Chapter 2: Injury, Inflammation, and Healing
rlb18
Learning Objectives
After completing this chapter, the learner should be able to:
- Discuss the mechanisms of cell injury.
- Discuss the processes involved in reversible and irreversible cell injury.
- Discuss the pathophysiology, signs and symptoms, stages, and complications of acute and chronic inflammation.
- Discuss the types of healing, factors affecting healing, and the complications of healing.
Chapter Contents
2.0 Injury, Inflammation, and Healing
To maintain a healthy body in an environment that exposes us to many potentially harmful situations and substances every day, we must have mechanisms in place to provide protection and defenses. Cells can sustain injury resulting from of any of the following mechanisms.
Mechanisms of Cell Injury
| Mechanisms of Cell Injury | Examples |
|---|---|
| DEFICIT | |
| Oxygen | Hypoxia leading to ischemia; for example cardiac muscle following a heart attack |
| Nutrition | Could be lack of ingested nutrients or deficit in transporting or absorbing nutrients |
| Hydration | Lack of water from lack of ingestion, transportation or absorption |
| TOXINS | |
| Endogenous | Metabolic errors or malformations that create toxic environments |
| Exogenous | Drugs, chemicals, inhalants |
| INFECTION | |
| Bacterial | Staph or strep infections, for example |
| Viral | Flu or herpes, for example |
| Fungal or other | Yeast infections (fungal), ringworm (fungal), tapeworms (protozoan |
| MECHANICAL | |
| Direct trauma or pressure |
Cuts, bumps, bruises, concussions, damage caused by squeezing or swelling |
| Thermal | Heat (burns); cold (frostbite) |
2.1 Reversible and Irreversible Cellular Damage
Cell damage can be divided into 2 main categories: reversible and irreversible. As the names would suggest, reversible cell damage results in the cell recovering from the injury, while irreversible damage causes cell death.
2.1.1 Reversible:
If the stress to the cell is of short duration or low in toxicity, the damage caused by any of the mechanisms of injury can be reversible. In reversible damage, the cell and some of its organelles can swell and perhaps function can be altered, but the nucleus remains unchanged, and the cell is able to recover and return to its normal homeostasis and function as it should.
2.1.2 Irreversible:
Sometimes the cellular stress is of great magnitude or occurs over an extended period, leading to irreversible damage. In this case, the functioning of the organelles within the cell, and the nucleus itself, are damaged and cease functioning. The cell membrane is often destroyed, and the cellular contents are dispersed, often causing damage to nearby cells. This cell death is called necrosis. The damaged cellular contents form substances called exudates, that can accumulate in or around organs. The types of necrosis are listed below.
2.1.3 Coagulative necrosis:
The nuclei of the cells die, but the cell membranes remain intact. The cells coalesce. This type of necrosis occurs in ischemia in internal organs, such as the heart, kidneys, or liver. Dry gangrene in the limbs is also classified as coagulative, although some sources list gangrene as a separate type of necrosis.
2.1.4 Caseous (cheesy)necrosis:
The cell membrane is destroyed, and contents of the cell become thick, creating a cheesy formation that persists in a walled-off fashion, forming a granuloma. This type of necrosis is most often associated with tuberculosis or another lung infection.
2.1.5 Liquefactive necrosis:
Pockets of liquid remain after the cell and its contents are destroyed in liquefactive necrosis, which is most common in the brain. Wet gangrene (gangrene due to active infection) in the extremities is also classified as liquefactive, although some sources list gangrene as a separate type of necrosis.
2.1.6 Fatty necrosis:
Fatty necrosis occurs in the pancreas or abdominal area in response to acute pancreatitis or abdominal trauma. White, chalky deposits of calcium, called soaps, are deposited in the necrotic area.
2.1.7 Fibrinoid necrosis:
Blood vessels experience fibrinoid necrosis when injured. As cells die and disintegrate, plasma proteins and fibrin accumulate in the cell walls, causing stiffness in the vessel walls.
(cite: Goodman, Catherine, Pathophysiology: Implications for the Physical Therapist, Philadelphia, Elsevier, 2003.)
Long Description
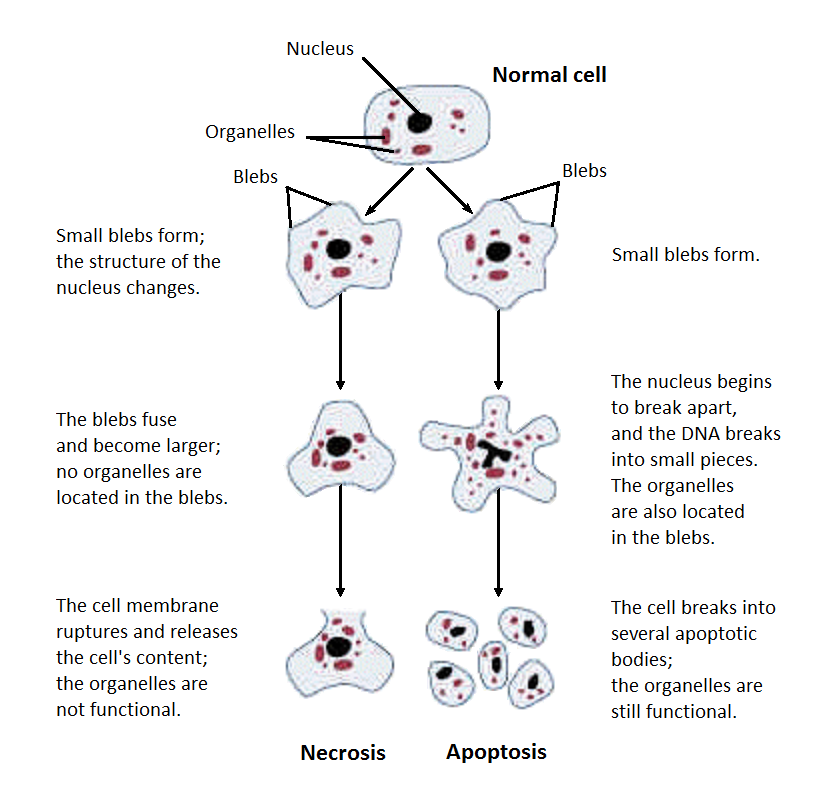
Title: Necrosis and Apoptosis
A normal cell with nucleus and organelles shows 2 arrows pointing to 2 different versions of the cell.
- On the left:
- Small blebs form; the structure of the nucleus changes.
- The blebs fuse and become larger, no organelles are located in the blebs.
- The cell membrane ruptures and releases the cell’s content; the organelles are not functional.
- On the right:
- Small blebs form
- The nucleus begins to break apart, and the DNA breaks into small pieces. The organelles are also located in the blebs.
- The cell breaks into several apoptotic bodies; the organelles are still functional.
2.1.8 Apoptosis
Apoptosis is a particular type of cell death that does not stimulate the inflammatory response or result in exudate formation or other harmful processes. Unlike necrosis, which is caused by some sort of insult to the cell, apoptosis is a normal process of programmed cell death. Through apoptosis, an organized disassembly of old or less functional cells occurs, and the cell breaks apart into small units. New cells replace the cells that have disintegrated, maintaining homeostasis. Optimal number of cells and optimal function of the organ are preserved.
For a short video, explaining the differences between necrosis and apoptosis, view the following:
2.1 -Resource 02 – “Cell Death Explained: Necrosis vs. Apoptosis” by Michael Post is licensed under Fair Use
2.2 Cellular Adaptation
Sometimes, changes to the environment of the cells or DNA or other changes within the cells require the group of cells to adapt. Different types of cellular adaptation are listed below.
2.2.1 Types of “-plasia”
- Anaplasia (structural differentiation loss within a cell or group of cells)
- Aplasia (organ or part of organ missing)
- Hypoplasia (congenital below-average number of cells, especially when inadequate)
- Hyperplasia (proliferation of cells)
- Neoplasia (abnormal proliferation)
- Dysplasia (change in cell or tissue phenotype)
- Metaplasia (conversion in cell type)
- Prosoplasia (development of new cell function)
- Desmoplasia (connective tissue growth)
2.2.2 Types of “-trophy”
- Atrophy (reduced functionality of an organ, with decrease in the number or volume of cells)
- Hypertrophy (increase in the volume of cells)
- Hypotrophy (decrease in the volume of cells)
- Abiotrophy (loss in vitality of organ or tissue)
- Dystrophy (any degenerative disorder resulting from improper or faulty nutrition)
Long Description
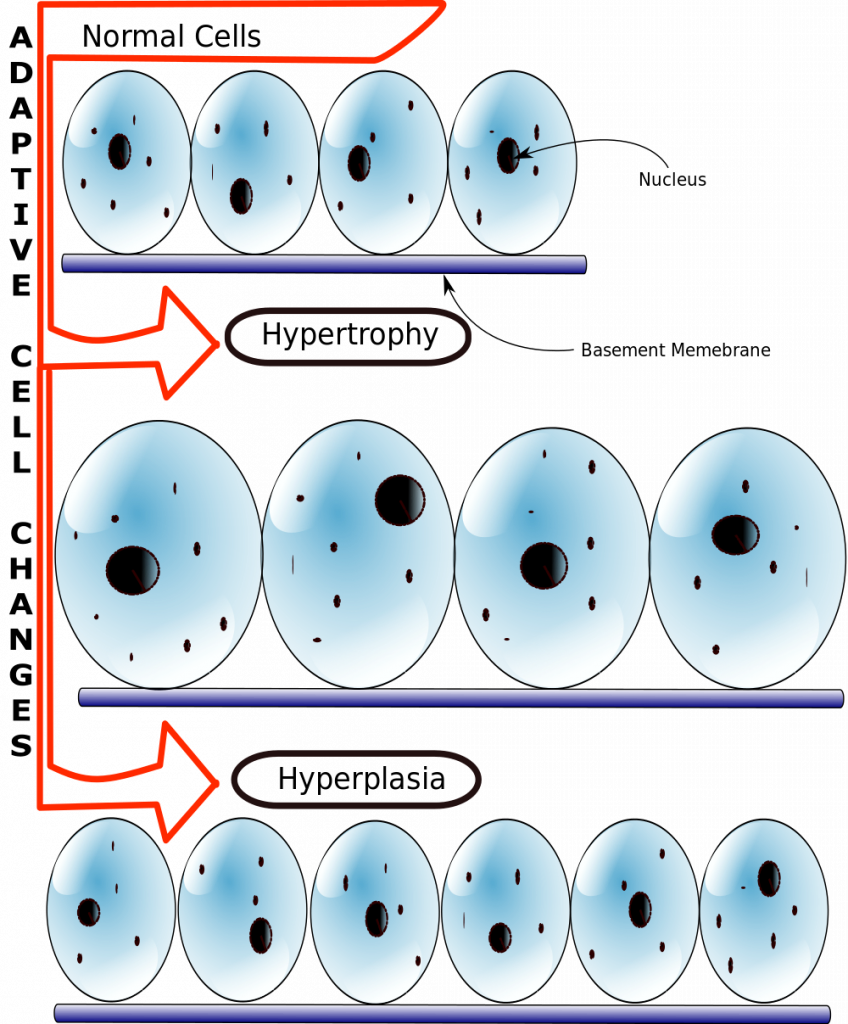
Title: Adaptive Cell Changes
Illustration of adaptive cell changes show 3 levels of cells. The top level are normal cells sitting on a basement membrane. One cell’s nucleus in labelled. The second level of cells are labelled hypertrophy; they also sit on a membrane and are larger than the top layer. The bottom layer are hyperplasia; they are smaller than the second level cells and sit on a membrane.
Link to source – Hypertrophy
In some cases, cellular adaptation can be helpful. For example, with exercise, muscle cells get larger through hypertrophy, which is generally good. Another example is the development of a callous in response to excessive friction on the skin; the callous would be the result of hyperplasia. But hypertrophy or hyperplasia in the cardiac muscle or blood vessel walls causes adverse consequences, including hypertension and heart failure.
The adaptations of cells can be benign or can have devastating consequences. Many cancerous conditions are associated with chronic irritation and inflammation. One example is the change in the epithelial cells lining the bronchi of people who smoke. The normal columnar epithelium can be replaced by squamous cells, which alters the function of the cells. This is a metaplastic change and a pre-cancerous condition.
2.2.5.Stages of wound healing
Watch the video at https://www.youtube.com/watch?v=Q3cVCiraAgw to learn about the 4 stages of wound healing and the local and systemic factors that influence wound healing.
https://www.youtube.com/watch?v=Q3cVCiraAgw
Please answer the following questions regarding the video.
2.3 The Inflammatory Response
Our bodies possess several different barriers and mechanisms to keep our cells from sustaining injury. Skin and other epithelial tissues provide a first layer of defense for many pathogens or other insults on the underlying cells. Fluids, such as mucus, sweat, and tears also help wash away some pathogens and contain cells that can kill some pathogens before they enter the body. Once an injurious agent does enter and cause damage to cells, the initial response is inflammation, which includes several different processes. Inflammation is a non-specific response, that is, the process is the same no matter what the mechanism of injury. A different response, the immune response, is pathogen-specific and will be discussed in a separate chapter. Please watch the following videos and answer the questions regarding the inflammatory process.
2.3 – Resource 01 – “The Inflammatory Response” by , PhysioPathoPharmaco is licensed under Fair Use
Link to first inflammation video
2.3 – Resource 02: “Inflammatory response | Human anatomy and physiology | Health & Medicine | Khan Academy” by , Khan Academy is licensed under Fair Use
Answer the following questions:
Signs and Symptoms of Inflammation
| Sign/Symptom | Cause |
|---|---|
| Edema | Dilation and endothelial retraction |
| Heat | Increased blood flow to the area |
| Redness | increased erythrocytes in the area due to increased blood flow |
| Pain | Chemical and mechanical (pressure) stimulation of nerve endings |
| Loss of fuction | Cells die, swelling increases pressure, pain |
2.4 Acute Inflammation vs Chronic Inflammation
Inflammation that occurs in a short time period is considered acute. The signs and symptoms are often quite pronounced, and healing occurs quickly, often with little or no residual effects. Physical therapy interventions for acute inflammation often include protection, rest, ice, compression, and elevation (PRICE). Most other physical therapy interventions, including most exercises, are contraindicated in the presence of acute inflammation. As inflammation resolves, the inflammation may enter the subacute phase. Many physical therapy modalities can be initiated during the subacute phase.
In chronic inflammation, the duration of the inflammation is longer, but the signs and symptoms of inflammation are usually much less noticeable. Chronic inflammation can be caused by unresolved acute inflammation or can develop insidiously with no acute phase. Chronic inflammation is more likely than acute inflammation to cause scarring and impaired function. Physical therapy interventions are less likely to be contraindicated in chronic than in acute inflammation. Read the following article on chronic inflammation and chronic inflammatory disease, then answer the following questions.
article on chronic inflammation and chronic inflammatory disease
It is possible that both acute and chronic inflammation exist simultaneously. People with chronic conditions, such as rheumatoid arthritis often has acute exacerbations, or flares. Although the PTA might be treating the chronic condition, they should be aware of signs and symptoms of an acute flare, so they do not inadvertently perform an intervention that is indicated for the chronic condition but contraindicated for the acute condition.
2.5 Inflammation and Complications
In general, a body that is in good physical condition will recover from most acute inflammatory conditions, unless they are of significant potency or virulence. Poor nutritional status, lower socioeconomic status, and comorbidities of any kind can complicate the picture, prolonging inflammation, increasing the chances of acute inflammation becoming a chronic condition. Genetics are also a factor, especially inherited predispositions to conditions such as diabetes mellitus, rheumatoid arthritis, or other autoimmune disorders. Smoking and alcohol use have also been linked with delayed healing of wounds. Other factors, such as diet, exercise, age, sleep, and stress can also affect the likelihood of developing and recovering from inflammation.
2.6 Healing
For a short video explaining the phases of healing, see below:
2.6 – Resource 01 – “Wound Healing” by crvomy is licensed under Fair Use
Answer the following questions:
2.6 – Resource 02 – Wound Healing phases
Long Description
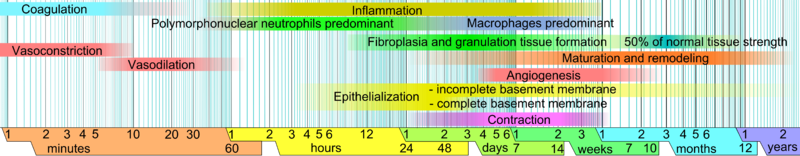
Title: Wound Healing Phases: Logarithmic Timeline
From left to right the timeline starts with 1 to 60 minutes, then 1 hour to 48 hours, then 1 day to 14 days, then 1 to 10 weeks, then 1 to 12 months, then finally 1 to 2 years.
Seven layers are above the timeline
- Layer 1
- Coagulation: 0 to 10 minutes
- Inflammation: 1 hour to 1 month
- Vasoconstriction (separate layer): 1 to 10 hours
- Vasodilation (separate layer): 5 to 60 minutes
- Layer 2
- Polymorphonuclear neutrophils predominant: 30 minutes to 2 days
- Macrophages predominant: 2 days to 1 month
- Layer 3
- Fibroplasia and granulation tissue formation: 12 hours to 1 month
- 50% of normal tissue strength: 2 to 12 months
- Layer 4
- Maturation and remodeling: 1 day to 2 years
- Layer 5
- Angiogenesis: 3 days to 3 months
- Layer 6
- Epithelialization
- Incomplete basement membrane: 5 hours to 5 months
- Complete basement membrane: 5 hours to 3 days
- Layer 7
- Contraction: 1 day to 1 month
2.6.1 Healing by First Intention or Second Intention
Watch the following video regarding healing by first or second intention, then answer the questions.
2.6 – Resource 03: “Wounds and healing 6, Primary and secondary healing” by Dr. John Campbell is licensed under Fair Use
For a short review of wound healing and information about the role physical therapy can play in wound care, see the Physiopedia page on wounds.
2.6.2 Regeneration and Repair
If lost or damaged cells are replaced by the same type of cells in the healing process, the process is called, regeneration. If different types of cells replace the lost cells, the process is called repair. Epithelial cells in the skin regenerate quickly and easily, so a paper cut, for example, will heal through regeneration. Larger wounds, such as burns, where much tissue is lost, must heal by repair, where scar tissue replaces normal epithelial cells. It is not uncommon to have wounds heal through a combination of both regeneration and repair. Regeneration is more favorable than repair, both for cosmesis, as in external wounds on the skin, but more importantly for function. Scar tissue does not function as other types of tissue. Areas of scarring on the skin will often lose the ability to sweat or grow hair. Internally, cardiac tissue damaged in a heart attack, will lose its contractile ability and lung tissue damaged by smoke may lose its ability to expand during inhalation.
The Injury, Inflammation, and Healing Resources
Section 2.1
Resource 01 – “File:Structural changes of cells undergoing necrosis or apoptosis.png” by National institute on alcohol abuse and alcoholism (NIAAA) is in the Public Domain
Resource 02 – “Cell Death Explained: Necrosis vs. Apoptosis” by Michael Post is licensed under Fair Use
Section 2.2
Resource 01 – Differences between hypertrophy and hyperplasia – “File:Hyperplasia vs Hypertrophy.svg” by Schwarze Melancholie is licensed under CC BY-SA 3.0
Section 2.3
Resource 01 – “The Inflammatory Response” by , PhysioPathoPharmaco is licensed under Fair Use
Resource 02: “Inflammatory response | Human anatomy and physiology | Health & Medicine | Khan Academy” by , Khan Academy is licensed under Fair Use
Section 2.6
Resource 01 – “Wound Healing” by crvomy is licensed under Fair Use
Resource 02 -Would Healing Phases – “File:Logarithmic time scale – milliseconds to years.svg” by Mikael Häggström is in the Public Domain
Resource 03: “Wounds and healing 6, Primary and secondary healing” by Dr. John Campbell is licensed under Fair Use

