Chapter 10: Stroke, Traumatic Brain Injury, and Concussion
Learning Objectives
After completing this chapter, the student should be able to:
- Identify the different types of strokes, in terms of etiology, risk factors, pathophysiology, interventions, and outcomes.
- Discuss the role of the PTA in the identification of stroke or risk of stroke.
- Discuss the role of the PTA in physical therapy interventions in stroke rehabilitation.
- Identify risk factors for traumatic brain injury.
- Contrast different types of traumatic brain injury and implications for medical intervention and prognosis with each.
- Discuss primary and secondary conditions associated with traumatic brain injury.
- Discuss the role of the PTA in physical therapy interventions in the rehabilitation of patients with traumatic brain injuries.
- Identify signs of concussion.
- Discuss the appropriate interventions following concussion.
- Discuss the role of the PTA in physical therapy interventions following concussion.
Chapter Contents
10.1 Stroke or Cerebral Vascular Accident (CVA)
A stroke or cerebral vascular accident (CVA) can be a life-changing event for a patient and their family. In the following paragraphs we will explore the different kinds of CVAs, risk factors, interventions, and prognoses for each.
As an introduction to stroke and TIA, please go to the NIH webpage and view the video.
Strokes can be divided into two broad categories: ischemic and hemorrhagic. The etiologies and pathophysiologies are different for the two types, but the signs and symptoms and physical therapy interventions are similar. The following video provides a general introduction to these two types of stroke.
10.1 – Resource 01 – “Khan Academy – What is a stroke?” by Vishal Punwani, Khan Academy is licensed under Fair Use
Signs and symptoms of stroke are described in the following video.
10.1 – Resource 02 – “Khan Academy – Common Stroke Signs and Symptoms” by Vishal Punwani, Khan Academy is licensed under Fair Use
Test Your Knowledge
10.1.1 Ischemic Stroke
Ischemic stroke is the most common form of stroke, responsible for approximately 80-85% of all strokes. An ischemic stroke is caused by an accumulation of atherosclerotic plaque in a blood vessel in the brain, or by an embolism to the brain from the left heart, aorta, or other blood vessel leading to the brain. A blood vessel that is occluded is unable to deliver oxygen and nutrients, namely glucose, to the brain. If this condition lasts more than a few minutes, brain cells will die. If enough brain cells die, tissue necrosis occurs, and that potion of the brain will cease to function. The severity of the stroke is very much dependent upon the location of the blockage and the time lapse before medical intervention.
Ischemic strokes are explained in the following video.
10.1 – Resource 03 – “Khan Academy – Ischemic Stroke” by Vishal Punwani, Khan Academy is licensed under Fair Use
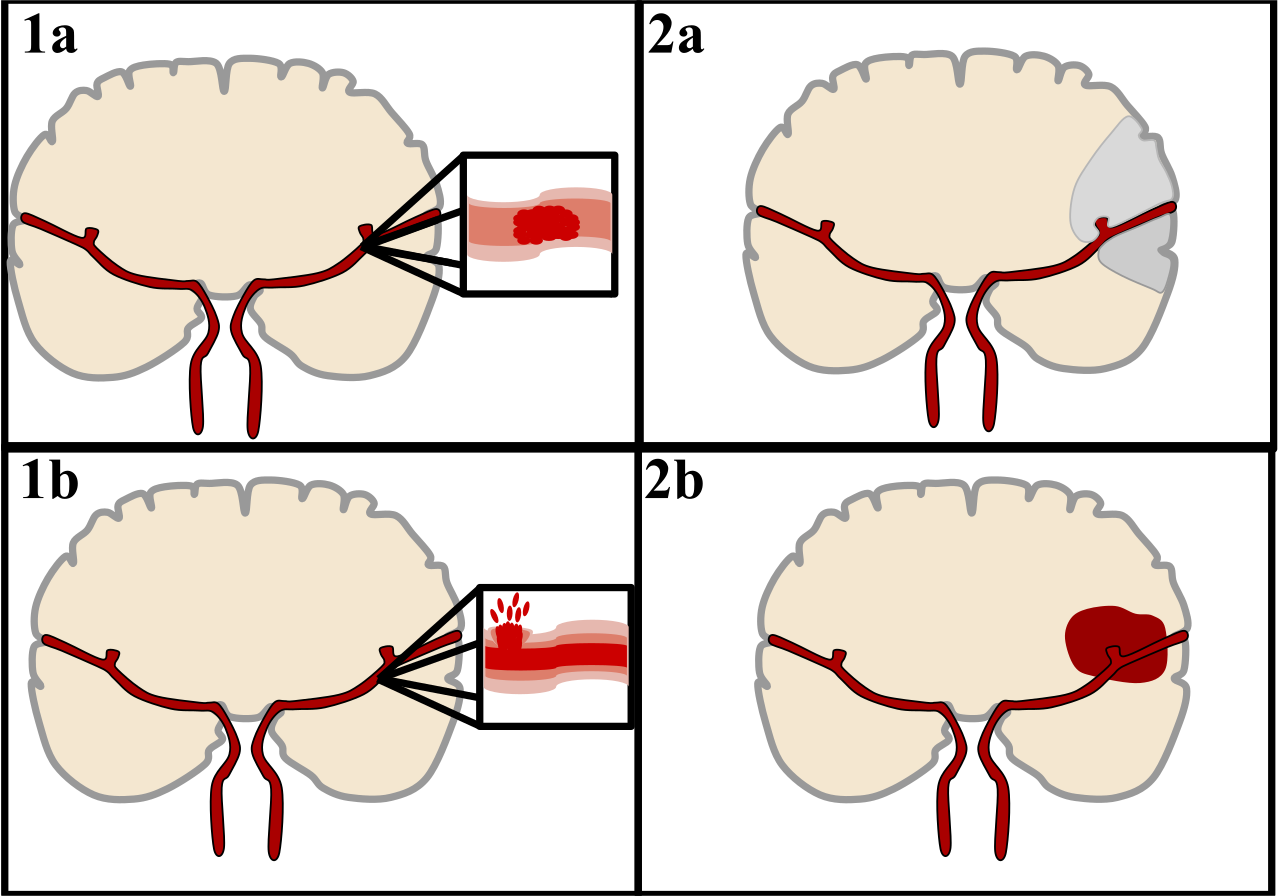
There are two main categories of strokes. Ischemic (top), typically caused by a blood clot in an artery (1a) resulting in brain death to the affected area (1b). Hemorrhagic (bottom), caused by blood leaking into or around the brain from a ruptured blood vessel (2a) allowing blood to pool in the affected area (2b) thus increasing the pressure on the brain.
10.1.2 Hemorrhagic Stroke
A hemorrhagic stroke occurs when a blood vessel in the brain bursts or leaks. When this happens, blood escapes into the outer portions of brain tissue, creating pressure on the brain. At the same time, blood is unable to get to portions of the brain beyond the area of hemorrhage, so those areas do not receive the oxygen and glucose they need for survival. So, the problems with the hemorrhagic stroke are twofold: pressure and ischemia. The effects of the stroke and the prognosis depend upon the area of damage, the extent of damage, and the timeliness of medical intervention. The two major types of hemorrhagic stroke are intracerebral hemorrhage subarachnoid hemorrhage.
Hemorrhagic strokes are explained in the following video.
10.1 – Resource 05 – “Hemorrhagic strokes | Circulatory System and Disease | NCLEX-RN | Khan Academy” khanacademymedicine is licensed under Fair Use

CT scan of an intraparenchymal bleed (bottom arrow) with surrounding edema (top arrow)
10.1.2.1 Stroke Risk Factors
The major risk factor for stroke is hypertension. Other known risk factors include smoking, obesity, hyperlipidemia, diabetes mellitus, history of transient ischemic attacks (TIAs, see below), and atrial fibrillation. Although most people experiencing stroke will be older, a significant number of strokes occur at younger ages. Infants, children, and young adults can suffer from strokes. For younger people, an aneurysm or some other defect in a blood vessel in the brain is generally the cause.
10.1.2.2 Stroke Signs and Symptoms
A person who is experiencing a stroke will most often exhibit the following symptoms: drooping of facial musculature on one side, speech difficulties, such as slurring or incoherence, and weakness and/or abnormal sensations in one upper extremity. The pneumonic “FAST” is often used to help remember the signs of a stroke, with the final letter, T for Time, prompting quick medical attention.
F = Face drooping on one side. Ask your senior to smile – is it uneven?
A = Is one arm weak or numb? Ask them to raise both arms – is one arm weak?
S = Speech problems like slurring, inability to speak, being incoherent. Ask them to repeat a simple sentence like “The sky is blue” as a quick test.
T = Time to call 911. If you see any of these signs, even if the symptoms don’t last, call 911 right away and get to the hospital ASAP. Check the time so you can tell EMTs and doctors when the symptoms started.
Other symptoms that may occur include: weakness or numbness of one lower extremity, dizziness, loss of vision, inability to understand language, and occasionally headaches. Most strokes of the ischemic type do not include headache. Loss of consciousness and death may also occur, especially in the absence of prompt medical intervention.
10.1.2.3 Stroke Diagnosis and Medical Interventions
The most important intervention for stroke is prompt medical attention at the first sign of problems. MRIs and CT scans, and angiograms, along with clinical presentation are the most useful tools for identifying a stroke. Both ischemic and hemorrhagic stroke sites are visible on scans and the signs and symptoms are usually quite clear. EEGs often demonstrate abnormal electrical activity in the brain following a stroke.
In terms of treatment, the sooner appropriate drugs can be administered, the greater the chance decreased long-term disability. Medications for ischemic stroke are generally administered to destroy the thrombus and “thin” the blood. Recombinant tissue plasminogen activator (rtPA), the most commonly used antithrombotic medication for ischemic stroke is most effective when given within the first 3 hours of the stroke. Its effectiveness after 3 hours is marginal. Other anticoagulants, such as aspirin are also used to decrease the chance of further clotting.
For a hemorrhagic stroke, antithrombotic and anticoagulant medications are not used, as they would increase the loss of blood from the damaged blood vessel(s) in the brain. Instead patients are closely monitored, and oxygen and blood glucose levels are kept at optimum levels, or as close to optimum levels as possible. Surgical intervention might be necessary to drain blood that is putting pressure on the brain, or to try to repair damaged blood vessels.
10.1.2.4 Prognosis
Long term effects of stroke vary greatly in terms of severity and mode. One side of the body, that opposite from the side of the damage to brain tissue, is affected. Disabilities in sensation, speech, and motor functioning are common. Muscle tone is often decreased in the affected muscles, but over time, the hypotonia can be replaced by spasticity as the body learns to move with the abnormal signals from the brain. Also common are cognitive and affective (mood) impairments. Vision, hearing, smell, and taste can also be diminished or lost on one side. Recovery is very much dependent upon the area and severity of damage.
Physical therapy, along with occupational therapy and speech therapy, is involved in the rehabilitative care of individuals who have had a stroke. The goal for physical therapy is to restore function and retrain muscles for functioning in all aspects of everyday life. Assistive devices, such as rollator walkers, are useful for gait training, as balance and endurance can be diminished by the stroke and the period of immobility. Adaptations for assistive devices and other objects for self-care may need to be adapted if hand function and upper extremity use are adversely affected. There are many different approaches and exercise formats that can be employed by the PT and PTA, and each patient needs an individualized program. Recovery times and eventual outcomes will also vary, depending upon the type, location, and severity of stroke, the age, general health and fitness level of the patient, and the availability and quality of the rehabilitation. Supportive caregivers and access to follow-up care following the stroke are very important to overall recovery and quality of life.
10.2 Traumatic Brain Injury
Traumatic brain injury (TBI) is a condition that can occur at any age. The brain can be damaged through falls, automobile or boating accidents, sports injuries, assault, or child abuse. Risk factors for TBI include participation in high-risk activities, balance disorders, alcoholism and drug abuse. TBI is the most common cause of death in people ages 1-45.
The results of TBI vary greatly, depending upon the area of the brain that is injured and the severity of the trauma to the brain. Injuries can be focal, limited to a small area of the brain, or more global, when much or all the brain is damaged due to trauma and swelling. Long-term effects can include deficits in motor skills, speech, cognition and affect. The major factor for predicting outcome is age. The younger the brain, the more plastic it is. This means that younger brains are more capable of creating new circuits and re-establishing connections than are older brains. After the age of 40, the prognosis for complete recovery dramatically decreases. TBI has become a serious concern for the elderly. Increased life expectancy and improvements in treatments for many disorders associated with aging have led to greater numbers of people remaining mobile well into old age. As people age, their balance and coordination tend to diminish and their reflexes and reactions to postural changes and changes in supporting surfaces slows down. This leads to increased risk of falling, which leads to increased risk of TBI.
10.2.1 Types of Traumatic Brain Injury
There are two main types of brain injury, categorized by the mechanism of injury, blunt force (e.g. falls, car accidents) or penetrating (e.g. bullet wounds). Each of these categories can be further subdivided into high- or low-velocity. All are capable of producing devastating injuries, but generally, the higher the velocity, the more serious the TBI. A third category is diffuse axonal injury. Shaken baby syndrome is probably the most common cause of this type of injury, which causes twisting and tearing of axons in many parts of the brain. Communication within the brain is severely compromised, and the effects are generally severe and life-long.
Since the brain is floating in cerebrospinal fluid, it can be displaced within the skull in reaction to force. This phenomenon allows for the brain to be damaged at the point of impact (coup) and opposite the point of impact (countercoup). This occurs most often when the moving head meets a stationary object. The brain continues to move inside the skull after the skull stopped accelerating. In the case of a penetrating wound, shock waves are sent through the brain, which can cause damage in areas of the brain that are far away from the actual penetrating wound.
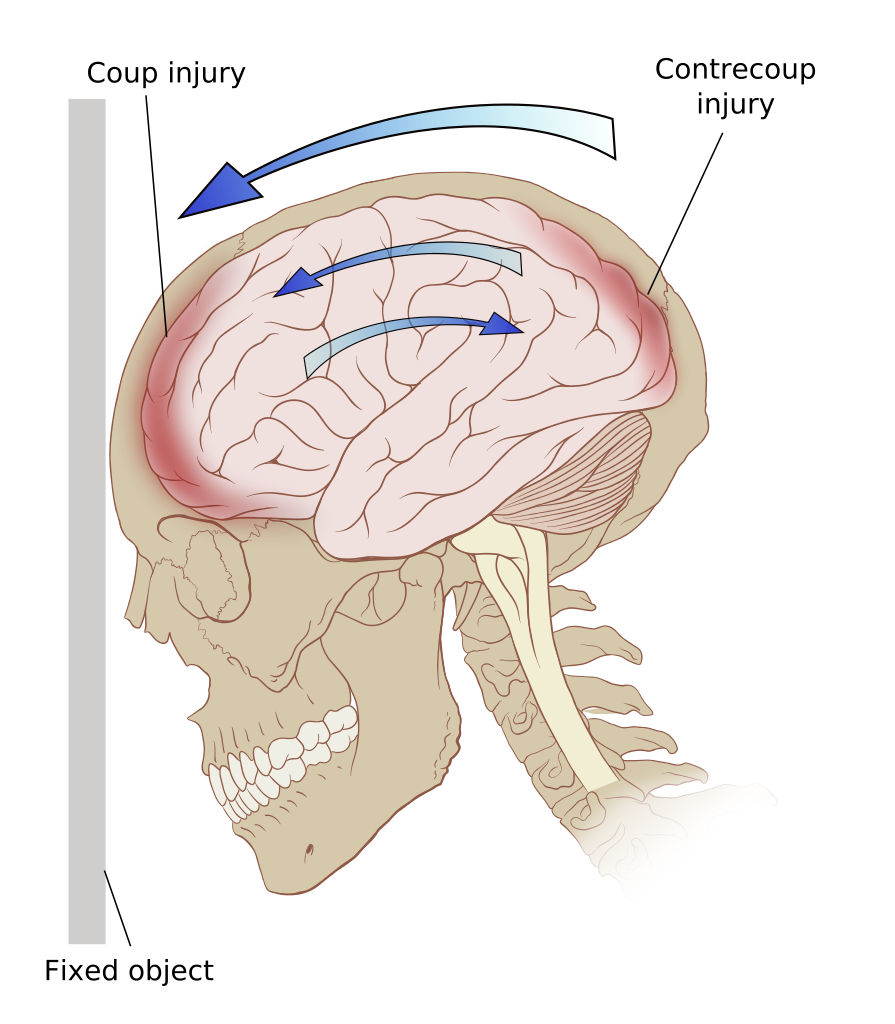
Blunt force trauma with coup and contrecoup injury (moving skull impacts stationary object)
10.2.2 Signs and Symptoms of Traumatic Brain Injury
The signs and symptoms of TBI include, bleeding or leaking of spinal fluid from the wound, ears, nose, mouth or eyes, loss of consciousness, sleepiness, confusion, inability to speak or move, pupil dilation or lack of reaction to light (especially uneven pupil size), visual loss or disturbance, hearing loss or disturbance, and nausea or vomiting. Symptoms of TBI are due to both the primary injury and from secondary injury to the brain as a result of the initial trauma. Secondary injuries may be due to swelling from direct pressure on brain tissue or lack of oxygen and glucose to the brain because of pressure, blood vessel rupture or decreased blood pressure.

Specific data collection of signs of TBI help determine the prognosis for recovery. The Glasgow Coma Scale is the most common tool used to determine the severity of injury and prognosis for recovery. The scale includes measures of verbal, motor, and eye-opening reactions in response to stimuli.
Glasgow Coma Scale
| Measure | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Eye | Does not open eyes | Opens eyes in response to pain | Opens eyes in response to voice | Opens eyes spontaneously | N/A | N/A |
| Verbal | Makes no sounds | Makes sounds | Words | Confused, disoriented | Oriented, converses normally | N/A |
| Motor | Makes no movements | Extension to painful stimuli (decerebrate response) | Abnormal flexion to painful stimuli (decorticate response) | Flexion / Withdrawal to painful stimuli | Localizes to painful stimuli | Obeys commands |
10.2 – Resource 03 – “Glasgow Coma Scale” Wikipedia Creative Commons Attribution-ShareAlike License 3.0
A score of 13 -15 on the Glasgow Coma Scale indicate a mild TBI. Scores of 9-12 indicate moderate TBI. Scores below 8 indicate a severe TBI.
8.2.3 Interventions
Some primary injuries, such as subdural hematoma, epidural hematoma, and subarachnoid hematoma are surgically treated with craniotomy to immediately relieve swelling and possibly repair damaged structures. The goal of acute treatment, including craniotomy, in TBI is to prevent secondary injuries. Other injuries, such as contusions in the brain tissue are generally just monitored for further injury as the body repairs itself. Shaken baby syndrome and other diffuse axonal injuries are also monitored, but prognosis is very poor.
Watch the following YouTube video to learn about TBI.
10.2 – Resource 04 – “Living With Traumatic Brain Injury” by University of California Television (UCTV) is licensed under Fair Use
10.2.4 Rehabilitation in TBI
Most patients with significant TBI will be hospitalized for long periods of time. In the acute phase, physical therapy can be beneficial for patients to help improve breathing and provide beginning mobility. Once they are medically stable, PT, OT, and Speech therapy can begin. Patient problems can include abnormal muscle tone, decreased muscle strength, decreased range of motion, decreased coordination, balance instabilities, and loss of motor planning abilities and judgement. Other cognitive limitations and speech and language difficulties are also often present. Physical therapy is provided to improve strength, range of motion, balance and coordination, endurance, and functional abilities. Patients in rehabilitation for TBI may receive 4-6 hours of PT every day for several months. Physical therapy interventions should be specific to the patient, considering his or her goals and prognosis. A supportive family or group is very helpful in assisting the patient to return to a fulfilling life.
Check Your Knowledge
10.3 Concussion
A concussion is a mild traumatic brain injury that affects brain function for a short period of time. Concussions occur in automobile accidents, with falls, in sports activities, and in bicycle accidents. Alcohol use is considered a significant risk factor for concussion. Signs of concussion include headache, cognitive changes, difficulty with memory or concentration, nausea, blurry vision, sleep disturbances or mood changes. Loss of consciousness, if present, must be less than 30 minutes, memory loss must be less than 24 hours, and the Glasgow Coma Scale score must be 13 to 15 for a diagnosis of concussion. The signs and symptoms of concussion can last only a few days or several weeks or months. Treatment includes initial resting of the brain, followed by gradual return to activity. Extended periods of lack of stimulation are not recommended. Physical therapy interventions are often directed at vestibular and balance activities improvement activities, with gradual return to sport or activity as postconcussion symptoms resolve. It is recommended that patients avoid activities which are associated with head injury (contact sports, horseback riding, etc.) until recovery is complete. Repeated mild traumatic brain injury is linked to the development of chronic traumatic encephalopathy (CTE), which is associated with the development of Alzheimer’s disease and other forms of dementia.
For a short explanation of the pathophysiology of concussion, view the following video.
10.3 – Resource 01 – “Concussion : Metabolic changes” by HeadWayAuckland is licensed under Fair Use
Check Your Knowledge
Other good resources on concussion can be found on the CDC webpage
Stroke, Traumatic Brain Injury, and Concussion Resources:
Section 10.1
Resource 01 – “Khan Academy – What is a stroke?” by Vishal Punwani, Khan Academy is licensed under Fair Use
Resource 02 – “Khan Academy – Common Stroke Signs and Symptoms” by Vishal Punwani, Khan Academy is licensed under Fair Use
Resource 03 – “Khan Academy – Ischemic Stroke” by Vishal Punwani, Khan Academy is licensed under Fair Use
Resource 04 – Two Main Categories of Stroke in Detail? – “File:Ischemic Stroke.svg” by ElinorHunt is licensed under CC BY-SA 4.0
Resource 05 – “Hemorrhagic strokes | Circulatory System and Disease | NCLEX-RN | Khan Academy” khanacademymedicine is licensed under Fair Use
Resource 06 – CT scan of an intraparenchymal bleed with surrounding edema –“File:Parachemableedwithedema.png” by James Heilman, MD is licensed under CC BY-SA 3.0
Section 10.2
Resource 01 – Blunt force trauma with coup and contrecoup injury – Picture of eyes after traumatic brain injury – “File:Contrecoup.svg” by Patrick J. Lynch, medical illustrator is licensed under CC BY 2.5
Resource 02 – Uneqal pupil sine in TBI – “File:Anizokoria.JPG” by Radomil is licensed under CC BY-SA 3.0
Resource 03 – “Glasgow Coma Scale” is licensed under
Resource 04 – “Living With Traumatic Brain Injury” by University of California Television (UCTV) is licensed under Fair Use
Section 10.3
Resource 01 – “Concussion : Metabolic changes” by HeadWayAuckland is licensed under Fair Use

