Chapter 16: Oncology
Learning Objectives
After completing this chapter, the learner should be able to:
- Define the basic terminology associated with cancer.
- Discuss current theory on the development of cancer.
- Discuss etiology and risk factors for selected cancers.
- Differentiate between normal cells and cancer cells.
- Differentiate between malignant tumors from benign tumor.
- Discuss clinical manifestations of selected cancers.
- Describe staging and grading of cancer and implications for treatment.
- Discuss the medical management of cancer, including prevention.
- Identify warning signs of potential cancer.
- Discuss PT interventions that are appropriate and inappropriate for patients with cancer.
Chapter Contents
16.0 Oncology
Cancer is not just one disease, but a group of many different conditions that can affect different organs and body systems. Some cancers are curable, some manageable, and some fatal. Risk factors are known for some and not known for others. Cancer is a complex issue that will be covered in general terms in this chapter. We will examine current theory, medical management, and physical therapy involvement in selected cancerous conditions.
For a very basic introduction to cancer, view this YouTube video.
“Oncogenetics – Mechanism of Cancer | Cells | MCAT | Khan Academy” by Khan Academy is licensed under CC BY 4.0
16.1 General Risk Factors for Cancer
There are some general risk factors for cancer, and many cancers also have specific risk factors. Some of these will be discussed in the sections on specific types of cancer later in this chapter or elsewhere in this book. Some general risk factors have been identified and are categorized as “modifiable” or “nonmodifiable.” Modifiable risk factors are those we are able to control, while nonmodifiable risk factors, such as age, are beyond our control.
Most Studied and Agreed Upon Risk Factors for Cancer
Source: NIH: Risk Factors for Cancer
Some cancers include a hereditary component. It is estimated that 5-10% of all cancers can be labeled “hereditary cancer syndromes,” meaning that the genetic mutation causing the cancer is carried in genes that are passed from parent to child. Genetic tests are available to identify some hereditary forms of cancer. (Source: The Genetics of Cancer)
Some cancers are linked to viral infection. For example, human papilloma virus (HPV) is associated with the development of cervical cancer in women and hepatitis is associated with the development of liver cancer.
16.2 Etiology of Cancer
Cancer starts with a mutation, or abnormality, in one cell. This mutation is passed on to daughter cells through mitosis. The mutation allows this cells and all its offspring to grow and reproduce without regulation from mechanisms inside or outside the cell. Inside the cell, proto-oncogenes can facilitate the production of oncogenes (cell capable of causing cancer through uncontrolled reproduction). Also, tumor suppressor genes, which normally turn-off cellular growth and reproduction can be diminished in number or in effect. This can form a tumor in an organ or destroy the normal balance of different types of cells in the blood stream or lymphatic system. There are three separate checkpoints during cellular life where the reproduction of the cell can be stopped and the cell can be destroyed. If these three checkpoints fail to recognize problems in the DNA or fail to achieve the appropriate cellular response, which is ceasing the reproductive cycle of the cell, the resulting genetic mutation can cause a cell to become cancerous.Apoptosis (pre-programmed cell death)is diminished or turned off completely and/or regulatory T-cells unable to stop the uncontrolled cell replication. The following video gives a thorough explanation of the development of cancerous cells through mutation. The video contains more detail than will be covered in this course, but it is helpful to see the whole picture in attempting to gain understanding of the mechanisms involved in the development of cancer.
“Oncogenetics – Mechanism of Cancer (tumor suppressor genes and oncogenes)” by Armando Hasudungan is licensed under CC BY 4.0
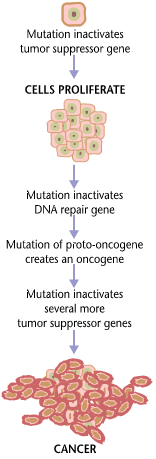
Long Description
Title: Cancers are caused by a series of mutations.
An illustrated flow chart contains these steps:
- Mutation inactivates tumor suppressor gene
- CELLS PROLIFERATE
- Mutation inactivates DNA repair gene
- Mutation of proto-oncogene creates an oncogene
- Mutation inactivates several more tumor suppressor genes
- CANCER
16.3 Benign and Metastatic Tumors
Tumors can occur anywhere in the body and they can be separated into two large groups: cancerous (metastatic) or benign. A benign mass of cells is a tumor, but it is not cancerous. The cells in a benign tumor may be abnormal, as they do not belong where they are occurring and there are many of them, but they resemble body cells and they do not spread to other areas of the body. A benign tumor can be dangerous if it occurs in a part of the body where surgical removal is risky or not possible, such as some areas of the brain. If a benign tumor gets large and exerts pressure on surrounding tissue, limiting or shutting off its function, it can be fatal. Most benign tumors are not fatal, however, and most are able to be removed through surgical intervention.
Cancerous tumors are different. Cancer cells do not behave like normal body cells. While normal body cells participate in functions that help the organ function as a whole, cancer cells seem to function only to replicate themselves, starving the surrounding normal cells of essential blood supply and nutrients. Cancer cells are much less cohesive than normal cells, so they break off easily, which makes them able to travel to other sites within the body. In addition, many cancer cells secrete substances that help break down blood and lymphatic vessel walls, allowing the cancer cells to enter the blood stream and lymphatic system and move freely about the body. This is the metastatic nature of cancer.
The typical steps in metastasis are: (1) local invasion (cancer forming at the primary site, invading adjacent tissues); (2) intravasation (cancer cells invading the blood vessels or lymphatic vessels and traveling throughout the body); (3)extravasation ( cancer cells breaking through vessel walls and entering new body tissue; (4) proliferation (reproduction of new cancerous cells in new area) and (5) angiogenesis (creating a network of blood vessels to feed the new tumor). Cancer can begin in one area of the body, say the breast, and then move to the circulatory or lymphatic systems to infect axillary lymph nodes and then lung tissue. In this case we would have a primary cancer site, the breast, and a secondary site, the lung. Once cancer has metastasized, it can cause cancer anywhere in the body. For this reason, it is important to identify the primary source early and treat it as completely as possible before it metastasizes. Screenings and tests are available for many types of cancer to help discover early signs of abnormal cells or abnormal growths. Colonoscopy and breast imaging through mammography are examples of widely utilized cancer screening tests.
” Search 9+ Avatar image 0:03 / 1:48 Metastasis: How Cancer Spreads” by National Cancer Institute is licensed under CC BY 4.0
Of course, some cancers do not produce tumors at all. Cancers of the blood and lymphatic systems cause complete disruptions of circulation and the supply of oxygen and nutrients to all parts of the body, as well as removal of waste and excess fluid. Leukemia and lymphoma are examples of these types of cancer. These disorders are discussed in the chapter on the Hematologic and Lymphatic Systems.
16.4 Diagnostic Methods for Cancer
Depending upon the type of suspected disease or disorder, different diagnostic methods are available. Masses, or tumors, can sometimes be felt or seen during a physical exam. Other times, radiographs (x-rays) , CT scans, MRI scans, mammography, or ultrasound can be used to visualize growths . Body fluids, such as blood and cerebrospinal fluid, can also be tested in a laboratory to determine the presence of abnormal cells. Markers of increased metabolism found in blood work can indcate increased metabolism or inflammation that could be associated with cancer. Tissue can be removed and sent to a lab for biopsy to determine if cells are cancerous, and if so, determine the type of cancer. Fine needle aspiration or surgical excision of tissue can be employed to attain tissue to be biopsied. Suspicious cells found in tests, such as colonoscopy or pap smear, can be analyzed for abnormalities.
16.5 Staging and Grading of Tumors
16.5.1 Staging
Staging is the most common categorization scheme for cancer. Staging is implemented to determine prognosis and appropriate intervention. The Tumor, Nodular, Metastasis (TNM) method is commonly used to determine the stage of cancer. In TNM tool, the size of the tumor, the lymph node involvement, and the absence or presence of metastases are evaluated and combined to determine the level of progression, prognosis, and medical intervention. Each component is listed in the description, so a particular cancer could be labeled, T1N2M0, meaning it is a small tumor, 2 lymph nodes show presence of cancer, and no metastases are present.
16.5.1.1 Primary tumor (T)
- TX: Main tumor cannot be measured.
- T0: Main tumor cannot be found.
- T1, T2, T3, T4: Refers to the size and/or extent of the main tumor. The higher the number after the T, the larger the tumor or the more it has grown into nearby tissues. T’s may be further divided to provide more detail, such as T3a and T3b.
16.5.1.2 Regional lymph nodes (N)
- NX: Cancer in nearby lymph nodes cannot be measured.
- N0: There is no cancer in nearby lymph nodes.
- N1, N2, N3: Refers to the number and location of lymph nodes that contain cancer. The higher the number after the N, the more lymph nodes that contain cancer.
16.5.1.3 Distant metastasis (M)
- MX: Metastasis cannot be measured.
- M0: Cancer has not spread to other parts of the body.
- M1: Cancer has spread to other parts of the body.
Source: Cancer Staging
16.5.2 Grading
Cancerous lesions can also be described through grading, which is different from staging. The grade refers to the type of cells in the abnormal mass or tissue. If, microscopically, the cells resemble normal body cells, the grade is low, usually meaning a better prognosis than if the grade is high. A high grade means the cells are poorly differentiated, or lack little resemblance to normal body cells.
- GX: Grade cannot be assessed (undetermined grade)
- G1: Well differentiated (low grade)
- G2: Moderately differentiated (intermediate grade)
- G3: Poorly differentiated (high grade)
- G4: Undifferentiated (high grade)
Source: Tumor Grade
There are several other staging and grading methods for cancer, some specific to certain types of cancer. It is beyond the scope of this text to discuss all staging and grading methods.
16.6 Medical Management of Cancer
Some cancer treatments are specific to the type of cancer, but general management includes surgical intervention, chemotherapy, and radiation. Hormonal therapies are useful with some types of cancer. Other methods that are used include immunotherapy, targeted therapy, stem cell transplant, and precision medicine. For some types of cancer in advanced stages, palliative treatments may be the best option.
16.6.1 Surgery
Surgical removal of the cancerous cells offers the most positive prognosis in most cases. If the cancerous cells are removed from the body, the cancer could be cured. Depending on the location, size, and type of cancerous mass, surgeries can be performed using either local or general anesthesia. In addition, surgeries can be performed in traditional methods, using scalpels and other tools, or growths can be removed in whole or in part through cryosurgery (freezing), lasers, hyperthermia (burning), or photodynamic therapy, where drugs are used in conjunction with light to target cancerous cells. Risks associated with surgery include post-surgical pain and infection. Since it is often difficult to determine if all cancer cells have been removed through surgical excision, surgical interventions are often used in conjunction with other treatments, such as radiation and chemotherapy.
16.6.2 Radiation
Radiation treatments are used to kill cancer cells. Radiation, like chemotherapy, can also damage healthy tissue. It is more focused than chemotherapy, so it is less likely to make a person feel ill. It does affect the immune response, so it is important to keep exposure to potential pathogens to a minimum. Radiation therapy can be in the form of external beam radiation, in internal radiation therapy, where liquid or solid forms (brachytherapy) of radiation are introduced inside the body. Radiation kills or shrinks cancer cells, but can also have detrimental effects on healthy cells. Radiation therapy can cause many different side effects, depending upon the site being radiated. Some of the most common side effects include immunosuppression, fatigue, nausea and vomiting, anemia, hair loss, and skin changes. The skin changes should be of particular concern to PTAs. The skin thins and becomes highly susceptible to damage through radiation, so it is at risk for pressure ulcers, tears, and lacerations. Thermal modalities should not be used on the skin affected by radiation for one year following radiation therapy.
16.6.3 Chemotherapy
Specialized drugs are used to treat cancer. There are often several drugs employed at the same time in order to kill as many cancerous cells as possible. These drugs target cancerous cells, but often also kill other healthy cells.
Chemotherapy may be given in many ways. Some common ways include:
- Oral
The chemotherapy comes in pills, capsules, or liquids that you swallow - Intravenous (IV)
The chemotherapy goes directly into a vein - Injection
The chemotherapy is given by a shot in a muscle in your arm, thigh, or hip, or right under the skin in the fatty part of your arm, leg, or belly - Intrathecal
The chemotherapy is injected into the space between the layers of tissue that cover the brain and spinal cord - Intraperitoneal (IP)
The chemotherapy goes directly into the peritoneal cavity, which is the area in your body that contains organs such as your intestines, stomach, and liver - Intra-arterial (IA)
The chemotherapy is injected directly into the artery that leads to the cancer - Topical
The chemotherapy comes in a cream that you rub onto your skin - source: NIH: Chemotherapy to Treat Cancer
Most people who are undergoing chemotherapy treatments feel tired and sometimes ill. The drugs used in chemotherapy are very strong. A person who is undergoing chemotherapy treatments is highly susceptible to infection. For this reason, it is important that they not be exposed to potential sources of infection, such as people who are sick or food that might be contaminated. Other side effects of chemotherapy include nausea and vomiting, fatigue, anemia, hair loss, anemia, appetite loss, and lymphedema.
16.6.4 Immunotherapy/ Biological Therapy
The body’s immune system can provide powerful responses to invasion by cancerous cells. Immunotherapy helps boost the infection-fighting cells (particularly the Killer T-cells) so that the immune system can be more effective in stopping the uncontrolled cell division associated with cancer. Skin changes, flu-like symptoms, and pain or irritation at the needle site are common side effects for immunotherapy treatments.
16.6.5 Stem Cell Transplant
Stem cells are cells that can grow into red blood cells, white blood cells, and platelets. They can retrieved from the individual receiving the transplant or from another person who is matched with the recipient. An identical twin is an ideal donor. Stem cells are retrieve from the blood stream, bone marrow, or umbilical cord from the donor and injected into the vein of a recipient. The new, healthy stem cells stimulate growth of healthy blood cells in the recipient. Stem cell transplants are often used to directly fight cancer in multiple myeloma, lymphoma or leukemia. they can also be useful in replenishing weakened blood supplies in individuals who have undergone intensive chemotherapy and/or radiation therapy for any kind of cancer.
16.6.6 Antiangiogenic Therapy
Several different types of drugs can be used in this type of treatment, with the goal of suppressing blood supply to cancerous cells. Antiangiogenic therapy seems to have success in slowing or stopping the growth of cancer, but has less of an effect on eliminating or curing cancer. Newer forms of antiangiogenic therapy are being explored using genetically altered bacteria to transport antiangiogenic substances to cancerous sites. Hypertension and hemorrhage are common side effects of this type of treatment. Other less common side effects include skin changes, fatigue, and diarrhea.
16.6.7 Targeted Therapy
Targeted therapy is the foundation of precision medicine. It is a type of cancer treatment that targets proteins that control how cancer cells grow, divide, and spread. As researchers learn more about the DNA changes and proteins that drive cancer, they are better able to design promising treatments that target these proteins. Most targeted therapies are either small-molecule drugs or monoclonal antibodies. Most of these therapeutic interventions require biopsy and analysis of the tumor, so that the intervention may be specific and unique to the tumor being treated. Research has identified many different targeted therapy options, but for many types of cancer, targeted therapy options are still being studied and no effective treatment is available at this time. Cells can also become resistant to targeted therapy interventions over time, so the effectiveness may be short-lived. The most common side effects of targeted therapy include diarrhea and liver problems. Other side effects might include problems with blood clotting and wound healing, high blood pressure, fatigue, mouth sores, nail changes, the loss of hair color, and skin problems.
“IMMUNOTHERAPY: The Path to a Cancer Cure (For Clinicians)” Society for Immunotherapy of Cancer is licensed under CC BY 4.0
16.7 Specific Cancers
16.7.1 Bone Cancer
Bone is not often a primary cancer, but is frequently a site for metastasis. Bone cancer is rare and includes several types. Some bone cancers, including osteosarcoma and Ewing sarcoma, are seen most often in children and young adults. Pain is the most common symptom of bone cancer, but not all bone cancers cause pain. Persistent or unusual pain or swelling in or near a bone can be caused by cancer or by other conditions. Other symptoms of bone cancer include a lump (that may feel soft and warm) in the arms, legs, chest, or pelvis; unexplained fever; and a bone that breaks for no known reason. Bone cancer can be treated with a range of options listed above, additional options of amputation and limb-sparing bone removal surgeries.
16.7.2 Brain Cancer
Primary brain cancer may arise from astrocytes, meninges, nerve cells, or tissues within the brain. The brain is also a common site for metastases from primary cancers in other organs. Signs and symptoms,treatments, and prognoses for different of brain tumors vary with the tumor type, location, grade, and stage. Surgical resection along with radiation and other combined therapies are the most commonly indicated therapies.
16.7.3 Breast
Breast cancer is the most common cancer in females, but is should be remembered that breast cancer can also occur in men. Breast cancer is the second most common fatal cancer in women. There are several identified risk factors for breast cancer. These included family history and genetics, age, increased breast density, obesity, smoking, prolonged exposure to estrogen (early onset of menses and/or late menopause, hormone replacement therapy (HRT)), exposure to radiation, and alcohol use. Most breast cancers arise from epithelial tissue (adenocarcinomas). Detection and diagnostic measures include physical exam (self-exam and health care provider exam) and mammography. Treatments include surgical excision, radiation therapy, and hormone adjustment. The cure rate is greater than 90% if the cancer is sucdessfully treated prior to metastasis. If breast cancer is not treated prior to metastasis, common secondary sites include the lymph nodes, lung, bone, skin, and brain.
16.7.4 Bronchial Carcinoma
Bronchial carcinoma is an epithelial carcinoma occurring in the lining of the bronchopulmonary tree. The major risk factor for developing this type of cancer is smoking. There are two broad categories of bronchial carcinoma: small cell carcinoma and non-small cell carcinoma. Non-small cell carcinoma includes adenomas and various types of carcinomas, all derived from epithelial tissue. Signs and symptoms do not typically emerge until the cancer is in an advanced stage, so prognosis can be unfavorable, depending upon the type, stage and grade of teh cancer. Surgical intervention, chemotherapy, and radiation therapy are commonly utilized treatments.
16.7.5 Colorectal Cancer
Colorectal cancer is one of the most deadly cancers in men and women. If caught early, however, the prognosis is good. Colonoscopy is recommended for everyone over the age of 50 and for some with risk factors, earlier in life. Risk factors for colorectal cancers include age, history of polyps, Chron’s disease, ulcerative colitis, family history, and a high-fat, low-fiber diet. Unfortunately, colorectal cancer does not show early warning signs, so by the time symptoms appear, the cancer is usually in an advance stage. Signs and symptoms include changes in bowel habits, bleeding from the rectum, fatigue, unexplained weight loss, and anemia. Treatment options include surgical resection of the involved portion of the bowel, often with resultant colostomy, radiation and/or chemotherapy.
16.7.6 Lung Cancer
Lung cancer is the single most deadly cancer for both men and women in the United States. Once developed, it rapidly metastasizes and spreads through the circulatory system to other parts of the body. Risk factors for lung cancer include smoking, exposure to environmental toxins, occupational hazards, and family history. Signs and symptoms include: cough,sputum, dyspnea, abnormal breath sounds, hemoptysis, and chest pain. Lung cancer can be treated with surgery, radiation therapy, chemotherapy, or a combination of interventions.
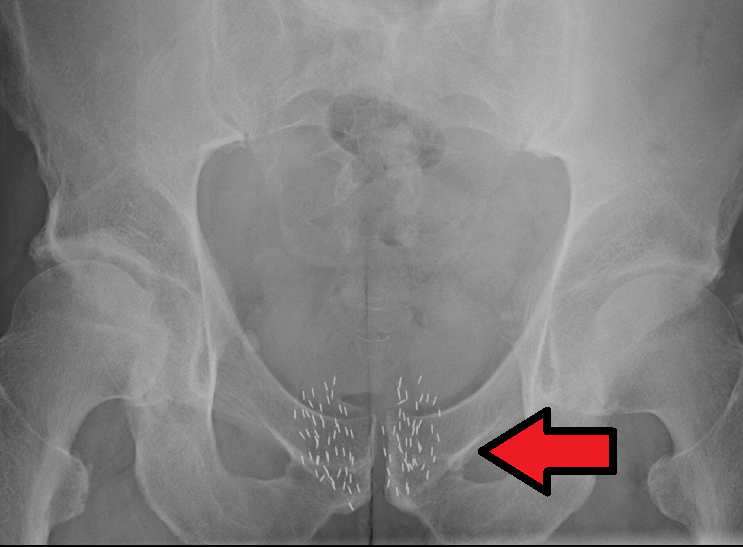
16.7.7 Prostate Cancer
Prostate cancer ranks 2nd in death rates from cancer for men. Usually adenocarcinoma, prostate cancer typically affects men over 50 years old. Several risk factors have been identified for prostate cancer. These include: age, high fat diet, genetic predisposition, African-American descent, and exposure to cadmium. Diagnosis is made through biopsy and prognosis is generally good. Signs and symptoms , which do not usually become evident until late in the disease, include urinary flow obstruction, urgency, pain, and decreased urine flow. Treatment is most often surgery, which can be supported with radiation and hormonal therapy.
16.8 Cancer and Physical Therapy
People who have cancer, or are undergoing treatments for cancer can benefit from physical activity and physical therapy is good method for safely gaining physical strength and returning to previously enjoyed activities. Several precautions are necessary to remember when working with a patient with cancer in physical therapy.
- Patients could be immunocompromised because of treatments or low white blood cell counts. These patients should not be exercising in a busy gym or exposed to a person who is ill.
- Patients who have undergone radiation therapy will have integumentary changes that cause the skin to be easily damaged and slow to heal. They should not be treated with thermal modalities.
- Patients who have cancerous lesions in the bone are at risk for fracture.
- Patients who are undergoing any kind of cancer treatments are likely to be easily fatigued and could be experiencing nausea, vomiting, or other body system dysfunction. Exercise programs need to be gentle and progressed slowly, keeping patient tolerance in mind.
- Patients who are recovering from surgery for breast cancer should be instructed in ROM activities for the upper extremity. They should also be monitored for signs of lymphedema. Lymphedema is a risk for all patients who have had cancer, but is especially prevalent in those patients with breast cancer.
- Aquatic therapy can pose a risk for any patient with unhealed surgical incisions or those with colostomies.
For a good article on the effects of physical activity on patients with cancer, please read the Physiopedia entry: Physiopedia: Physical Activity in Cancer

