosis occurs in blood vessels which have been damaged due to high blood pressure, smoking, diabetes, or other causes. Atherosclerosis in the coronary arteries is coronary artery disease, which is associated with heart attacks and heart failure.
6.9.4 Peripheral Artery Disease (PAD) or Peripheral Vascular Disease (PVD)
If the arteries in the periphery become narrowed due to arteriosclerosis or atherosclerosis, the muscles may not receive adequate blood supply or oxygen. This can lead to pain and cramping. The arteries of the lower extremities are the most common site for PAD, but it can occur in other areas of the body. Intermittent claudication is the most common symptom of PAD. Other symptoms include cold skin, bluish skin, ulcers, and delayed healing. Risk factors for PAD include smoking, high blood pressure, diabetes mellitus, hypercholesterolemia, and sedentary lifestyle.
6.9.5 Deep Venous Thrombosis (DVT)

A thrombus or clot can form in a vein anywhere in the body, but the most common area is in the deep veins of the lower leg. Superficial veins can also be affected in a superficial venous thrombosis, but these tend to be much less serious and usually result in a self-limiting bout of thrombophlebitis (inflammation).
Prevention of a DVT is preferable to treatment after one occurs. Exercise, especially walking helps prevent DVTs. Even exercises as simple as ankle pumps (alternate dorsi- and plantar flexion of the ankles) help the muscles push blood through the vessels and can help prevent blood stasis, which can cause DVT. Patients are often instructed to wear compression stockings and maintain legs in an elevated position to help blood flow back to the heart, and keep it from pooling in the feet and legs.
DVTs are most often diagnosed via doppler ultrasound. They are generally treated with anticoagulant drugs, such as heparin. Sometimes, a small screen is surgically implanted in the inferior vena cava for a short period of time to “catch” clots returning to the heart.
Exercise, massage, and other forms of physical therapy are usually restricted in the presence of a DVT. Any activity that could cause the thrombus to break loose should be avoided until the DVT has been resolved.
6.9.6 Aneurysm
An aneurysm is a localized weakened area of an artery that bulges, or expands, due to the pressure of
the blood pumping through it. Aneurysms can form anywhere in the body, but they are most common and most serious in the thoracic or abdominal aorta and in the arteries in the brain. Some aneurysms are hereditary in nature. Many are linked to risk factors which include age, smoking, high blood pressure, diabetes, atherosclerosis, and alcoholism. It is important that people with known aneurysms maintain healthy blood pressures and have regular checks of the aneurysm size, generally assessed with ultrasound, MRI, CT scan or x-ray.
Most aneurysms are asymptomatic at first. As they grow, they may put pressure on adjacent structures that cause pain or discomfort. If they rupture or burst, the condition is life-threatening, as massive bleeding into body cavities can occur. As the blood leaves the circulation, blood pressure drops, syncope occurs, and shock ensues. Elective surgical repair of an aneurysm is recommended in most cases.
Watch the following video on abdominal aortic aneurysm (AAA).
6.9 – Resource 05 – Abdominal aortic aneurysms – Khan Academy – Abdominal Aortic Aneurysm
Exercises
- A patient is diagnosed with an AAA. He is 67 years old, a smoker, moderately obese, and leads a moderately active lifestyle, doing yard work and walking approximately 1 mile per day. He has Type 2 Diabetes. What is the most important advice you could give him regarding risk factors for AAA and other cardio-respiratory disorders?
- What other advice can you give him about his condition and general health?
6.10 Congenital Conditions of the Heart
6.10.1 Atrial Septal Defect (ASD)
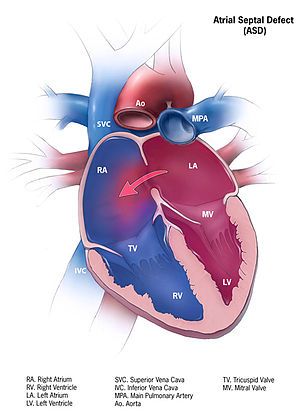
An opening (patent foramen ovale) between the right and left atria is normal in a fetus, as it allows the blood to bypass the nonfunctional lungs. When the baby is born, and the lungs begin working, the small hole should close completely. If this fails to occur, the hole can remain and blood with be able to pass between the atria. If the shunt is from left to right, oxygenated blood will be recirculated through the heart and lungs. The right atria can become enlarged if the hole is large and the situation is allowed to continue. If the shunt is right to left, deoxygenated blood will be pumped out into the circulation, posing a greater problem for getting oxygen to all parts of the body.
6.10.2 Ventricular Septal Defect (VSD)
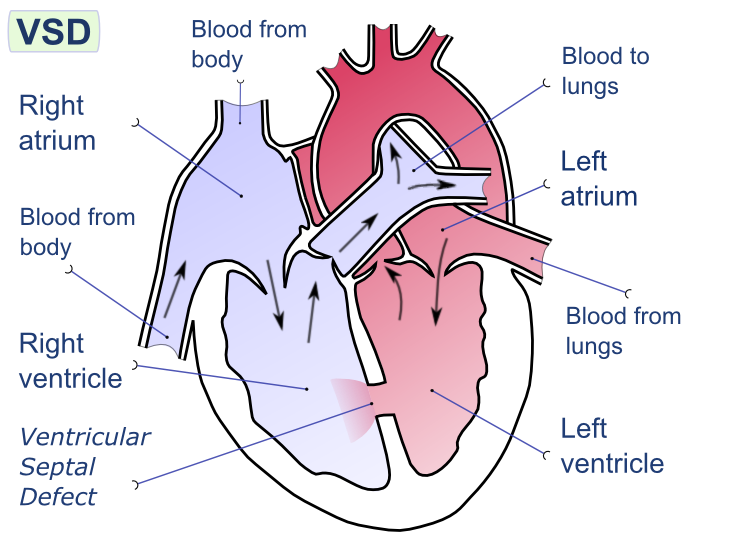
Long Description
Left side of image:
- Blood from body
- Right atrium
- Blood from body
- Right ventricle
- Ventricular Septal Defect
Right side of image:
- Blood to lungs
- Left atrium
- Blood from lungs
- Left ventricle
When there is a disruption in the tissue between
the right and left ventricles in a VSD, blood is able to flow between the two ventricles. Since the pressure is normally greater in the left side of the heart, blood flows from left to right, allowing oxygenated blood to be recirculated through the lungs. Over time and in the case of a large opening, the extra blood flow into the right ventricle can lead to increased pressure in the pulmonary vein and right ventricle, which can change the shunt from left-to-right to right-to-left. If deoxygenated blood from the right side of the heart flows to the left ventricle and gets pumped out to the body, cyanosis (bluing of the lips, fingers, and toes) can occur. Additionally, the individual in this case will fatigue easily,
experience shortness of breath, and begin to show signs of heart failure.
Sometimes, if the defect is small, the hole will grow closed during childhood. Sometimes, again in the case of a small opening, there will be no symptoms and no treatment is required. If the hole is large, surgery is required to repair the defect and prevent the effects of eventual right-to-left shunting. Also, if a large defect is unrepaired, heart failure will ensue, usually in early adulthood. VSDs are more common in people with Down syndrome than in the general population. For more information on VSD, please watch the video below.
6.10 – Resource 03 – Khan Academy – Ventricular Septal Defect
6.10.3 Tetralogy of Fallot (TOF)
Tetralogy of Fallot (TOF) is the most common cyanosis-causing congenital heart defect. This defect is apparent at or soon after birth, as the baby will exhibit a blueish tint in the skin around the nose and mouth and in the fingernail and toenail beds (cyanosis). The condition consists of four separate defects that combine to cause significant problems with getting oxygenated blood pumped throughout the body. The first and most significant defect is pulmonary valve stenosis. The pulmonary valve is stiff and does not open completely. This causes blood to back up into the right ventricle, which in turn enlarges the right side of the heart, leading to the second characteristic, hypertrophy of the right ventricular wall. The third problem is a ventricular septal defect, which allows blood from the right and left sides of the heart to mix. The fourth issue is an aorta that overrides both the right and left ventricles, so that blood that is not well-oxygenated is sent into the general circulation. This leads to cyanosis and fatigue. TOF is more common in babies with Down syndrome. TOF is generally surgically repaired during the first year of life.
4.10 – Resource 04 – Khan Academy – Tetralogy of Fallot
If you are interested in surgical repair procedures, you can view a video on this subject at
6.10 – Resource 05 – Nationwide Children’s – Tetralogy of Fallot: Animation Explains Heart Defect and Repair
Questions for further thought:
- What is a boot sign?
- What is the mechanism behind the development of the heart condition that is associated with a boot sign?
- Why do we see cyanosis in TOF?
- Why don’t we see cyanosis in most VSDs?
6.10.4. Transposition of the Great Arteries
An infrequent and serious congenital cardiac condition is transposition of the great arteries or transposition of the great vessels. In this condition, the aorta and pulmonary artery are “switched” so that deoxygenated blood from the right ventricle is pumped into the aorta to circulate throughout the body. Oxygen-rich blood from the lungs circulates on the left side of the heart only, entering the left atrium, then into the left ventricle, then to the lungs via the pulmonary artery, and then back to the right atrium. Since deoxygenated blood is circulating throughout the body, this condition is associated with cyanosis, and requires surgical intervention within the first few weeks of life. With surgical correct, over 90% of babies go on to lead full active lives. A short video on this condition can be seen below:
6.10 Resource 06- https://www.youtube.com/watch?v=lBGUtiBp8k8&t=157s: Resource video explains the condition of Transposition of the Great Arteries.
6.11 Cardiomyopathy
A disorder of the cardiac muscle is termed a cardiomyopathy. There are many types of cardiomyopathy, some with genetic etiologies, others are acquired through infection or illness. Most are silent, that is symptom-free, at first, but can later lead to light-headedness, syncope, shortness of breath, fatigue, swelling of the lower extremities, cardiac arrhythmia, and even sudden cardiac death. The cardiac muscle can become stiff and thick, decreasing the size and elasticity of the ventricles, or distended and flimsy, thinning the ventricular walls and weakening the force of contraction. In either case, the heart will be larger than normal, and the pumping mechanism will be less effective. Depending upon the type and severity of cardiomyopathy, the patient might be treated with lifestyle changes, medications, or surgeries. Surgeries are usually intended to improve the pumping mechanism of the heart through electrical stimulation or alteration through cardiac ablation, or the implantation of a pacemaker or VAD. In severe cases, a heart transplant might be necessary.
6.12 Medications Used to Treat Disorders of the Heart and Blood Vessels
6.12.1 Angiotensin-converting enzyme (ACE) inhibitors
Angiotensin-converting enzyme (ACE) inhibitors are most often used to control hypertension or treat heart failure. They work by inhibiting enzymes that cause blood vessels to constrict, maintaining larger lumen in arteries, which maintains a lower blood pressure and decreases the workload of the heart. Some of the more common ACE inhibitors include Lisinopril (Prinivil, Zestril), Enalapril (Vasotec), Fosinopril (Monopril). The names of the generic forms of these drugs often have the “–pril” suffix.
Side effects of ACE inhibitors include light-headedness and syncope, especially when rising from supine or sitting.
6.12.2 Angiotensin-2 Receptor Blockers (ARBs)
These medications are also used in the treatment of hypertension and heart failure. They are effective in blocking the ACE receptors in the heart and blood vessels. Losartan (Cozaar), Telminisartan (Micardis), and Valsartan (Diovan) are examples of ARBs.
Side effects of ACE-2 inhibitors (ARBs) include light-headedness, dizziness and syncope, especially when rising from supine or sitting.
6.12.3 Anticoagulants
Anticoagulants are medications that decrease the blood coagulation, so that clots are less likely to form or grow. They will not break up existing clots, but they do help prevent clots from forming and may slow the growth of thrombi. They are used as a preventative measure, helping to prevent coronary artery disease, stroke, heart attack, and deep venous thrombosis and other conditions of the blood vessels. Some common anticoagulants are Heparin (various) and Warfarin (Coumadin).
With anticoagulant medications, the PTA must be careful to avoid even small injuries to the patient, as excessive bleeding or hemorrhage, internally or externally, is possible. Also, these medications can cause gastrointestinal upset. Long-term use can lead to liver toxicity.
6.12.4 Antiplatelet (Antithrombotic) Agents
Antiplatelet agents work by decreasing the cohesiveness of platelets, which are involved in the clotting mechanism of blood. These medications are most often prescribed in patients where atherosclerosis is suspected or diagnosed, but a cardiac event or stroke has not yet occurred. Aspirin and Clopidogrel (Plavix®) are the most commonly prescribed antiplatelet agents.
With antithrombotic medications, the PTA must be careful to avoid even small injuries to the patient, as excessive bleeding or hemorrhage, internally or externally, is possible. Also, these medications can cause gastrointestinal upset. Long-term use can lead to liver toxicity.
6.12.5 Beta Blockers
Beta blockers work by blocking the effects of epinephrine, which is a stimulator of the fight-or-flight response. The effects of beta blockers include slowing the heart rate and decreasing the cardiac output. These changes decrease the blood pressure and the force of contraction of the heart. Beta blockers are used to treat hypertension, cardiac arrhythmias, and angina. They are also used to help prevent future heart attacks in patients who have experienced a heart attack. Some commonly prescribed beta blockers include Metoprolol (Lopressor, Toprol XL), Propranolol (Inderal), and Nadolol (Corgard). The generic forms of these drugs often end in “-olol.”
Side effects of beta-blockers include light-headedness, dizziness and syncope, especially when rising from supine or sitting. Beta blockers also do not allow the heart rate to rise, so heart rate is not always useful to determine the exertion level of a particular exercise or activity. It is wise to use a scale of perceived exertion to determine these levels.
6.12.6 Calcium Channel Blockers
These medications block calcium from crossing the cell membranes of cells in the heart and blood vessels. The result is that the heart may not pump as strongly and the blood vessels remain more relaxed. Calcium channel blockers are used to treat high blood pressure, chest pain, and cardiac arrhythmias. Some commonly prescribed calcium channel blockers include Amlodipine (Norvasc, Lotrel), Diltiazem (Cardizem, Tiazac), and Felodipine (Plendil).
Side effects of calcium-channel blockers include light-headedness, dizziness and syncope, especially when rising from supine or sitting. In addition, peripheral edema might worsen with use of these medications, so the PTA should watch for edema and weight gain.
6.12.7 Cholesterol-Lowering (Antihyperlipidemia) Medications
Because cholesterol levels in the blood are associated with atherosclerotic plaque formation in the blood vessels, cholesterol-lowering medications can be helpful in treating coronary heart disease, heart failure, and hypertension. These medications work in the liver or intestinal tract to help decrease the amount of cholesterol, especially low-density lipoprotein, in the circulation. Statin drugs are the most frequently used of the cholesterol-lowering medications, and some of the most popular statins include Atorvastatin (Lipitor) and Rosuvastatin (Crestor).
Antihyperlipidemia medications are sometimes associated with the following side effects: headache, gastrointestinal distress, myalgia, and skin rash.
6.12.8 Diuretics
Diuretics help decrease blood pressure by helping the body remove excess water and sodium from the blood and interstitial spaces. This can help with the edema that is associated with heart failure. These medications are most often used to treat high blood pressure, heart failure, and swelling in the body. Diuretics include Furosemide (Lasix), Chlorothiazide (Diuril), and Hydro-chlorothiazide (Esidrix, Hydrodiuril). The “-ide” suffix is common in the names of the generic forms of diuretics.
Side effects of diuretics include light-headedness, dizziness and syncope, especially when rising from supine or sitting. A patient who is taking diuretics is also at risk for dehydration and electrolyte imbalances, and confusion might be a sign of these metabolic issues.
6.12.9 Digitalis Preparations (Positive Inotropic Agents)
Digitalis preparations are used to treat cardiac arrhythmia, especially atrial fibrillation and heart failure. These work by increasing the force of contraction in the heart muscle. Digoxin, Digitoxin, and Lanoxin are examples of digitalis preparations.
Side effects of these medications include cardiac arrhythmia, gastrointestinal distress, dizziness, and blurred vision.
6.12.10 Vasodilators
Vasodilators, most often nitrates, can be used to open the blood vessels in the cardiac circulation and help relieve chest pain. Nitroglycerine tablets, which are a type of nitrate, are the most common form of these medications, and they are generally administered under the tongue. Other examples include Isosorbide dinitrate (Isordil), Nesiritide (Natrecor), and Hydralazine (Apresoline).
Side effects of ACE-2 inhibitors (ARBs) include light-headedness, dizziness and syncope, especially when rising from supine or sitting.
6.12.11 Immunosuppressive Medications
Patients who have received a heart transplant or heart-lung transplant will be taking medications to depress their immune systems, in order to help prevent rejection of the new organ. Some examples of immunosuppressive medications include tacrolimus, azathioprine, mycophenolate mofetil, cyclosporine, and prednisone.
Side effects of these medications include immunosuppression, nausea and other gastrointestinal distress, liver abnormalities, kidney problems, seizures, low platelet levels, increased cholesterol levels, headache, mood swings, and weight gain.
For practice in identification of different types of medications used to control blood pressure and treat cardiac conditions, complete the exercise below:
6.13 The PTA and Cardiovascular Conditions
Many patients receiving physical therapy interventions need cardiovascular conditioning. Some have diagnosed cardiac or vascular diseases or conditions, and some have depressed cardiovascular functioning because of immobility, inactivity, or lifestyle choices. It is the responsibility of the PTA to demonstrate awareness of cardiovascular functioning in all patients by monitoring vital signs and noticing signs and symptoms of cardiovascular problems. In addition, the PTA should be knowledgeable about risk factors for cardiovascular conditions and be able to help patients make informed choices regarding lifestyle and possible interventions.
Signs and Symptoms of Cardiac Pathology or Distress
- Chest pain
- Dyspnea (shortness of breath)
- Diaphoresis (perspiration)
- Nausea
- Dizziness
- Light-headedness
- Syncope (fainting)
- Fatigue
- Cyanosis
- Edema
- Coughing
- Weight Gain
- Pain in Shoulder, Neck, Tongue
- Confusion
4.13 – Resource 01 – Signs and Symptoms of Cardiac Pathology or Distress
If a patient exhibits any of these signs, or especially if they exhibit several of these signs, the PTA should get the patient into a safely supported position, monitor the patient’s vital signs, and request assistance. If the patient becomes unresponsive or loses consciousness, immediate medical attention should be sought.
The PTA needs to be aware of the effects and the side effects of the medications prescribed for cardiac and vascular conditions. For the medications that lower blood pressure (ACE inhibitors, ACE-2 inhibitors, beta-blockers, calcium-channel blockers, diuretics), vasodilators, and positive inotropic agents, orthostatic hypotension, dizziness, and light-headedness are common side effects. The PTA needs to move the patient slowly from a supine to seated or standing position. In addition, the PTA should educate the patient to be aware of this side effect and make these transitions between positions slowly and deliberately.
Patients who are on diuretics may complain of muscle cramping or show signs or muscle weakness associated with electrolyte depletion. These symptoms could be side effects of the medications. Patients taking diuretics might also experience dizziness or light-headedness.
If a patient is taking medications to decrease blood clot formation (anticoagulants, antithrombotics), the PTA needs to be aware that any injury might cause the patient to bruise or bleed externally or internally. Also, these medications can make a patient feel nauseous or have other signs or gastrointestinal upset.
If a PTA notices any of the side effects mentioned above, and they are negatively impacting the patient’s well-being, quality of life, or progression in physical therapy, the PTA should communicate with the prescribing health-care professional so that adjustments to the medication scheme can be considered.
Patients recovering from surgical procedures to the heart or chest area need care. Any surgical incision or wound needs to be checked for signs of infection. The surgical site might be tender and the PTA should take care not to disturb or irritate the site. If the chest has been opened, in the case of open-heart surgery, sternal precautions should be observed. These include avoiding undo stress to the surgical area by avoiding upper extremity support. Patients with these surgical incisions will have difficulty using assistive devices for pulling themselves up in bed, rising to stand, and ambulating. Care should be taken when moving these patients. They will also need instruction and encouragement for deep breathing exercises and controlled coughing, using a pillow to support the chest and abdomen.
The PTA must be very careful not to expose patients who have undergone heart transplant surgery to infectious agents. Handwashing and the appropriate use of individual protective equipment (gloves, mask, gown) are extremely important when working with patients in this vulnerable population.
For a quick review, try this:
The Cardiovascular System Resources
Section 6.1
Section 6.2
Resource 01 – “File:2110 Pulse Sites.jpg” by OpenStax College is licensed under CC BY 3.0
Resource 02 – Level of perceived extersion scale – more information needed
Section 6.3
Resource 01 – Risk factors for cardiovascular disorders table – more information needed
Section 6.4
Resource 01 – General signs and symptoms of cardiac problems – more information needed
Section 6.5
Resource 01 – What is heart failure? – Khan Academy Medicine
Resource 02 – Enlargement of the Left Ventricle – “File:Right side heart failure.jpg” by Scientific Animations is licensed under CC BY-SA 4.0 .
Resource 03 – Pitting Edema – “File:Combinpedal.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0
Resource 04 – External jugular vein distension External Jugular – “File:Elevated JVP.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0
Resource 05 – Artificial Cardiac Pacemaker – “File:Herzschrittmacher auf Roentgenbild.jpg” is licensed under CC BY 3.0
Resource 06 – Ventricular Assistive Device – “File:Ventricular assist device.png” by Madhero88 is licensed under CC BY-SA 3.0
Section 6.6
Resource 01 – Ventricular Assistive Device -Coronary Arteries- “File:Coronary arteries.svg” by Patrick J. Lynch, medical illustrator is licensed under CC BY-SA 3.0
Section 6.7
Resource 01 – Fatty Deposits Fatty Deposits – “File:Blausen 0257 CoronaryArtery Plaque.png” by BruceBlaus, Blausen.com is licensed under CC BY 3.0
Resource 02 – Coronary Heart Disease – “Coronary Heart Disease with Fatty Deposits” by Harvard Health Publishing is licensed
Resource 03 – Khan Academy – What is coronary artery disease?
Resource 04 – Khan Academy – Heart Attack Pathophysiology
Resource 05 – “File:Blausen 0034 Angioplasty Stent 01.png” by BruceBlaus, Blausen.com is licensed under CC BY 3.0
Resource 06 – Coronary Artery Bypass Graft (CABG) – “File:Blausen 0152 CABG All.png” by BruceBlaus, Blausen.com is licensed under CC BY 3.0
Section 6.8
Resource 01 – Khan Academy – Electrical System of the Heart
Resource 02 – Sinus Rhythm – “File:Heart conduct sinus.gif” by is licensed under CC BY-SA 3.0 – Arterial Fibrillation – “File:Heart conduct atrialfib.gif” by is licensed under CC BY-SA 3.0
Section 6.9
Resource 01 – What is Blood Pressure? – Khan Academy – What is Blood Pressure?
Resource 02 – Blood Pressure Stages – “Blood Pressure Categories” by The American Heart Association is licensed under All rights reserved (2018).
Resource 03 – Signs of DVT – “File:Deep vein thrombosis of the right leg.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0
Resource 04 – Aneurysm –“File:Blausen 0001 AbdominalAorticAneurysm 01.png” by BruceBlaus, Blausen.com is licensed under CC BY 3.0
Resource 05 – Abdominal aortic aneurysms – Khan Academy – Abdominal Aortic Aneurysm
Section 6.10
Resource 01 – Atrial Septal Defect
Resource 02 – Atrial septal defect – “File:Atrial septal defect-en.png” by Manco Capac is licensed under CC BY-SA 3.0
Resource 03 – Atrial septal defect –Ventricular Septal Defect – Khan Academy
Resource 03 – Khan Academy – Ventricular Septal Defect
Resource 04 – Khan Academy – Tetralogy of Fallot
Resource 05 – Nationwide Children’s – Tetralogy of Fallot: Animation Explains Heart Defect and Repair
Section 6.11
Section 6.12
Section 6.13
Resource 01 – Signs and Symptoms of Cardiac Pathology or Distress
(Do we need this now? from here down?)
(Need to connect resources with the sources here )
CDC. Deaths, percent of total deaths, and death rates for the 15 leading causes of death in 10-year age groups, by race and sex: United States, 2013.
Resource 05: Cardiac Circulation – https://en.wikipedia.org/wiki/Coronary_circulation
Resource 09: Blausen.com staff (2014). Stent https://en.wikipedia.org/wiki/Stent#/media/File:Blausen_0034_Angioplasty_Stent_01.png
“Medical gallery of Blausen Medical 2014“. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. – Own work
Resource 10: C.A.B.G https://upload.wikimedia.org/wikipedia/commons/6/68/Blausen_0152_CABG_All.png
Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014“. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. – Own work
Resource 12: Pacemaker xray
https://commons.wikimedia.org/wiki/File:Herzschrittmacher_auf_Roentgenbild.jpg
Resource 14: A.H.A http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/KnowYourNumbers/Understanding-Blood-Pressure-Readings_UCM_301764_Article.jsp#.W0O-bNOWw2w
Resource 15: (altered from original image) https://commons.wikimedia.org/wiki/File:Mean_arterial_pressure.png
Resource 16: arrhythmia types (Just good info on types of arrythmia)
Resource 17(DVT): By James Heilman, MD – Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=9444797
Resource 18 (AAA): By BruceBlaus. When using this image in external sources it can be cited as:Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. – Own work, CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=28761793
Resource 20 (A.S.D): https://en.wikipedia.org/wiki/Atrial_septal_defect
Resource 21 (VSD):V.S.D
Attribution: Manco Capac
Resource 22 (Osmosis) https://www.youtube.com/watch?v=uHv2RHnTpJg
This video is licensed under a Creative Commons CC-BY-SA 4.0 international license, which means that you’re free to share and adapt it so long as you follow the Attribution and ShareAlike terms and conditions!
Credits:
Script/audio/visuals: Tanner Marshall, MS
Reviewer: Rishi Desai, MD, MPH
Attributions:
Boot-shaped heart radiograph by Dr. Vincent Tatco – http://radiopaedia.org/cases/tetralog…
Retro video-game sweep sound effect by ‘Timbre’ – https://www.freesound.org/people/Timb…
Resource 23 (Kahn Academy V.S.D): https://www.youtube.com/watch?time_continue=3&v=lZSi0xifXwc
Resource 24 (T.O.F) https://commons.wikimedia.org/wiki/File:Bluebaby_syndrom-IT.png
(Need to connect resources)

