Chapter 11: Peripheral Nervous System Injuries and Conditions
Learning Objectives
After completing this chapter, the students should be able to:
- Briefly discuss the component of and organization of the peripheral nervous system (PNS).
- Contrast the PNS with the central nervous system (CNS).
- Describe the different classifications of injuries and conditions affecting the PNS.
- Describe several PNS disorders, including:
- Hereditary: Charcot-Marie-Tooth Disease
- Mechanical: Carpal Tunnel Syndrome, Sciatica, Radial nerve palsy, Bell’s palsy
- Metabolic: Diabetic Neuropathy, Alcoholic Neuropathy
- Infectious: Gillian-Barre Syndrome
- Discuss each of the above disorders in terms of etiologies, risk factors, progression, prognosis, and intervention.
- Discuss the role of the PTA in the management of each of the conditions.
Chapter Contents
- 11.1 Introduction to the Peripheral Nervous System
- 11.2 Definitions and Key Terms
- 11.3 Hereditary Conditions: Charcot-Marie-Tooth Disease
- 11.4 Mechanical Injuries (Radial Neuropathy, Bell’s Palsy, Carpal Tunnel Syndrome, Lumbar Radiculopathy)
- 11.5 Metabolic Conditions
- 11.6 Infectious Conditions: Gillain-Barre Syndrome
11.1 Introduction
For a good overall review of the peripheral nervous system, please view the following:
11.1 – Resource-01 – “Introduction to the peripheral nervous system” by Andrew Wolf is licensed under Fair Use
11.2 Definitions and Key terms
The peripheral nervous system includes somatic motor and sensory components of cranial and spinal nerves whose cell bodies are in the brain stem and spinal cord or in dorsal root ganglia, so sensation and/or movement can be affected with a peripheral nerve injury. Autonomic nervous system fibers are also included in the peripheral nerves. If autonomic nerves are damaged, symptoms such as sweating and vascular changes are noted.
PNS injuries can be classified as demyelination or degeneration. In demyelination, the myelin sheath which surrounds the axon becomes fragmented or lost, so that conduction along the nerve is slowed. In a degenerating PNS injury, the axon atrophies and dies.
Further classifications of PNS injuries are listed below:
- Neurapraxia: segmental demyelination due to compression and mild ischemia; myelin dysfunction; mildest form of peripheral nerve injury; recovery in 4-6 weeks
- Axonotmesis: axonal damage, intact connective tissue coverings; due to prolonged compression, traction, crush injury; distal Wallerian degeneration can occur; spontaneous regeneration possible, may be spotty or incomplete
- Neurotmesis: complete severance of axon plus disruption of coverings complete transection of nerve trunk, as in gunshot or knife wound; Wallerian degeneration occurs distal to the axonal damage; flaccid paralysis and lack of sensation; no regeneration possible, unless surgical reattachment occurs soon after injury
A more detailed explanation of these types of injuries can be viewed below.
11.2 – Resource-01 – “Neurology – Nerve Damage and Regeneration” by Armando Hasudungan is licensed under Fair Use
Check Your Knowledge
PNS injuries can also be classified by the number of peripheral nerves that are affected or the area of damage:
- Mononeuropathy: single peripheral nerve is affected
- Polyneuropathy: several peripheral nerves involved
- Radiculoneuropathy: nerve root is involved as it emerges from spinal cord
- Polyradiculitis: involvement of several nerve roots; occurs in infections
- Myopathy: involves muscle
When the sensory components of a peripheral nerve are involved, the loss of sensory function follows nerve distribution in the region or, in the case of lesion of the spinal nerve or dorsal root ganglia, in a dermatomal pattern.
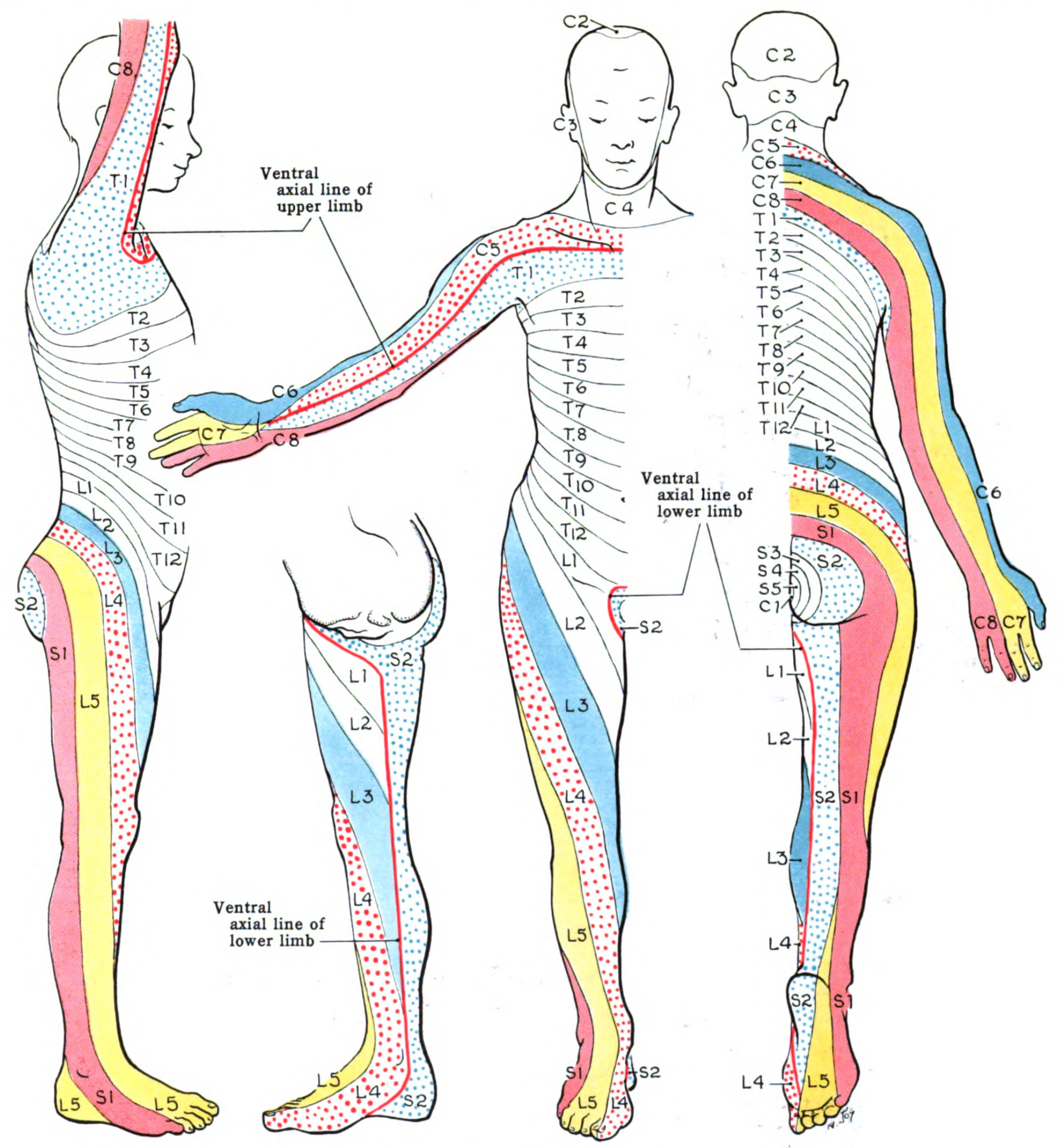
If the motor components of a peripheral nerve are affected, the loss of motor function occurs in muscles innervation by a particular nerve and its motor units distal to the lesion. If the lesion is in the spinal motor nerve, weakness will occur in a myotomal pattern.
There are four main categories of PNS dysfunction that are arranged according to cause of injury. These are: hereditary, mechanical, metabolic, and infectious. The remainder of this chapter will explore representative conditions in each of these categories.
11.3 Hereditary: Charcot-Marie-Tooth Disease
Charcot-Marie-Tooth (CMT) disease is a genetic disorder, which can be passed down through generations in recessive, dominant, and X-linked genetic patterns. There are as many as 120 variants of the disease. Most types become apparent in adolescence, but some do not become symptomatic until adulthood. Some are demyelinating in nature, others cause axonal degeneration. The most common type of CMT causes weakness and atrophy of the lower legs. As the disease slowly progresses, the hands are affected and the sensation of both hands and feet is altered. Numbness, tingling, and pain are common in the distal periphery. In rare types of the disorder, muscles of chewing, swallowing and breathing can be affected.
A cavus foot with hammer toes is typical of a patient with CMT. The fibular (peroneal) muscles are usually the first to be involved, followed by the anterior and posterior tibial muscles, as the tibial nerve becomes involved. The gastrocnemius and soleus muscles are usually the last leg muscles to show weakness and atrophy.

Lack of sensation, decreased muscle strength, and joint instabilities in the feet and legs cause balance problems for people with CMT. They often present with a drop foot and high-steppage gait, which may cause them to need ankle-foot orthoses and assistive devices for ambulation.
In the upper extremities, distal sensory and motor changes are also apparent, although the upper extremities show involvement later in the disease process than do the lower extremities. Severe clawing of the hands and loss of sensation in the hands is possible, negatively affecting dexterity and hand use.
There is no cure for CMT. CMT does not affect life expectancy, unless swallowing and respiratory muscles are involved. Medications for pain relief are the most commonly prescribed drugs for the disease. Surgeries to correct musculoskeletal deformities caused by the disease are useful in some cases. Physical therapy is recommended for patients with CMT to maintain muscle strength, endurance, and joint range of motion. Stretching of tight structures is often necessary. Balance is often an issue, so balance training and fall prevention should be part of a PT program. Assistive devices and orthotics or braces might also be helpful in maintaining functional abilities and ambulation.
This NIH link takes you to a one-page fact sheet on CMT.
Check Your Knowledge
11.4 Mechanical Injuries (Radial Neuropathy, Bell’s Palsy, Carpal Tunnel Syndrome, Sciatica/Lumbar Radiculopathy)
11.4.1 Radial Neuropathy/ Radial Mononeuropathy/ Radial Nerve Palsy/ Saturday Night Palsy/ Honeymooner’s Palsy
Radial nerve palsy is a compression injury to the radial nerve that occurs from compression of the radial nerve, most often while sleeping. The injury is most often in the category of neurapraxia but can be axonotmesis if the compression is long-standing. The result of the compression is the inability to extend the wrist and fingers, or wrist drop. Sensation is also altered on the dorsum of the hand. If the injury is in the axilla or mid-humerus, supination of the forearm and elbow extension can be weak.
For a good picture of radial nerve palsy (Saturday night palsy), watch the following patient video.
11.4 – Resource-01 – “Saturday Night Palsy” by Larry Mellick is licensed under Fair Use
Physical therapy can be beneficial for patients recovering from radial nerve injury. Interventions include range of motion, strengthening, and sometimes stretching. A cock-up splint for the wrist can hold the wrist and hand in a neutral position to assist in the use of the hand and help prevent contractures of the wrist flexors. Spontaneous recovery of both sensory and motor components of the radial nerve usually occurs in 1-2 months.
Check Your Knowledge
- Why does the patient in the video demonstrate weak grip strength on the right side?
- When the doctor is checking the patient’s strength of the brachioradialis, he says it is fairly strong. Which other muscles might be recruited to make up for lack of strength of the brachioradialis? Which nerve innervates them?
11.4.2 Bell’s Palsy
Bell’s palsy affects the facial nerve (cranial nerve VII). The most obvious symptom of Bell’s palsy is unilateral facial droop, especially noticeable around the eye and mouth. Inability to close the eye can lead to dryness of the eye, and inability to close the mouth can cause drooling. Patients with Bell’s palsy also report ear pain before or during an attack. The etiology of Bell’s palsy is unknown, but it seems to be linked to a viral infection, most likely a form of herpes simplex/ herpes zoster. During an attack, demyelination of the facial nerve, and sometimes axon damage occurs as a result of inflammation of the nerve.
Bell’s palsy is a common disorder, most often seen in people between the ages of 15 and 45. Risk factors include diabetes, recent upper respiratory tract infection, and pregnancy. It is a temporary condition that usually comes on over 48 hours and usually resolves within 2 weeks. In some cases, the condition can last much longer, however.
The condition can range from very mild to quite severe, both in terms of pain and weakness. Medical interventions often include high doses of corticosteroids to lessen the inflammation, anti-viral medications to kill the virus, and pain medications, if necessary. Physical therapy can be beneficial to stimulate the facial nerve (electrical stimulation), massage the facial muscles, and provide instruction for facial muscle exercises.

A short video on Bell’s palsy can be viewed below.
11.4 – Resource-03 – “Bell’s Palsy – causes, symptoms, diagnosis, treatment, pathology” Osmosis is licensed under Fair Use
Check Your Knowledge
11.4.3 Carpal Tunnel Syndrome
For a quick lesson on carpal tunnel syndrome (CTS), please view the following video:
11.4 – Resource-04 – “Carpal tunnel syndrome – causes, symptoms, diagnosis, treatment & pathology” Osmosis is licensed under Fair Use
CTS is a compression of the median nerve in the carpal tunnel. The etiology of the disorder is unknown, but risk factors include obesity, pregnancy, rheumatoid arthritis, hypothyroidism, diabetes, and trauma. Genetics also seem to play a role, but a specific gene for CTS has not been identified. Overuse and abnormal biomechanical stresses to the elements included in and surrounding the carpal tunnel are often cited as causes of CTS, but a cause-effect relationship has not been established. Repetitive work with the wrist, hand, thumb, and fingers can exacerbate the condition, however.
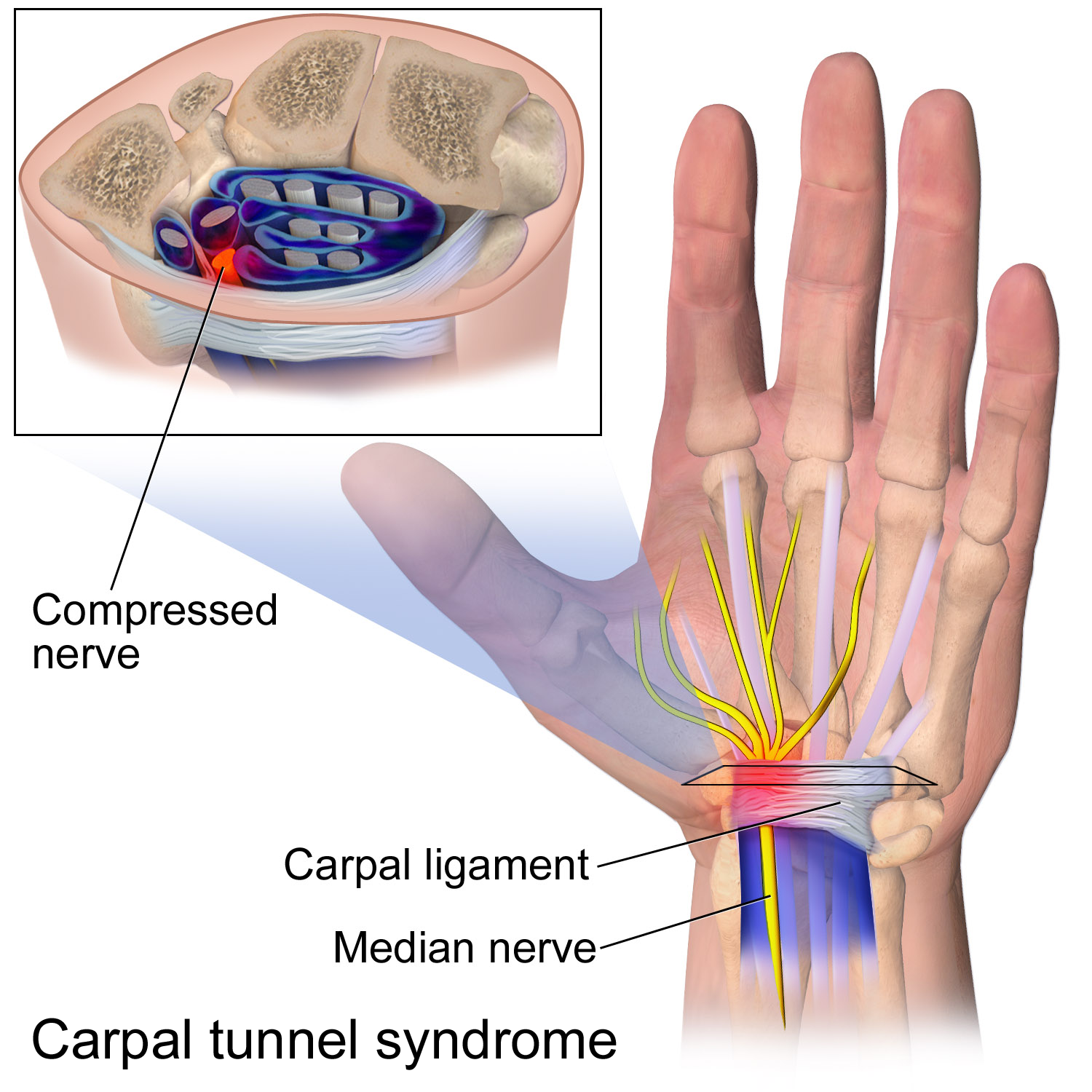
The signs and symptoms of CTS include tingling or numbness in the median nerve distribution in the hand and weakness of the thenar muscles. Sensory changes appear first, and muscular weakness and atrophy usually only appears in untreated CTS. Pain can accompany CTS, usually most evident in the morning and in the evening.

Treatment for CTS is directed at decreasing pressure on the median nerve. Injected or oral corticosteroids are useful in decreasing inflammation in the carpal tunnel. Splinting the wrist in a neutral position often helps relieve symptoms. Physical therapy, including stretching and ROM activities should be implemented, as these therapies may be adequate to relieve symptoms for some patients. Surgical intervention to release the transverse carpal ligament is often necessary, and generally yields good results.
Test Your Knowledge
11.4.4 Sciatica/ Lumbar radiculopathy
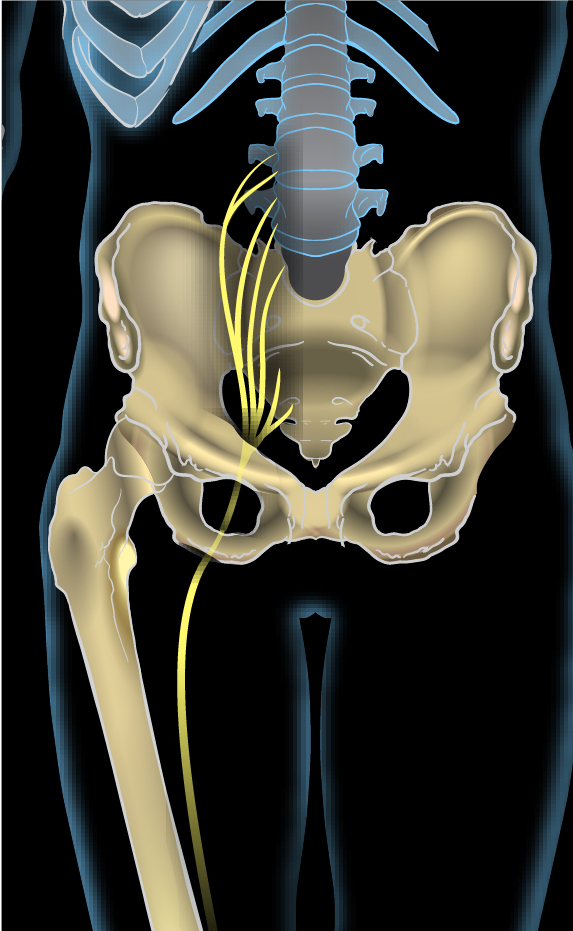
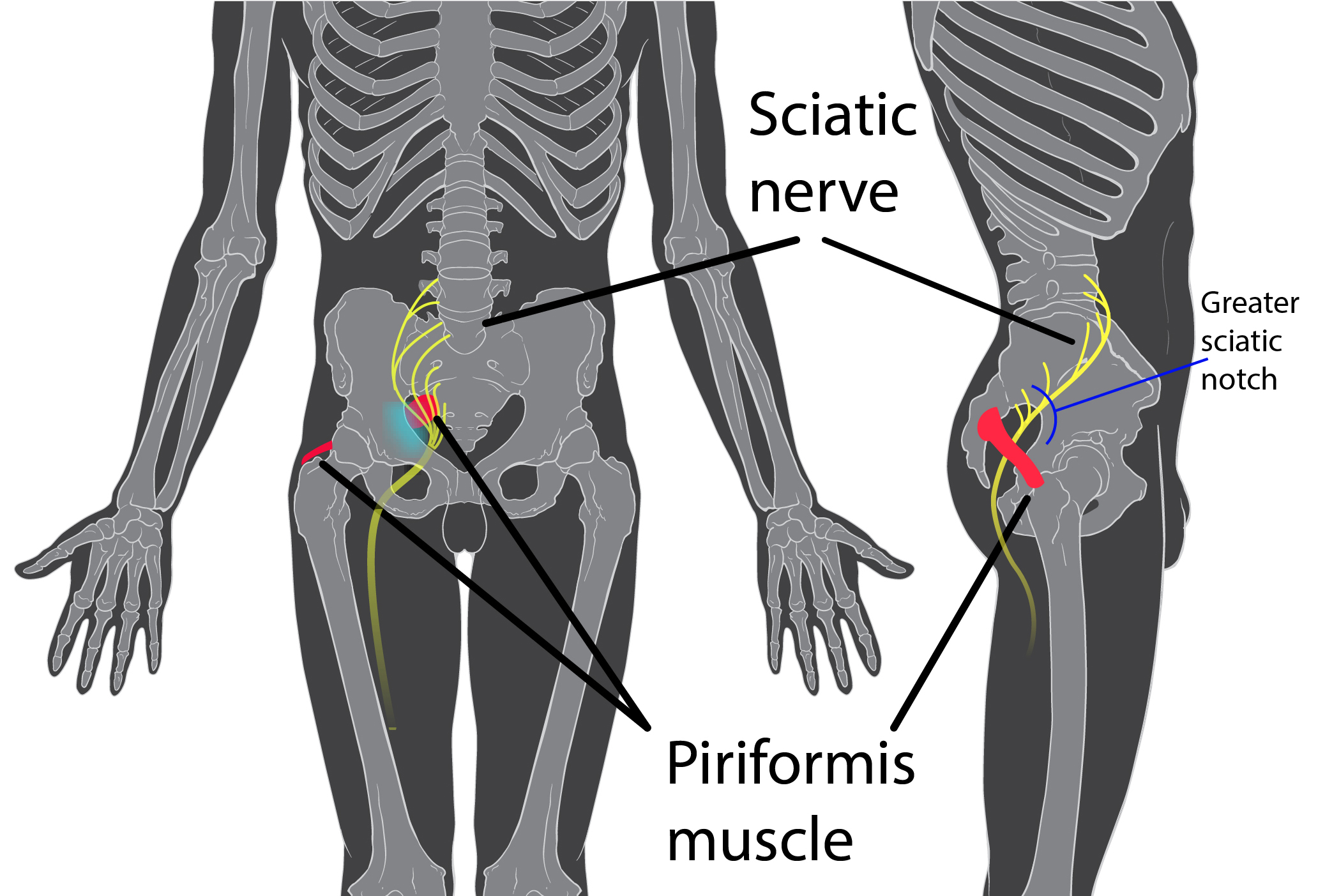
Sciatica is a common disorder causing pain, sensory changes, and weakness in nerve distribution areas of the sciatic nerve (L4, L5, S1, S2, S3). Symptoms occur anywhere along the nerve in the lower back, gluteal region, posterior thigh, posterior calf, or lateral ankle and foot. The symptoms are often considered radicular, that is that the pain is felt somewhere along the nervous pathway, but not at the location of the actual problem. Several different conditions can cause sciatica, including bulging or herniated disc, spinal stenosis and other arthritic changes, spondylolisthesis, piriformis syndrome, or pregnancy. Other less common causes of sciatic pain include tumor, infection, and blood clots. Most of the time, the condition is one-sided, but bilateral involvement is possible. Pain can be elicited with a straight leg raise, which stretches the sciatic nerve. Muscular weakness associated with sciatic generally appears most noticeably in the ankle dorsiflexor muscles.
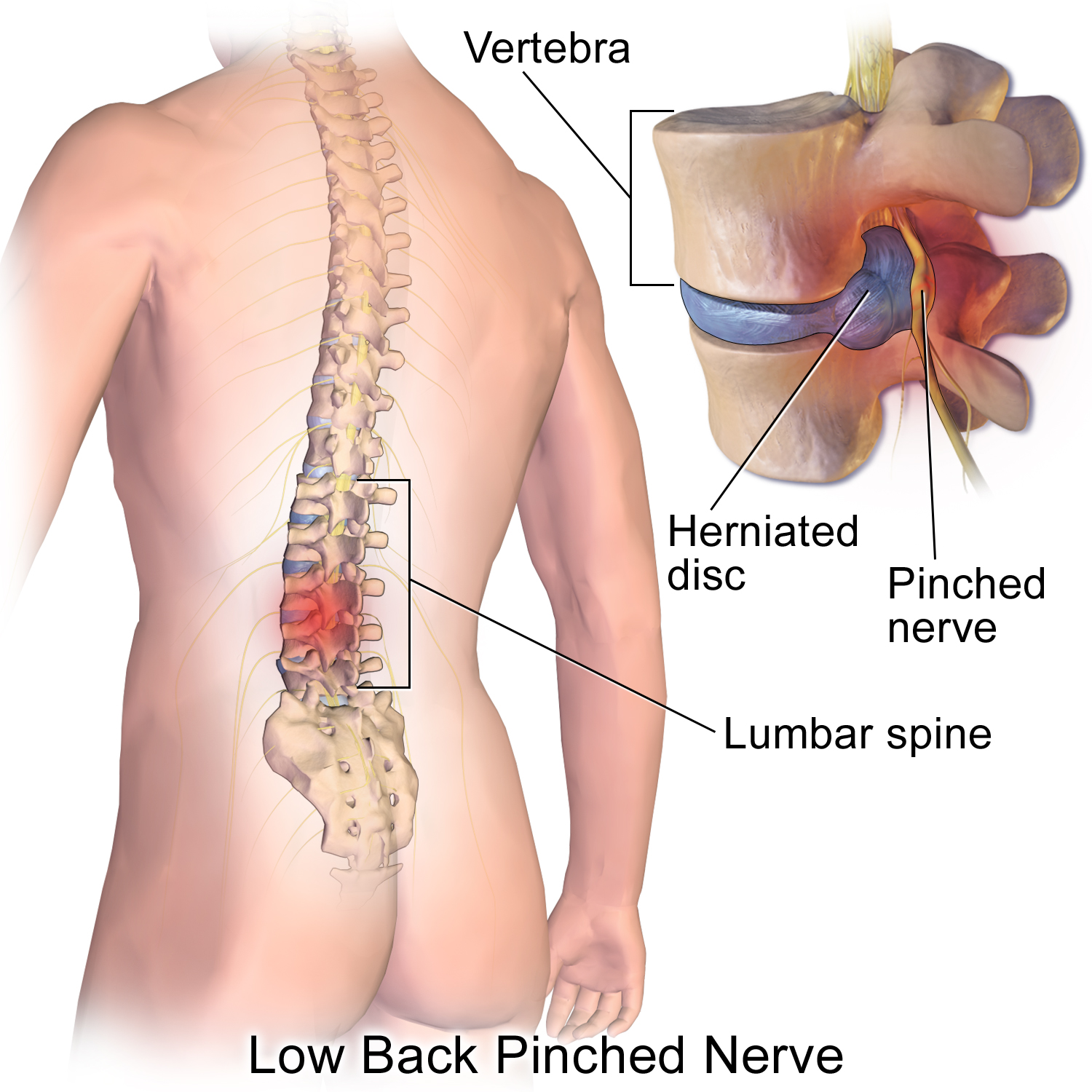
A bulging or herniated disc in the lumbar spine can put mechanical pressure on the nerve root as it exits the spinal canal. This can be very irritating to the nerve and pain or other sensory changes can be perceived by the patient at areas distant from the disc herniation. Patients might feel the pain from a herniated disc in the posterior thigh or even the calf or lateral foot. The pain can occur suddenly, associated with lifting or twisting of the spine, or it can have a more insidious onset. Patients report pain with sitting, forward bending, twisting, coughing, and sneezing.
In piriformis syndrome the piriformis muscle is short or stiff and puts pressure on the sciatic nerve as it courses beneath the muscles. In some people, the sciatic nerve actually courses through the piriformis muscle, causing then to be especially susceptible to sciatica.
Because sciatic is painful and can involve inflammation, especially in the acute stages, medications including corticosteroids (oral or injected) and NSAIDs are often prescribed. Muscle relaxants are also useful, as muscle spasms can occur in response to the sciatic pain. Physical therapy is very important for patients with sciatica. Range of motion and stretching can be used to lengthen short or stiff muscles, especially in the case of piriformis syndrome. Other muscles that are commonly short or tight include the hamstring group. For disc lesions, motions that emphasize spinal extension (increase lumbar lordosis) are recommended. Although it is wise to avoid activities that irritate the condition, bed rest or other forms of immobility should be avoided. Cardiovascular endurance should be included in a physical therapy program. Aquatic activities (swimming, water walking), stationary bike, and walking activities are usually well-tolerated and beneficial. Postural correction and education might be important, as posture in sitting, standing and during other activities could be predisposing a patient to sciatic pain.
If the problem is a disc that is bulging or herniated, conservative treatment as described above should help resolve the pain in a matter of weeks or months. Some patients will elect to undergo surgical procedures to relieve the disc pressure. These include discectomy, laminectomy, chemonucleolysis, laser discectomy or laminotomy.
If the source of the pain was piriformis syndrome, daily stretching of the piriformis and postural exercises should decrease the stress on the sciatic nerve and pain should be relieved.
Pain that occurs from stenosis, spondylolisthesis, or other bony changes can be somewhat relieved through conservative measures and changes in activities or postures during activities. Many patients with arthritic or bony issues will choose surgical intervention to relieve pressure on the spinal nerves. These surgeries are usually laminectomies and spinal fusions.
Check Your Knowledge
11.5 Metabolic Neuropathy
11.5.1 Diabetic Neuropathy
Diabetic neuropathy affects all areas of the body. Problems include sensory and motor losses in the extremities, visual disturbances, swallowing dysfunction, urinary incontinence, and erectile dysfunction. For the purposes of this text, only the problems associated with loss of sensory and motor neurons to the extremities will be discussed.
Many people with diabetes mellitus develop peripheral neuropathy because of poor oxygenation of small nerves in the extremities. The prolonged effect of exposure to high levels of blood glucose is presumed to have a negative effect on the small nerves of the periphery. The neuropathy takes on a stocking (or in the hand, glove) pattern, as many nerves are involved. This is considered a polyneuropathy. Sensory changes and motor weaknesses in a symmetrical pattern are characteristic of diabetic neuropathy. Pain in the extremities affected by diabetic neuropathy is also a concern. Autonomic nervous involvement may also be apparent in some patients.
Gait deviations are common in patients with diabetic neuropathy, due to poor sensation and lack of muscle strength in the lower extremities. Balance assessment and training, and gait training with an assistive device is often necessary. Patients with diabetic neuropathy are at risk for skin lesions, especially in the feet. These can lead to ulcers, gangrene, and ultimately, amputation.
Blood glucose levels need to be closely monitored in patients with diabetes. Prevention of diabetic neuropathy through maintenance of appropriate blood glucose levels is prudent and should be encouraged by all members of the health care team. Once neuropathy is present, physical therapy can be useful for balance and gait training activities. Cardiovascular and muscular endurance should be emphasized to maintain good blood flow throughout the body and limbs. PTs and PTAs should encourage patients to check their feet daily, avoid barefoot walking, and select good-fitting appropriate footwear to avoid damage to the skin on the feet. If a skin lesion or ulceration should be detected, immediate attention to eliminating causes of irritation or possible sources of infection is essential. Physical therapy interventions for skin breakdown and wounds includes wound care techniques, such as debridement, dressing changes, and application of products to assist in wound healing. PTAs do not perform sharp debridement (scalpel, scissors, tweezers), but can perform other aspects of wound care.
If amputation is necessary, PTs and PTAs will be involved in wound care and wrapping of the residual limb, positioning and stretching to avoid or correct contractures, and fitting and gait training with a prosthesis.
If pain is a problem for patients with diabetic neuropathy, medications to reduce pain are prescribed. Medication options for pain control include antiepileptic drugs (AEDs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs) and capsaicin cream.
11.5.2 Alcoholic Polyneuropathy / Alcoholic Neuropathy
Alcoholic neuropathy, or more correctly, alcoholic polyneuropathy because of the number of neurons involved, is a disorder caused by chronic alcoholism and nutrient deficiency. It involves demyelination and axonal degeneration of many different neurons at once in the distal extremities. Both sensory and motor neurons are affected, so the symptoms include pain, paresthesia, decreased sensation, and muscular weakness in the hands and feet. As the disease progresses, symptoms emerge more proximally. The condition is not life-threatening, but it does adversely affect the quality of life. Pain can be debilitating, and patients are at risk for falls and inadequate wound healing.
Alcoholic polyneuropathy is treated most effectively by the abstention from alcohol and attention to adequate nutrition. The symptoms can decrease or disappear completely if abstention from alcohol is implemented early in the disease. Unfortunately, many people who are alcoholic are unable to discontinue alcohol use, they may be faced with permanent disability. Medications to alleviate pain can be prescribed. Over the counter medications, such as aspirin, acetaminophen, or ibuprofen are often the drugs of choice. If prescription drugs are necessary, tricyclic antidepressant medications (amitriptyline) are used. Anticonvulsants and capsaicin are also used.
Physical therapy can be employed for patients with alcoholic polyneuropathy. Muscle strengthening, gait training, balance training, and cardiovascular endurance training are the most often used interventions in physical therapy.
For a good look at polyneuropathies, in general, watch this video:
11.5 – Resource-01 – “Polyneuropathy” by Matthew B. Jensen is licensed under Fair Use
11.6 Infectious Polyneuropathy: Guillain-Barre Syndrome (GBS)/Acute Inflammatory Demyelinating Neuropathy
Guillain-Barre Syndrome is a polyneuropathy that is caused by a reaction to a viral infection, surgery or vaccination. Sometimes, the cause is unknown. It is believed that the immune system “sees” the proteins coating myelin surrounding axons as very similar to the protein markers on virus or bacterial pathogens and continues to destroy myelin after the infectious agents have been removed from the body. Sensory losses often precede motor losses, but both afferent and efferent nerves are affected. This condition generally begins in the feet and hands and progresses proximally over the course of a few hours, days, or weeks. The symptoms include pain, loss of sensation, and muscle weakness in the most distal parts. Deep tendon reflexes can be absent. In some cases, the condition spreads rapidly, involving muscles of respiration, in which case it can be life-threatening. Also, sometimes the autonomic nerves are affected, causing dangerous changes in heart rate and blood pressure.
For most patients, spontaneous full recovery occurs, but may take weeks, months or years. Some patients experience lasting neurological deficits, and less than 10% succumb to the disease. Plasmapheresis and intravenous immunoglobulins (IVIG) are the two main immunotherapy treatments for GBS. Plasmapheresis attempts to reduce the body’s attack on the nervous system by filtering antibodies out of the bloodstream. Similarly, administration of IVIG neutralizes harmful antibodies and inflammation. Pain-reducing medications are also used in treating GBS.
Physical therapy is a very important component of the treatment of GBS. Muscle strengthening, endurance training, and gait training are the main goals of PT interventions. Splints, orthotics, and assistive devices are sometimes helpful in returning patients to functional activities.
The prognosis of GBS is considered to be generally positive, with most people regaining muscle strength, sensation, and pre-disease activity levels. Some, however, continue to have pain, weakness, and abnormal sensations throughout life. Older patients and those with longer lasting acute phases of GBS are more likely to have poorer outcomes.
Link to Wikimedia page with above animation.
11.6 – Resource 02 – Guillain-Barre Syndrome – causes, symptoms, diagnosis, treatment, pathology by Osmosis is licensed under Fair Use
Test Your Knowledge
Peripheral Nervous System Injuries and Conditions Resources:
Section 11.1
Resource-01 – “Introduction to the peripheral nervous system” by Andrew Wolf is licensed under Fair Use
Section 11.2
Resource-01 – “Neurology – Nerve Damage and Regeneration” by Armando Hasudungan is licensed under Fair Use
Resource-02 – “File:Grant 1962 663.png” by Grant, John Charles Boileau is in the Public Domain
Section 11.3
Resource-01 – “File:Charcot-marie-tooth foot.jpg” by Benefros, English Wikipedia is licensed under CC BY-SA 3.0
Section 11.4
Resource-01 – “Saturday Night Palsy” by Larry Mellick is licensed under Fair Use
Resource-02 – “File:Bellspalsy.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0
Resource-03 – “Bell’s Palsy – causes, symptoms, diagnosis, treatment, pathology” Osmosis is licensed under Fair Use
Resource-04 – “Carpal tunnel syndrome – causes, symptoms, diagnosis, treatment & pathology” Osmosis is licensed under Fair Use
Resource-05 –Anatomy of the carpal tunnel, showing the median nerve passing through the tight space it shares with the finger tendons – “File:Carpal Tunnel Syndrome.png” by BruceBlaus, Blausen.com staff is licensed under CC BY 3.0
Resource-06 – Untreated Carpal Tunnel Syndrome (Arrows point to atrophy of intrinsic thumb musculature)- “File:Untreated Carpal Tunnel Syndrome.JPG” by Dr. Harry Gouvas, MD, PhD is in the Public Domain
Resource-07 – Sciatic Nerve – “File:Sciatic nerve2.jpg” by KDS4444 is licensed under CC BY-SA 4.0
Resource-08 – Herniated Lumbar Disc – “File:Blausen 0484 HerniatedLumbarDisc.png” by BruceBlaus, Blausen.com staff is licensed under CC BY 3.0
Resource-09 –Location of piriformis syndrome within the body – “File:Piriformis syndrome.jpg” by Patrick J. Lynch & KDS4444, Blausen.com staff is licensed under CC BY-SA 2.5
Section 11.5
Resource 01 – . “File:Guillain-barré syndrome – Nerve Damage.gif” by Doctor Jana is licensed under CC BY 4.0 International
Resource 02 – Guillain-Barre Syndrome – causes, symptoms, diagnosis, treatment, pathology by Osmosis is licensed under Fair Use

