Chapter 9: Degenerative Neurological Disorders
Learning Objectives
After completing this chapter, the student should be able to explain and discuss the etiologies, sign and symptoms, pathophysiology, interventions, and prognoses for each of the following conditions:
- Amyotrophic Lateral Sclerosis (ALS)
- Parkinson Disease’s Disease (PD)
- Multiple Sclerosis (MS)
- Alzheimer’s Disease (AD)
- Huntington’s Disease (HD)
- Friedreich ataxia (FA)
- Spinal Muscular Atrophy (SMA)
- Dystonia
Chapter Contents
9.1 Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic Lateral Sclerosis (ALS), often called Lou Gehrig’s Disease. is a neurological condition that affects both upper and lower motor neurons. Early in the disease, only one limb may be affected, but as the condition progresses, all limbs will be involved. Voluntary movement of the limbs and trunk becomes difficult, and then impossible. Chewing and swallowing function, speaking, and eventually breathing are also affected. Most people are in their 50s or 60s when diagnosed and the median survival rate is 2 years. There are some forms of ALS in which the survival rate is longer. These forms are less common and have an earlier age of onset. Overall, ALS is considered a relatively rare disease affecting 1 or 2 per 100,000 in the United States.
Since the motor neurons die in ALS in the spinal cord, brainstem, and brains of people with ALS, they experience both lower motor neuron symptoms (weakness, fasciculations) and upper motor neuron symptoms (spasticity, positive Babinski reflex). For a review of upper and lower motor neurons, watch the videos below:
9.1 – Resource 01 – “Motor neurons | Muscular-skeletal system physiology | NCLEX-RN | Khan Academy”
9.1 – Resource 02 – “Upper motor neurons | Organ Systems | MCAT | Khan Academy”
For information on lower motor neurons and motor units, please view the Khan Academy video: Traumatic Brain Injury – Diffuse Axonal Injury (DAI).
Demyelination, axonal swelling, and atrophy within the cerebral cortex, premotor areas, sensory cortex, and temporal cortex cause the symptoms of ALS. In some forms of ALS, dementia is part of the disorder, but those forms are less common than classic ALS.
For 90% of the cases of ALS, there is no known cause. For approximately 10% of the cases a familial link has been established. There have been many environmental factors researched to find a correlation to ALS. Overall, the research has been mostly inconclusive in connecting ALS with exposure to cigarette smoking, exposure to lead or other metals, farming chemicals, military service, and physical activity. There could be some correlation to professional sports, such as soccer and football, but it is difficult to establish a direct correlation, since chronic traumatic encephalopathy (CTE), which is the result of numerous mild and moderate brain injuries, is a close mimic of ALS.
The course of the disorder begins with weakness (patients often report “clumsiness”) of one or two extremities. They may notice they are unable to maintain grasp on objects, or they might be tripping often. The symptoms start distally and progress proximally. Neurological changes occur in the spinal cord, progressing both superiorly and inferiorly over time.
ALS is diagnosed through patient history, electromyography (EMG) and nerve conduction velocity (NCV) tests, muscle biopsy, spinal tap, and CT scan.
There is no cure for ALS. The medication that used to prolong life for a few months is riluzole (Rilutek), which appears to slow the destruction of the motor neurons. Symptomatic relief can be attained through prescriptions for muscle relaxants and antidepressants. Non-invasive ventilation (NIV) is most commonly used to help with breathing difficulties. If NIV is unsuccessful, invasive techniques (tracheotomy) is used.
Physical therapy is an important aspect of treatment of ALS. Maintaining functional abilities is the primary goal of PT. Strengthening of muscles, particularly trunk muscles that help with breathing, is very important for patients with ALS. Breathing exercises, conditioning activities, overall strengthening and range of motion activities are all important components of a PT program. Patients also need assistance with mobility, canes, crutches, walkers, wheelchairs, splints, and braces might be useful to help maintain mobility. Caregivers also need to be considered. Transfer techniques, bed mobility, and general assistance with activities of daily living should be included in the plan of care.
Patients with ALS are at risk for pressure injuries, so preventative measures (position changes, appropriate bed and seating choices) need to be addressed. If a pressure injury does develop, wound care needs to be a high priority. Choking and aspiration pneumonia are also common with ALS, and the PTA needs to be aware of swallowing difficulties. Care should be taken with feeding activities. Speech and language pathologists and occupational therapists often work with patients in these areas.
Khan Academy Video on ALS:
9.1 – Resource 03 – “ALS – Amyotrophic lateral sclerosis | Miscellaneous | Heatlh & Medicine | Khan Academy”, Khan Academy is licensed under Fair Use
Check Your Knowledge
Answer each of the following questions about ALS
9.2 Parkinson’s Disease (PD)
Here’s a short video on Parkinson’s disease that discusses the main characteristics of the disorder. It shows patients and their movement patterns.
9.2 – Resource 01 – “ALS – Amyotrophic lateral sclerosis |What are the symptoms of Parkinson’s Disease? – Ask the Experts” by ButlerHospital is licensed under Fair Use
Parkinson’s disease (PD) is a progressive degenerative neurological disorder that causes difficulties with movement, namely: tremor, rigidity, bradykinesia, and balance disorders. These symptoms are present in the extremities and in the muscles of the face, head, and neck, so that dysphagia and dysarthria are often present. In addition, other symptoms include depression, memory loss, and concentration difficulty. The cause of Parkinson may be in part, genetic. It may well be multifactorial in etiology as other known risk factors are increased age, history of concussions, and exposure to cleaning chemicals or heavy metal particles. Parkinson’s Disease affects men more often than women. People who smoke and/or consume caffeine have a lower risk for developing PD, although the correlation has not been explained. Physical activity in mid-life is also seemingly protective against PD. While most patients are diagnosed with PD around the age of 60 years, some patients have a form of Parkinson’s called young-onset or early-onset Parkinson’s disease, and they are diagnosed at much younger ages.
Parkinson’s Disease is the most common cause for the group of symptoms called “parkinsonism” (resting tremor, bradykinesia, muscular rigidity, and postural instability). Parkinsonism can be cause by other factors including head injury and some medications.
The problem with PD is that the neurons in the substantia nigra, which normally produce dopamine, begin to die. A build-up of proteins into abnormal structures, called Lewy bodies, occurs in the cells of the substantia nigra, and the cells die. Dopamine levels decrease gradually over time as more and more cells die. The mechanism for causing the Lewy body formation and the cell death is not known. The lack of dopamine causes the classic motor symptoms of PD: tremor, bradykinesia, muscular rigidity, and coordination and balance difficulties.
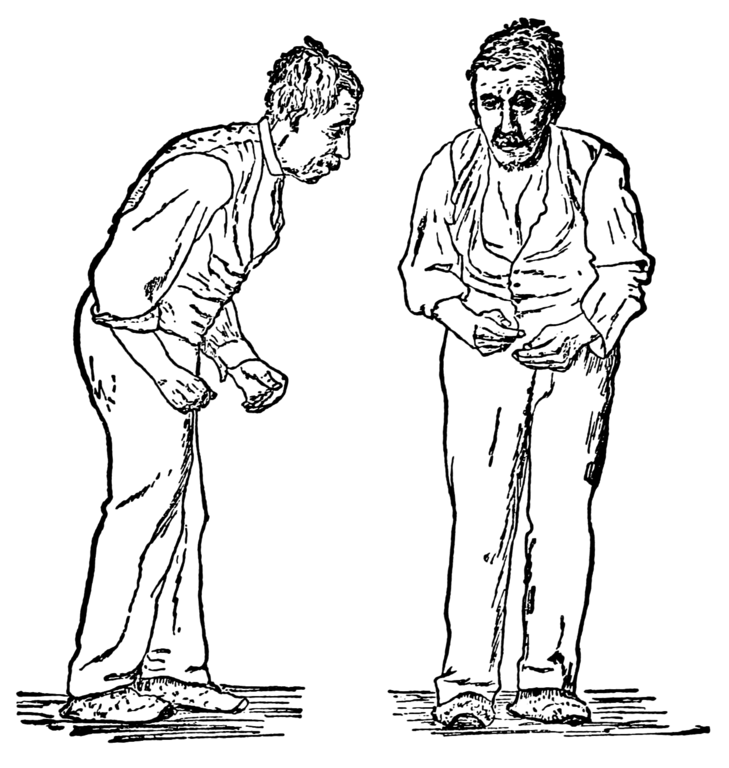
Parkinson’s Disease is quite debilitating. Patients have difficulty initiating movement. They are unstable when walking, and they develop a shuffling gait pattern. Turning to the right or left while walking is problematic. Muscles become rigid, and posture becomes “crouched” (kyphotic with hip and knee flexion). Trunk rotation and arm swing diminish over time and completed disappear later in the disease process. Talking, chewing, and swallowing are problematic and the face lacks expression, as the facial muscles appear to be frozen. The life expectancy for a person with PD is quite variable, with the average being 10 years after diagnosis. People with you-onset PD often live longer.
Medical treatment for PD includes drugs to replace dopamine (levodopa or L-dopa), drugs to increase dopamine production (dopamine agonists), and drugs that prevent the breakdown of dopamine in the central nervous system (MAO-B inhibitors). Surgery is sometimes an option for patients for whom medication is not tolerated or not effective. Deep brain stimulation surgery involved implanting a neurotransmitter in the brain to stimulate parts of the brain that are inactive because of dopamine depletion.
Physical therapy is very important for patients with PD. Range of motion, stretching, gait training (with or without an assistive device), balance training, and general endurance-building exercises are useful. For best results, PT should be scheduled around the patient’s medication cycle. In later stages of the disease, breathing might become difficulty, so PT could focus on diaphragmatic breathing and chest expansion. Occupational therapy and speech-language pathology may also be involved in the treatment team for patients with PD.
Red area is substantia nigra
Watch the following videos to get a better understanding of Parkinson Disease.
9.2 – Resource 04 – “What is Parkinson’s disease? | Nervous system diseases | NCLEX-RN | Khan Academy” by khanacademymedicine is licensed under Fair Use
9.2 – Resource 05 – “Putting it all together – Pathophysiology of Parkinson’s disease | NCLEX-RN | Khan Academy” by khanacademymedicine is licensed under Fair Use
Check Your Knowledge
Answer each of the following questions about Parkinson disease.
9.3 Multiple Sclerosis (MS)
Multiple Sclerosis (MS) is an autoimmune disease that affects the neurological system. Specifically, it causes inflammation and demyelination throughout the central nervous system. It affects many parts of the brain, brain stem and spinal cord. These areas of inflammation and destruction show up as lesions, or plaques, in radiographs. The etiology of the disease is unknown, but a genetic predisposition exists, and other risk factors include living north of the equator, being female, and being of northern European dissent. Other possible causative factors might include viral infection, smoking and stress.
The first symptoms many people with MS notice are visual disturbances, including visual acuity, color vibrancy, and eye movements. Other problems include sensory abnormalities (paresthesia, numbness, pain), motor control problems (peripheral muscles, bowel and bladder, and sexual function), and cognitive difficulties. The course of MS is variable, depending upon the type of MS.
- Clinically isolated syndrome (CIS)
- One incidence of MS-like symptoms; 30-70% progress to Relapsing-Remitting
- Relapsing-remitting MS (RRMS)
- Clear unpredictable exacerbations (attacks) and remissions; slow progression over time; most common type (80%)
- Primary progressive MS (PPMS)
- No clear periods of remission (10-20%)
- Secondary progressive MS (SPMS)
- Most people (60%) of those initially diagnosed with RRMS progress to SPMS after 15-20 years; slow decline, no real remission
Although MS is not a fatal disease, people with MS are more susceptible to other disorders, such as infection, because of immunosuppression, and pneumonia, heart disease, and other disorders associated with decreased mobility in later stages. The disorder is very debilitating for most people, as they may progress from independent ambulation, to use of cane, crutches, and walker, to wheelchair mobility only.
PTs and PTAs can help individuals with MS maintain muscular strength, mobility, and independence through range of motion exercises, gait training, and assistive device incorporation. Fatigue may be a factor in physical therapy sessions, particularly in warm weather, so treatment sessions should be scheduled accordingly.
Medical management includes corticosteroids (injected or oral) to manage attacks. There are several disease-modifying agents available to treat MS, as well. There is no cure for MS, but some medications are associated with fewer and less damaging attacks in the disease process.
Watch the following Khan Academy video on MS:
9.3 – Resource 01 – “What is multiple sclerosis? | Nervous system diseases | NCLEX-RN | Khan Academy” by khanacademymedicine is licensed under Fair Use
9.3 – Resource 02 – “Multiple sclerosis signs and symptoms | Nervous system diseases | NCLEX-RN | Khan Academy” by khanacademymedicine is licensed under Fair Use
Check Your Knowledge
Answer each of the following questions about multiple sclerosis.
9.4 Alzheimer Disease (AD)
Alzheimer disease (AD) is a degenerative disease of the brain, which affects the ability to form new memories, recall older memories, perform motor tasks, communicate, and perform self-care activities. As the average lifespan of people has increased, so has the incidence of AD. It is the most common form of dementia, but it is important to recognize that it is not the only possible cause of dementia.
There are two types of AD: familial and sporadic. The familial type is often referred to as “early-onset AD” and develops and progresses at much younger ages than does the sporadic type. Specific dominant genes have been identified with familial types of AD. One subcategory of familial-type AD is associated with trisomy 21 (Down syndrome). There are other subcategories as well, but all develop in middle adulthood and progress rapidly. Familial types of AD account for about 5-10% of AD cases.
The majority people with AD are affected by the sporadic type of AD. Although, there is no known cause for this type of AD, a genetic link has been identified in patients with sporadic AD. Age is one clear risk factor for the development of sporadic AD, as it is diagnosed in approximately half of all individuals over the age of 85. Other risk factors for developing AD include head injuries, depression, sleep deprivation, and hypertension. Some studies have suggested regular physical exercise, mental exercise (education, reading, intellectual stimulation) and a diet low in saturated fat and simple carbohydrates can help reduce the risk of AD.
Alzheimer disease follows a progression of symptoms, but rate of the development of these symptoms varies. Most people first notice short term memory loss, then motor skill and language difficulties, then long term memory loss and disorientation. In the final stages of AD, patients become bedridden, unable to perform any self-care activities. They usually die from an infection, most often from a pressure injury or pneumonia.
The pathophysiology of the disorder is the result of main changes in the brain tissue: (1) neurofibrillary tangles inside the neurons and (2) amyloid plaques outside the neurons. The video below gives a clear explanation of changes in the brain that occur because of AD. This link goes to an NIH page that includes a transcript of the video and links to other information about AD.
Watch video on how Alzheimer’s changes the brain.
9.4 – Resource 01 – How Alzheimer’s Changes the Brain NIH: National Institute on Aging
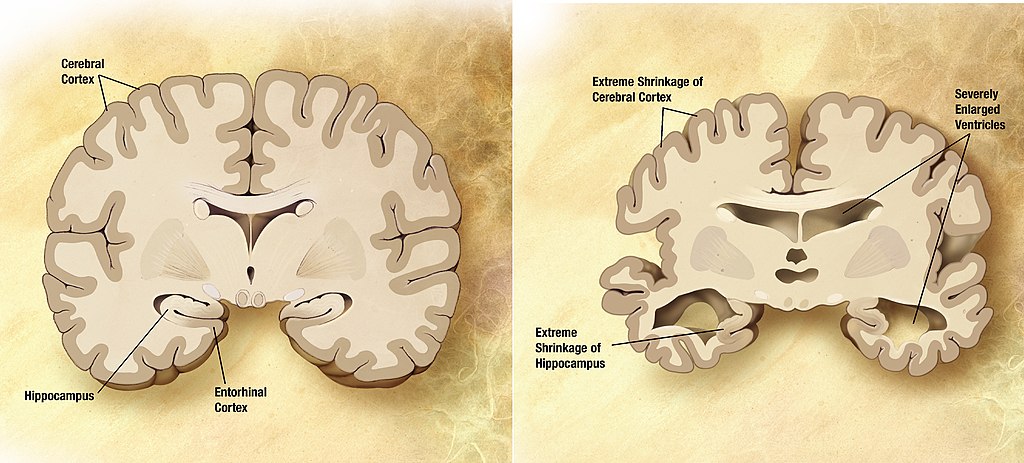
All areas of the brain are affected by AD, but the most notable changes occur in the hippocampus, cerebral cortex, namely the temporal lobe, the parietal lobe, the frontal lobe, and in the cingulate gyrus. There is actual deterioration of brain tissue in these areas, with gyri becoming wider and shallower. The ventricles become larger, leading to an over decrease in brain tissue mass.
There is no cure for AD, and the medications used in treatment of the disease have little effect on disease progression. People with AD live an average of 10 years after initial diagnosis, with steadily declining abilities in cognition, communication, and motor skills.
Although no cure for AD is eminent, there is some promising research that will help scientists better understand the disease process and then develop drugs and interventions that could help slow progress, decrease symptoms, and ultimately, prevent or cure AD. The possible role of viruses (Resource 03) and diabetes (Resource 04) in the development of AD is developing some new insights into the condition.
Check Your Knowledge
After viewing the video and reading the text above, answer the following questions about Alzheimer disease.
9.5 Huntington Disease (HD)
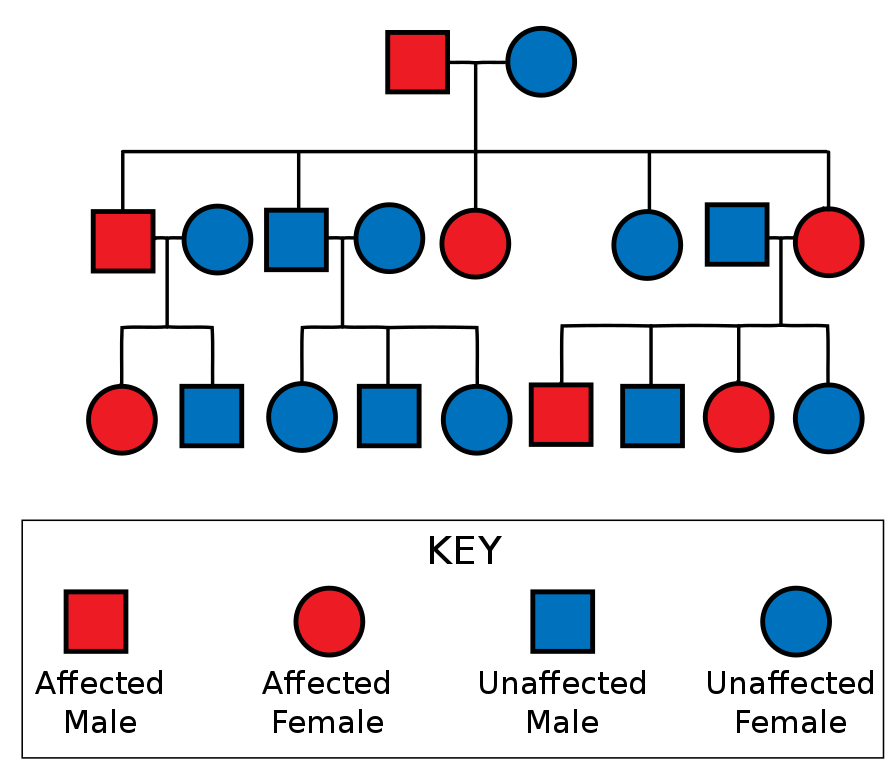
Hunting disease (HD) is a rare neurologic disease with a known genetic trait. It is a dominant gene, passed from parent to child with each child having a 50% chance of expressing the gene and being affected by HD. Of course, there is also a 50% chance of being completely free of the disease. There is no carrier state in a condition that is a dominant trait. The mutation can also occur spontaneously if neither parent has HD. The genetic mutation gets stronger with each successive generation, so offspring develop the disease at younger ages than their parents.
HD causes degeneration of the entire brain, but the first area and most significant area of destruction is the basal ganglia. As brain matter lessens, the lateral ventricles expand, and the brain becomes less dense and decreased in mass.
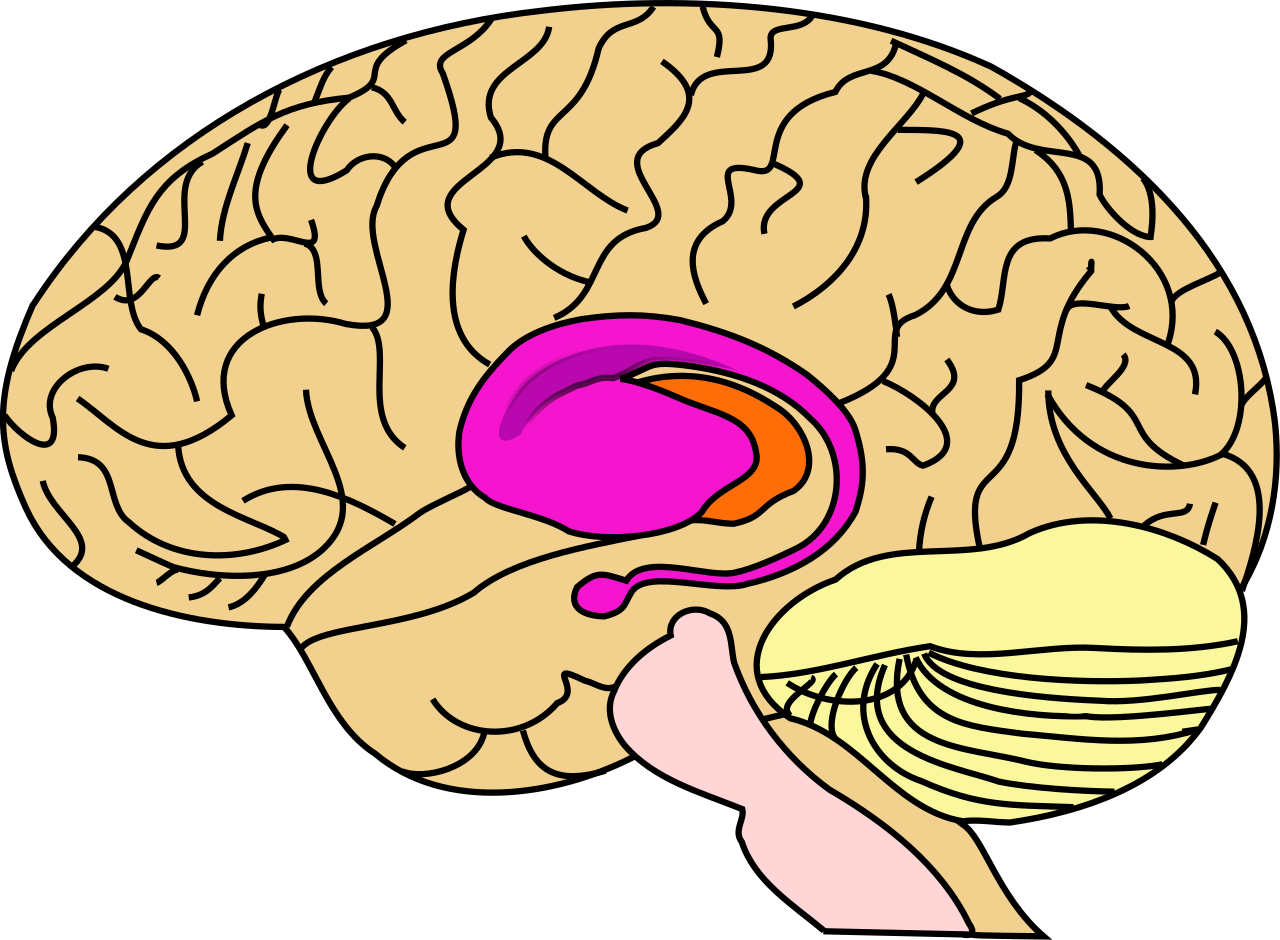
The striatum (in pink) is the major area of the brain to be affected by HD.

Coronal FSPGR through the brain at the level of the caudate nuclei demonstrating marked reduced volume in keeping with the patient’s known diagnosis of Huntington Disease. Image from Radiopaedia.org case here
The basal ganglia are largely responsive for inhibition of movement and behavior, so one of the symptoms of HD is uncontrolled jerking or flailing motions known as chorea. (The disease used to be called Huntington’s Chorea.) Other movement disorders include incoordination, abnormal eye motions, abnormal facial expressions, speaking and swallowing difficulties, and muscular rigidity. Behavioral and mood changes are also typical in the disease. These include irritability, anxiety, apathy, depression, obsessive and compulsive disorders, and rarely, psychoses. Cognitive functions are also affected. Memory, problem solving, planning, organizational skills, and abstract thinking diminish, and dementia is the eventual outcome. Internal organs, including the heart and lungs can also be involved. The diaphragm and other respiratory muscles become involved as the disease progresses.
There is no cure for HD and the average life expectancy from the onset of symptoms is 20 years. The average time of diagnosis is around the age of 40, but with successive generations, the onset can be much earlier, even as early as in infancy. The most common cause of death from HD is pneumonia, usually because of aspiration, infection, and lack of mobility. The second most common cause of death is heart dysfunction. The third most common cause of death is suicide.
There are a few drugs used to treat HD, but none completely control the symptoms or increase the life expectancy. Physical therapy is beneficial for patients with HD. In early stages, fall prevention and general muscular strength and cardiopulmonary conditioning are important aspects of PT. Falls are common in patients with HD, so PTs and PTAs will also be involved in the treatment of musculoskeletal injury in HD. In later stages, breathing techniques, gait training with assistive device, transfer training, and education for caregivers become important. As mobility decreases, prevention of pressure injuries needs to be addressed. Eventually the patient will be dependent for all aspects of daily living.
To see video of some patients with HD, please check out this YouTube video. Warning: It’s kind of difficult to watch. Tough disease.
9.5 – Resource 04 – “Living with Huntington’s Disease” by Attitude is licensed under Fair Use
Test Your Knowledge
Answer each of the following questions regarding Huntington disease.
9.6 Friedreich Ataxia (FA)
The first thing you should probably do to learn about Friedreich ataxia (FA), is watch this video and learn from a kid who has it. He’s very bright and the video is spot-on.
9.6 – Resource 01- “Jake and Friedreich’s Ataxia” by Randall Juip is licensed under Fair Use
FA is a genetic disorder which is recessive in nature. That means both parents carry a gene that causes the disease and the child must get two copies of the gene to express the condition.
FA affects the spinal cord and peripheral nerves. Demyelination of the peripheral nerves and sclerosis and degeneration of the dorsal root ganglion are prominent features of this disorder. Within the spinal cord, the spinocerebellar tracts, lateral corticospinal tracts and posterior columns are affected. The defects in these sensory nerves and their connections with the cerebellum cause the classic symptoms of incoordination, gait disturbances, and slurring of speech. The motor neurons of the spinal cord are not affected in FA.
Friedreich ataxia is diagnosed during childhood or adolescence, between the ages of 5 and 15, when symptoms begin to appear. There is a form of FA, called late-onset FA, which begins in early adulthood, in the 20s or 30s. For most patients, the first sign of FA is frequent tripping and clumsiness. Other symptoms may include muscular weakness, scoliosis, pes cavus, slurred speech, vision and/or hearing loss, diabetes and heart disorders. Deep tendon reflexes, proprioception, vibratory sense, and kinesthetic awareness are diminished or absent. Complete loss of sensation in the arms and legs occurs as the disease progresses. Speaking and swallowing become problematic, especially later in the disease process. Many people with FA develop diabetes as the disease progresses. Cognition and emotional centers of the brain are not affected. There is a general decline in physical abilities, and death usually occurs 15-20 years after the onset of symptoms. Heart dysfunction is the most common cause of death.
There are no drugs to effectively treat FA and there is no known cure. Medications for diabetes and heart dysfunction are helpful in controlling those issues. Many patients undergo spinal surgeries to correct or limit scoliosis. Physical therapy is very helpful in the management of FA. It is important to help patients to maintain strength and endurance for as long as possible. Assistive devices, splints, and braces can help maintain function and mobility. A wheelchair will be a necessity, and a PT or PTA can make recommendations for appropriate wheelchair and seating options.
A good fact sheet on FA is available through NIH.
Friedreich Ataxia Fact Sheet – Click to view
9.6 – Resource 02 – Friedreich Ataxia Fact Sheet – https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Friedreichs-Ataxia-Fact-Sheet
Check Your Knowledge
9.7 Spinal Muscular Atrophy (SMA)
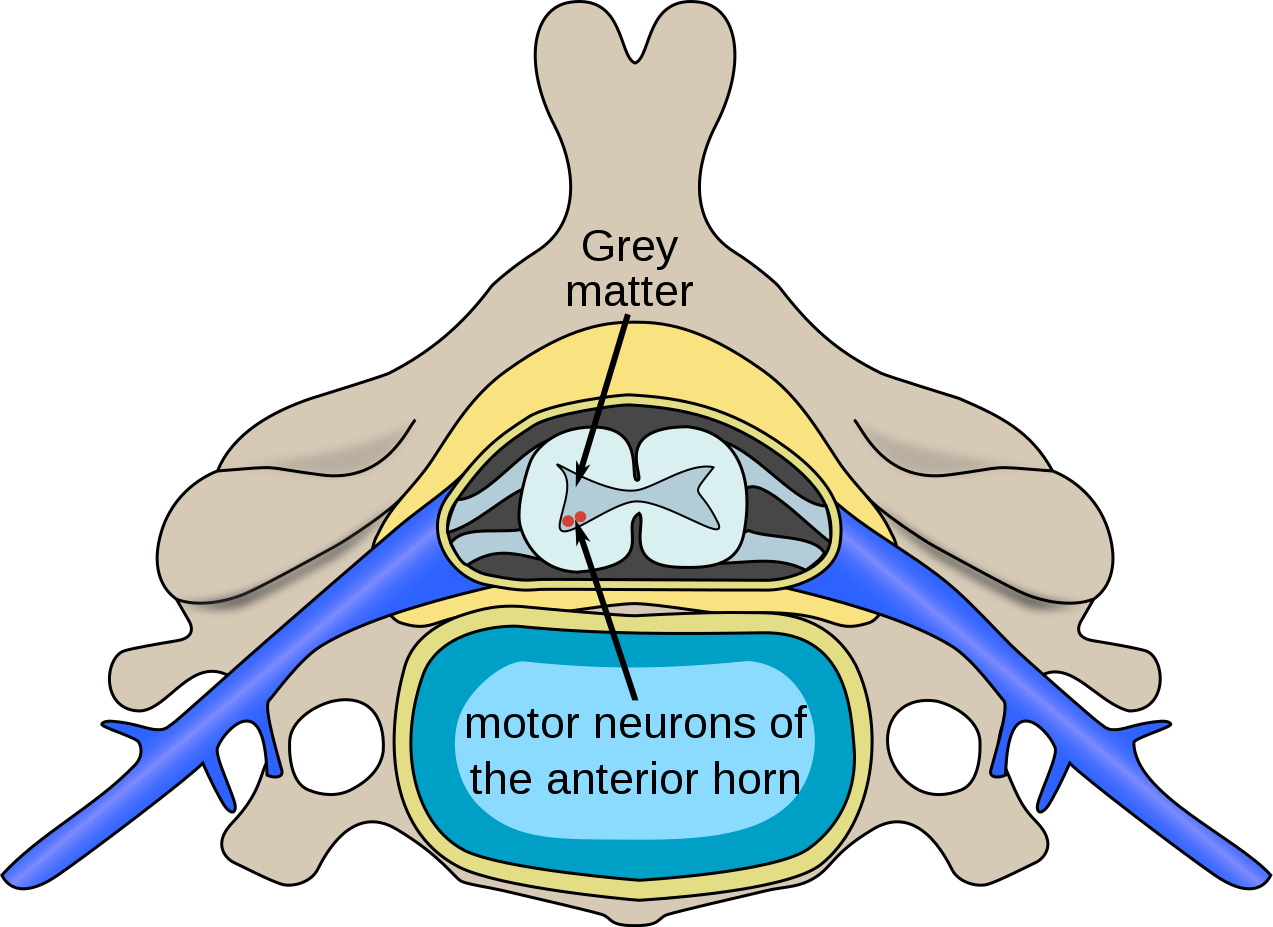
Spinal muscular atrophy (SMA) is an autosomal recessive degenerative genetic disorder that affects the motor neurons in the spinal cord and effects muscular strength in the trunk and periphery. The area that is affected is the anterior horn cells of the spinal cord, which leads to progressive weakness of all skeletal muscles.
There are several types of SMA, which vary greatly in age of onset, progression of symptoms, and life expectancy. The most severe type begins in infancy and the life expectancy can be several weeks to 2 years. Other types are diagnosed in later childhood, and life expectancy can be somewhat decreased or near normal. The adult-onset form of SMA does not decrease life expectancy.
In all forms of SMA, the muscles most affected are the proximal muscles. As the disease progresses more distal musculature becomes involved. Hypotonia and decreased or absent reflexes are noted in SMA. Respiratory involvement is quite problematic in the more aggressive forms of the condition.
There is one major drug available to treat SMA, nusinersen (trade names: Spinraza and Zolgensma). Both appear to slow the progression of the disease, and there is hope they can reverse the genetic damage causing the disease. So far, neither is none to cure SMA and ventilatory assistance toward the end of life is necessary for many patients with SMA. PTs and PTAs can help maintain strength and cardiovascular condition, assist with breathing techniques, provide training for with gait with assistive devices, provide splinting or orthotic devices, and assist patients with general mobility and activities of daily living.
The following video is very helpful in understanding SMA.
https://youtube.com/watch?v=Ax89gbbC-4g
9.7 – Resource 02 – “Spinal muscular atrophy – causes, symptoms, diagnosis, treatment, pathology”, Osmosis is licensed under Fair Use
Check Your Knowledge
After reading and watching the video on SMA, answer the following questions.
9.8 Dystonia
Dystonia is a movement disorder that causes muscles to contract involuntarily. Contractions, or muscle spasms, are often repetitive, often with a rotational component. There are different types of dystonia. Focal dystonia affects only one body part; segmental dystonia affects two or more adjacent parts; and general dystonia affects all body parts. The spasms can range from mild to severe.
The etiology of dystonia is most often unknown, although there are some familial types which have an identified genetic basis. Sometimes dystonia occurs following injury to the brain from head trauma, stroke, drug use, or infection, such as meningitis. The basal ganglia and cerebellum are the parts of the brain most often affected in dystonia.
Dystonia can affect people of all ages, although focal dystonia that begins after age 21 tends to affect the musculature of the head, neck, face, or arm and remain focal or segmental. Sometimes, spasms are associated with a specific activity, such as handwriting. Symptoms are aggravated by stress or fatigue and usually become more noticeable over time.
There is no cure for dystonia, but medications can be helpful in lessening some of the muscle contractions. Some of the medications most often used in treating dystonia are in listed in the box below. Surgery is sometimes used to disable peripheral nerves or stimulate deep areas of the brain. More information about dystonia can be found at the following website.
9.8 – Resource 01 – Dystonia: Causes, Types, Symptoms, and Treatments, WebMD is licensed under © 2005 – 2021 WebMD LLC. All rights reserved.
The video below explains dystonia.
9.8 – Resource 02 – Demystifying Dystonia, Demystifying Medicine is licensed under Fair Use
Medications used in Dystonia
- Anticholinergics
- Diphenhydramine
- Benzatro
- Atropine
- Baclofen
- Botox
- Muscle relaxants
- Parkinson’s medications
Here is a nice Ted Talk on dystonia. It’s a good personal story.
9.8 – Resource 03 – Dystonia. Rewiring the brain through movement and dance | Federico Bitti | TEDxNapoli, TEDx Talks is licensed under Fair Use
Check Your Knowledge of Dystonia
After reading and watching the video, answer the questions about dystonia.
Quick Check: Degenerative Neurologic Conditions
For each of the items below, match the condition with major areas of involvement within the neurologic system.
Degenerative Neurological Disorders Resources:
Section 9.1
Resource 01 – “Motor neurons | Muscular-skeletal system physiology | NCLEX-RN | Khan Academy”
Resource 02 – “Upper motor neurons | Organ Systems | MCAT | Khan Academy”
Resource 03 – “ALS – Amyotrophic lateral sclerosis | Miscellaneous | Heatlh & Medicine | Khan Academy”, Khan Academy is licensed under Fair Use
Section 9.2
Resource 01 – “ALS – Amyotrophic lateral sclerosis |What are the symptoms of Parkinson’s Disease? – Ask the Experts” by ButlerHospital is licensed under Fair Use
Resource 02 –Two sketches (one from the front and one from the right side) of a man, with an expressionless face. He is stooped forward and is presumably having difficulty walking. – “File:Paralysis agitans (1907, after St. Leger).png” by William Richard Gowers (1845–1915) after St. Leger (unknown dates) is in the Public Domain
Resource 03 – Substantia nigra – “File:Substantia nigra.gif” by FrozenMan is licensed under CC BY-SA 4.0
Resource 04 – “What is Parkinson’s disease? | Nervous system diseases | NCLEX-RN | Khan Academy” by khanacademymedicine is licensed under Fair Use
Resource 05 – “Putting it all together – Pathophysiology of Parkinson’s disease | NCLEX-RN | Khan Academy” by khanacademymedicine is licensed under Fair Use
Section 9.3
Resource 01 – “What is multiple sclerosis? | Nervous system diseases | NCLEX-RN | Khan Academy” by khanacademymedicine is licensed under Fair Use
Resource 02 – “Multiple sclerosis signs and symptoms | Nervous system diseases | NCLEX-RN | Khan Academy” by khanacademymedicine is licensed under Fair Use
Section 9.4
Resource 01 – NIH National Institute on Aging: How Alzheimer’s Changes the Brain
Resource 02 – Diagram of a Normal Brain and a Brain with Alzheimer’s Disease – “File:Alzheimer’s disease brain comparison.jpg” by Garrondo is in the Public Domain
Resource 03 – Abbott, Alison. “Are infections seeding some cases of Alzheimer’s disease?” Nature 587, 22-25 (2020)
Resource 04 – “Keeping Your Blood Sugar In Check Could Lower Your Alzheimer’s Risk”
Section 9.5
Resource 01 – Huntington’s disease is inherited in autosomal dominant fashion. – “File:Autosomal Dominant Pedigree Chart2.svg” by Jerome Walker is licensed under CC BY-SA 3.0
Resource 02 – Area affected by Huntington’s disease – “File:BrainCaudatePutamen.svg” by John Henkel and Leevanjackson is in the Public Domain
Resource 03 – Cross section of brain with Huntington’s disease – “File:Huntington.jpg” by Frank Gaillard is licensed under CC BY-SA 3.0
Resource 04 – “Living with Huntington’s Disease” by Attitude is licensed under Fair Use
Section 9.6
Resource 01- “Jake and Friedreich’s Ataxia” by Randall Juip is licensed under Fair Use
Resource 02 – Friedreich Ataxia Fact Sheet – NIH National Institute of Neurological Disorders and Stroke
Section 9.7
Resource 01 – Polio Spinal Diagram – “File:Polio spinal diagram-en.svg” by Fred the Oyster is licensed under CC BY-SA 4.0
Resource 02 – “Spinal muscular atrophy – causes, symptoms, diagnosis, treatment, pathology”, Osmosis is licensed under Fair Use
Section 9.8
Resource 01 – Dystonia: Causes, Types, Symptoms, and Treatments, WebMD is licensed under © 2005 – 2021 WebMD LLC. All rights reserved.
Resource 02 – Demystifying Dystonia, Demystifying Medicine is licensed under Fair Use
Resource 03 – Dystonia. Rewiring the brain through movement and dance | Federico Bitti | TEDxNapoli, TEDx Talks is licensed under Fair Use

