Chapter 1: Introduction to Pathophysiology
rlb18
Learning Objectives
After completing this chapter, the learner should be able to:
- Define basic terminology used in the discussion of pathophysiology.
- Discuss cultural, ethnic, geographical, and age-related differences regarding health and illness.
- Discuss the ICF Disablement Model: define terms associated with it and discuss its relevance to physical therapy.
Chapter Contents
Physical therapist assistants (PTAs) are expected to possess a basic understanding of diseases and conditions, whether they are the focus of physical therapy intervention or comorbidities that could affect interventions and recovery. This text is intended to introduce PTA students to Pathophysiology and provide them with knowledge necessary for addressing patients and health professionals in clinical settings. Students enrolled in a course in Pathophysiology should bring to the course a solid foundation of Anatomy and Physiology, as this text is intended to build upon knowledge of normal body structures and functions. An understanding of how the body works when a person is well is essential to understanding how health and homeostasis can be disrupted by disease or injury.
1.1 Basic Terminology
A common language is a logical place to begin the discussion of pathophysiology. Listed below are several terms and definitions that will be used throughout the text and in most discussions of disease and the study of disease.
Condition – state of being. In medical terms, anything that disrupts the body’s normal homeostasis can be considered a condition. Bone fractures, visual deficits, infectious diseases, and chronic illnesses are all termed “conditions.”
Disease – a medical condition, usually with negative effects, that is associated with a specific list of signs and symptoms. Often, “disease” is used to describe a communicable, or infectious, condition. Parkinson’s disease is an example of a non-infectious condition that affects the nervous system.
Acute – refers to a condition or disease that has a sudden onset and short course in the body. Strep throat is usually an acute condition.
Chronic – lasting a long time, maybe a lifetime. Diabetes mellitis and heart failure are chronic conditions.
Latent stage – a stage of the infectious disease process during which the pathogenic agent is in the body, but in an inactive form. The varicella virus that causes chicken pox can remain in a latent stage in the body and become reactivated years later as shingles.
Congenital – present since birth, but not necessarily genetic in nature. A baby exposed to syphilis during the birth process will be diagnosed with congenital syphilis. This condition is not genetic, but it is congenital.
Genetic – caused by genetic mutations or other problems in the transfer and development of genetic material. Trisomy 21 is a genetic condition caused by an abnormal number of genes. This genetic condition causes the most common form of Down syndrome
Infectious – refers to a communicable disease, caused by a pathogen, such as a bacterium or virus. HIV is an infectious disease.
Idiopathic – refers to no known cause. Most adolescents and pre-adolescents who develop scoliosis are diagnosed with idiopathic scoliosis.
Iatrogenic – refers to an illness or condition caused by the medical profession. Sometimes, patients who are prescribed high doses of steroids develop Cushing’s syndrome. This is an example of an iatrogenic condition.
Nosocomial – refers to an illness or condition acquired during a hospital, or inpatient, stay. Urinary tract infections acquired during hospitalization are common nosocomial conditions.
Precipitation factor – trigger; a factor that causes an exacerbation of symptoms or flare-up of disease or condition. Pollen is a common precipitating factor in seasonal allergy.
Predisposing factor– risk factor; a trait, habit or environmental condition that causes one to be more likely to develop a disease or condition. Obesity is a predisposing factor for heart disease.
Insidious – gradual; a gradual onset of a disease or condition; the patient often cannot identify the date of onset. Cataracts in the eyes often usually have an insidious onset.
Malaise – general feeling of discomfort, pain, lack of energy, often associated with the initial onset of illness. A person often goes through a period of malaise prior to being diagnosed with a specific condition, such as measles or mumps.
Signs – objective indicators of disease that are obvious to someone other than the subject. A bulls-eye rash can be a sign of Lyme disease.
Symptoms – subjective feelings. A patient might complain of shortness of breath, which could be a symptom of heart failure.
Syndrome – a collection of signs, symptoms or conditions that often occur together, creating a named condition. Metabolic syndrome includes increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels.
Sequelae – describe the potential unwanted outcomes of the primary condition. One possible sequela of bacterial encephalitis is hearing loss.
Morbidity rate– indicates the functional impairment that certain diseases inflict on the population. Low back pain has a very high morbidity rate in the United States.
Mortality rate– number of deaths resulting from a disease or condition. The morbidity rate for amyotrophic lateral sclerosis (ALS) is much higher than for many other neurological conditions.
Epidemiology – the science of tracking the pattern or occurrence of a disease
Epidemic – attacking many people in a region at one time. We try to avoid a flu epidemic by encouraging vaccination.
Pandemic – high numbers of cases in several regions or perhaps worldwide. Bubonic plague, or the Black Death, killed high numbers of people in Europe in the 14th century. AIDs reached pandemic status in the 1980s and 1990s.
Endemic – ever-present in the community. Rhinovirus (causes the common cold) is endemic world-wide.
Incidence – refers to the occurrence of new cases of disease or injury in a population over a specified period of time.
Incidence proportion is the proportion of an initially disease-free population that develops disease, becomes injured, or dies during a specified (usually limited) period of time. Synonyms include attack rate, risk, probability of getting disease, and cumulative incidence. Incidence proportion is a proportion because the persons in the numerator, those who develop disease, are all included in the denominator (the entire population).
Method for calculating incidence proportion (risk)
Number of new cases of disease or injury during
________specified period_______ x10n
Size of population at start of period
Example: Calculating Incidence Proportion
In the study of diabetics, 100 of the 189 diabetic men died during the 13-year follow-up period. Calculate the risk of death for these men.
Numerator = 100 deaths among the diabetic men
Denominator = 189 diabetic men
10n = 102 = 100
Risk = (100 ⁄ 189) × 100 = 52.9%
Incidence proportion is a measure of the risk of disease or the probability of developing the disease during the specified period. As a measure of incidence, it includes only new cases of disease in the numerator. The denominator is the number of persons in the population at the start of the observation period. Because all of the persons with new cases of disease (numerator) are also represented in the denominator, a risk is also a proportion.
Incidence rate or person-time rate is a measure of incidence that incorporates time directly into the denominator. A person-time rate is generally calculated from a long-term cohort follow-up study, wherein enrollees are followed over time and the occurrence of new cases of disease is documented. Typically, each person is observed from an established starting time until one of four “end points” is reached: onset of disease, death, migration out of the study (“lost to follow-up”), or the end of the study. Similar to the incidence proportion, the numerator of the incidence rate is the number of new cases identified during the period of observation. However, the denominator differs. The denominator is the sum of the time each person was observed, totaled for all persons. This denominator represents the total time the population was at risk of and being watched for disease. Thus, the incidence rate is the ratio of the number of cases to the total time the population is at risk of disease.
Prevalence – the proportion of persons in a population who have a particular disease or attribute at a specified point in time or over a specified period of time. Prevalence differs from incidence in that prevalence includes all cases, both new and preexisting, in the population at the specified time, whereas incidence is limited to new cases only.
Point prevalence refers to the prevalence measured at a particular point in time. It is the proportion of persons with a particular disease or attribute on a particular date.
Period prevalence refers to prevalence measured over an interval of time. It is the proportion of persons with a particular disease or attribute at any time during the interval.
Method for calculating prevalence of disease
All new and pre-existing cases
___during a given time period____ × 10 n
Population during the same time period
EXAMPLE: Calculating Prevalence
In a survey of 1,150 women who gave birth in Maine in 2000, a total of 468 reported taking a multivitamin at least 4 times a week during the month before becoming pregnant.(7) Calculate the prevalence of frequent multivitamin use in this group.
Numerator = 468 multivitamin users
Denominator = 1,150 women
Prevalence = (468 ⁄ 1,150) × 100 = 0.407 × 100 = 40.7%
Exercises
Exercise 1
NEW SYNDROME DISCOVERED
The Center for Disease Control has just announced the discovery of a new syndrome affecting many college and university students. The cause of the syndrome is at this time unknown, but it is believed that the causal agent must exist on college and university campuses. Cases have been reported in every state in the nation. On the Penn State Mont Alto Campus alone (total number of students: 1000), 5 new cases were reported on August 28, which makes a total of 15 reported cases since the start of the fall semester on August 26.
The syndrome affects both males and females and is most common in adults over the age of 18, although some less serious cases have been reported in younger adolescents. The syndrome is usually marked by insidious onset of a mild feeling of disinterest which gradually progresses into lethargy toward learning. This can then lead to poor classroom attendance and poor or failing grades. Periods of spontaneous remission have been reported, and are usually associated with school breaks, although the syndrome is often reactivated within several weeks of starting a new semester. If no intervention is implemented, the condition usually becomes chronic and persists throughout life.
The condition has been called Student Apathy Syndrome (SAS). The signs and symptoms of SAS are mild at first, but as the syndrome progresses, they can be easily recognized. Many organs can be affected in SAS as described below:
Vision: eyes may close for long periods during times of study and classroom activities. Vacant stare sometimes apparent.
Hearing: periods of selective deafness may be apparent, especially in instances when assignments are given or test dates announced.
Speech: temporary muteness may accompany visual and hearing disorders when the patient is in a classroom setting.
Sensory: the patient may experience a feeling of muscular weakness or general fatigue although no actual loss of muscle strength has been demonstrated clinically.
Gait: may be slow, often with a kyphotic posture, especially noted in patients who are often late for class.
Appetite: usually not affected, but if affected, usually increased rather than decreased.
The following activities have been associated with severe cases of SAS when undertaken in excess but may not be detrimental if undertaken in moderation: binge TV watching, computer or phone games, social media, socializing with peers, sporting and other recreational activities. Therapeutic intervention is very important, and the earlier it is implemented, the better the prognosis. The patient should perform daily active learning exercises, including reading, note taking, rereading and outlining notes, actively participating in classroom discussions and activities, and enthusiastically completing all assignments in a timely manner. Additional therapeutic interventions include: adequate sleep, exercising daily, and eating a healthy diet, with lots of vegetables. With therapeutic intervention and patient commitment to learning exercises, a complete recovery can be expected.
- 1) What was the prevalence rate of SAS at PSMA on Aug 26? On Aug 28?
- 2) What was the incidence proportion of SAS at PSMA during the period of Aug. 26- 28?
- 3) Describe the etiology of SAS.
- 4) Describe its pathogenesis and possible outcomes.
- 5) List some interventions that are helpful in preventing or curing the condition.
- 6) Name a place where SAS would be considered endemic.
- 7) Where would you NOT expect to see SAS?
- 8) What are YOU doing to ensure you are not a victim of SAS?
1.2 Factors Affecting Health
There are many reasons why people experience differing levels of health. The Office of Disease Prevention and Health Promotion has identified 5 Social Determinants of Health that should be targeted for improvements in the health of people in the United States. The video below, narrated by Admiral Rachel Levine, US Assistant Secretary for Health, presents the 5 Social Determinants of Health as identified by the Health People 2030 initiative. Personal health cannot be adequately discussed without considering public health and the determinants presented in the video. When the discussion is about a particular disease or condition, the terms “risk factors” or “predisposing factors” are often used. Some of the factors affecting our health and likelihood of developing certain conditions are within our control, other less so. Some are individual, such as genetics and ethnicity, and personal choices; others are created by social structures, environmental issues, and laws and regulations. View the video, then answer the questions following the video.
Exercises
EXERCISE 2
Consider the Social Determinants of Health and describe how your own health is affected by where you live, educational opportunities, access to health care, and your own support network. Then think about how different these social determinants are for some other groups. Consider migrant workers that can be seen in the fields next to the Mont Alto campus. Consider the differences between wealthy and powerful people who got COVID (maybe the President of the US) and others (maybe an elderly individual living alone in substandard housing in New York City, or someone without a home at all. You should be able to identify advantages and disadvantages associated with social determinants for yourself and for others.
Other factors that affect health and well-being are either not in our control or much more difficult to control. Some of these include age, ethnicity, cultural beliefs and practices, geographical location, and socioeconomic status.
1.2.1 Age
As we age, our bodies change, which affects our predisposition to some conditions. Infants and young children have underdeveloped immune systems, so they are predisposed to infections like colds and flu, conjunctivitis and impetigo. Advanced age is also associated with a less-robust immune system, so the elderly are more likely than young adults to have problems with the flu and respiratory conditions that can lead to pneumonia. The musculoskeletal system becomes more brittle and bones lose density as people age, so fractures are more common in older people. they are also slower to heal, as blood flow is slower growth factors are less abundant in people of advanced age.
Some conditions are associated with different portions of the human life span. For example, children are most likely to get certain forms of leukemia, acute lymphoblastic leukemia (ALL) or acute myeloid leukemia (AML), while elderly people have a much higher predisposition to different forms, chronic myeloid leukemia (CML) and chronic lymphocytic leukemia (CLL).
Exercises
EXERCISE 3
Look over the information on aging presented by NIH.
Pay special attention to the section on Exercise and Physical Activity.
- List the four types of exercise people should engage in as they age.
- List one or two physical therapy exercise interventions that could help with each.
1.2.2 Sex
Some conditions have a strong association with sex and hormones associated with sex. The connection is not difficult to see in some conditions, such as breast cancer, which is much more common in women than in men. Other disorders seem to have a connection with sex, but in some cases, the connection is not well understood. Many autoimmune diseases, such as multiple sclerosis, lupus, and Sjogren’s disease affect women at much higher rates than men. Other disorders are more common in men, including amyotrophic lateral sclerosis (ALS) and gout.
1.2.3 Ethnicity
Closely related to genetics, ethnicity is associated with predisposition for some conditions. A few examples are hypertension, sickle-cell disease and Tay-Sach’s disease. Hypertension occurs more commonly in African-Americans in the US than in any other racial or ethnic group.
Sickle-cell disease shows a strong correlation to people with African or Hispanic ancestry. Tay-Sach’s disease, a rare degenerative neurological disorder, is caused by a genetic mutation that is predominantly found in people of Aschkenazi (eastern and central European) Jewish heritage than in those with other backgrounds. The mutations responsible for this disease are also more common in certain French-Canadian communities of Quebec, the Old Order Amish community in Pennsylvania, and the Cajun population of Louisiana.
1.2.4 Geographical Location
Geography plays a role in the predisposition to disease. Conditions that are associated with certain insect vectors occur in areas where the particular insects are common. Lyme disease, which is transmitted to humans via deer ticks, is most likely to be seen in the northeastern US. Malaria, which is carried by the female Anopheles mosquito, commonly affects people living in Sub-Saharan Africa. On a smaller scale, pockets of disease outbreak put all people living in that area at higher risk for becoming infected. Recent cases of measles in some areas of the US have posed a higher-than-usual risk for people living in or visiting these areas, especially those individuals who have depressed immune systems.
1.2.5 Cultural Factors
Cultural beliefs, customs and practices can have a great affect on health and health care. The belief in “Western medicine” is very strong most Caucasians living in the US but is not accepted in all parts of the world or in all cultures, even within the US. Some cultural beliefs are inconsistent with preventative vaccination of children or other medical procedures. Culture also has a strong influence on dietary preferences, which can affect health. Some diets are more highly associated with consumption of fried foods and meats, which can lead to cardiovascular problems, while others are associated with greater consumption of fresh fruits and vegetables (Blue Zone), which positively correlates with longevity. Other cultural influences affecting health include the role of family in caring for elderly or unhealthy individuals, religious beliefs, and gender roles.
1.2.6 Socioeconomic Factors
Access to healthy lifestyles is often driven by socioeconomic factors. Medical, prescription drug, dental, and vision insurance, employment status, geographic location, access to transportation, educational level, exposure to high-risk behaviors, and family support structures are associated with socio-economic status and certainly impact health care. Socioeconomic status has been shown to have an inversely proportional relationship to health in the US.
1.3 ICF Disablement Model
In 2001, the World Health Organization (WHO) developed a conceptual model for discussing health and disability, the International Classification of Functioning, Disability, and Health (ICF). The American Physical Therapy Association (APTA) officially adopted this model in 2008. Prior to the ICF model, disease and disability were discussed in a linear manner according to the Nagi model:
Pathology —à Impairment –à Functional Limitation –à Disability
The development of the ICF model marked a shift in the way we talk about health and disability, including the integration of many factors and demonstrating the interconnectivity of all factors in the determination of health or disability.
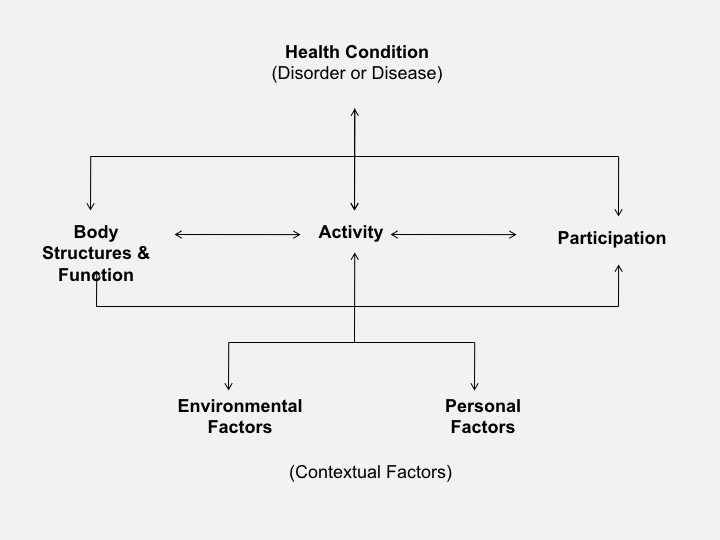
Long Description
Title: ICF Model
A top, middle and bottom arrangement is shown.
Top:
- Health Condition (Disorder or Disease)
Middle
- Middle left: Body Structures and Function
- Middle center: Activity
- Middle right: Participation
Bottom
- Bottom left: Environmental Factors
- Bottom right: Personal Factors
Health Condition (Disorder or Disease) is connected to Activity
Body Structures and Function is connected to Activity and Participation
Activity is connected to:
- Health Condition (above)
- Body Structures and Functions (left)
- Participation (right)
- Environmental Factors and Personal Factors (below)
Participation is connected to Activity and Body Structures and Function
Environmental Factors is connected to Activity and Personal Factors
Personal Factors is connected to Activity and Environmental Factors
The language in the ICF model is purposefully nonjudgmental. “Impairments,” “limitations,” and “disability” used in the Nagi model are negative terms. The newer terms, “body structures and function,” “activity,” and “participation” allow for all ability levels. This is important to remember as the same diagnosis in two different people might lead to very different activity levels and life situations, depending upon comorbidities, personal fortitude, and family and social support structures. Physical therapists and physical therapist assistants use the ICF model to develop and implement intervention plans that consider all aspects of a person’s life.
Definition of Terms in the ICF Disablement Model
- Body Functions are physiological functions of body systems (including psychological functions). This includes data such as muscle strength, joint integrity and range of motion, cardiovascular and respiratory functioning and endurance, integumentary status and neurological functioning.
- Body Structures are anatomical parts of the body such as organs, limbs and their components.
- Activity is the execution of a task or action by an individual. Examples of activities are raising the arm overhead, squatting, walking, running, and operating a wheelchair.
- Participation is involvement in a life situation. Participation includes engaging in activities such as household tasks, participating in a sport or recreational activity, driving a car, and going to work.
- Environmental Factors make up the physical, social and attitudinal environment in which people live and conduct their lives.
- Personal Factors include an individual’s age, cognitive status, and personality.
Introduction to Pathophysiology Resources:
Section: 1.3
Resource 01 – ICF Model Disablement Model – Author: Renee Borromeo

