Chapter 19: Genital and Reproductive Systems
Learning Objectives
After completing this chapter, the learner should be able to:
- Define and discuss conditions involving the genital and reproductive systems for males and females.
- Discuss physiological changes associated with pregnancy.
- Discuss complications associated with pregnancy and childbirth.
- List and describe rationale for indicated and contraindicated physical therapy interventions in relationship to genital and reproductive conditions, including pregnancy and childbirth.
Chapter Contents
- 19.1 Female Reproductive System
- 19.2 Pregnancy
- 19.2.1 Factors that cause higher than average risk to a pregnancy include
- 19.2.2 Pregnancy Body Changes
- 19.2.2.1 Musculoskeletal and Neurological
- 19.2.2.2 Cardiovascular
- 19.2.2.3 Pre-eclampsia and Eclampsia
- 19.2.2.3 Pulmonary
- 19.2.2.4 Urinary
- 19.2.2.5 Digestive
- 19.2.2.6 Gestational Diabetes
- 19.2.2.6 Psychological and Emotional
- 19.2.3 Physical Therapy and Pregnancy
- 19.2.4 Exercise During Pregnancy
- 19.3 Male Reproductive System
- 19.3.1 Genetics
- 19.3.2 Cancer
- 19.3.3 Erectile Dysfunction (ED)
19.1 Female Reproductive System
The female reproductive system includes organs located in the pelvis: ovaries, fallopian tubes, uterus, cervix, and vagina. External structures include the labia and clitoris.
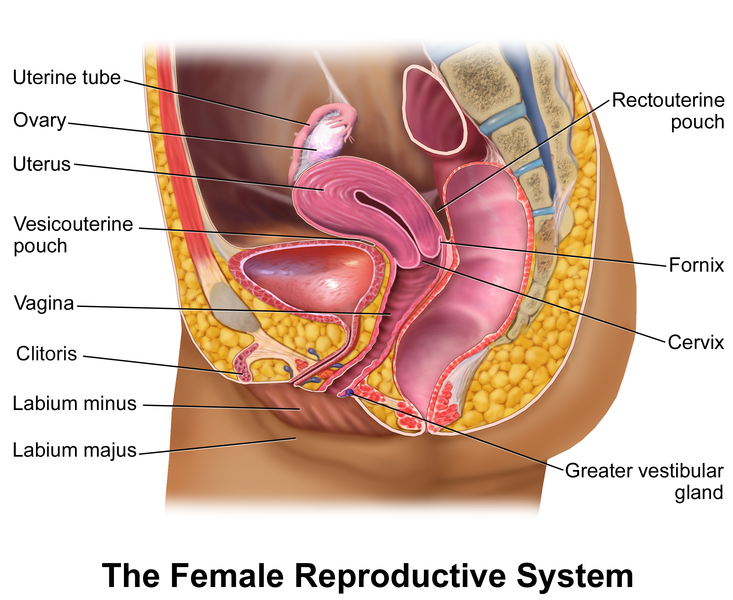
Long Description
The Female Reproductive System
An illustration with the following labels:
- Uterine tube
- Ovary
- Uterus
- Vesicouterine pouch
- Vagina
- Clitoris
- Labium minus
- Labium majus
- Rectouterine pouch
- Fornix
- Cervix
- Greater vestibular gland
Some general terms describing common conditions associated with the female reproductive system:
- Dysmenorrhea: pain during menstruation
- Amenorrhea: no period
- Menorrhagia, hypermenorrhea: very heavy blood flow or excessive length of period
- Premenstrual Syndrome (PMS): condition that affects a woman’s emotions, physical health, and behavior during certain days of the menstrual cycle, generally just before her menses; very common condition; affects more than 90 percent of menstruating women
- Menopause: in females, occurs when the ovaries stop producing the hormones estrogen and progesterone; can be associated with hot flashes, mood swings; risk of heart disease increases once a woman enters menopause (no period for one year)
- Dyspareunia: pain related to intercourse (physical/psychological basis of pain)
- Endometriosis: a condition in which endometrial tissue grows into other pelvic organs
- Hysterectomy: surgical removal of the uterus; may be recommended for uterine fibroids, cancers of the uterus, cervix, or ovaries, prolapse of the uterus, or endometriosis
- Oophorectomy: surgical removal of the ovaries; usually performed in the presence of cancer
- Mastectomy: surgical removal of breast tissue; excision of tissue can range from minimal tissue, as in lumpectomy, to removal of entire breast and underlying tissue; following surgical removal of the breast, reconstructive surgery can rebuild/replace breast tissue
- Anorexia nervosa: eating disorder seen most commonly in, but not exclusively in females; severely limited caloric intake; may cause amenorrhea and infertility
- Turner syndrome: a condition that affects only females, results when one of the X chromosomes (sex chromosomes) is missing or partially missing; can result in failure of ovarian development and delayed or incomplete development of secondary sexual characteristics; Turner syndrome places girls and women at elevated risk for : cardiac pathology, vision and hearing problems, high blood pressure, autoimmune disorders, learning disabilities, mental health and socialization issues, and infertility.
19.1.1 Etiologies of Conditions of the Female Reproductive System
The female reproductive system is related to other body systems and signs and dysfunction in any of the body systems can cause symptoms in the reproductive system. The endocrine system, in particular, can affect the functioning of the reproductive organs. The pituitary gland produces prolactin, which helps in milk production during breastfeeding; and luteinizing hormone, which manages estrogen in women. The ovaries produce estrogen and progesterone, which help develop breasts, regulate the menstrual cycle, and support pregnancy. They also produce the hormone, relaxin, which has been suggested to cause ligamentous laxity, allowing the bony pelvis to expand for delivery. Because autoimmune diseases (e.g. multiple sclerosis, rheumatoid arthritis, lupus erythematosus) are seen more often in women than in men, it is believed that the endocrine system and female hormones are associated with immune system dysfunction. Some conditions, such as Turner’s syndrome are caused by genetic anomalies. Turner’s syndrome results from ab absent or missing piece of one of the X chromosomes in females.
Many treatment options are available for management and/or cure for conditions of the female reproductive system. These include: hormone replacement therapy, surgery, chemotherapy, and radiation therapy.
19.1.2 Cancer and the Female Reproductive System
Cancerous conditions of the female reproductive organs are associated with various risk factors, including: heredity, obesity, age, diet and lifestyle, sexual activity, alcohol use, and exposure to some viruses, substances, and drugs. Breast cancer is the most common cancer in women. Cervical, ovarian, vaginal, and uterine cancers are also seen in women. There are some preventative measures for female cancers (breast exam, mammography, human papillomavirus (HPV) vaccine, pap smear, proactive mastectomy). When treatment is necessary, hormone replacement therapy, chemotherapy, radiation therapy, and surgery are utilized. More information on cancer in females can be located in the chapter on oncology.
19.1.3 Physical Therapy and the Female Reproductive System
Many conditions associated with women’s health and the health of the reproductive system can be addressed by physical therapy interventions. Indeed, the APTA recognizes Women’s Health as a specialty certification in physical therapy. Pelvic floor health and incontinence are topics included in this field. This text addresses those in the chapter on the urinary system. For women who are experiencing symptoms of pain or dysfunction of the reproductive organs, specific treatment plans can be developed by physical therapists and carried out by PTAs . Some of the more common physical therapy interventions include: therapeutic exercise, postural awareness and exercise, cardiovascular exercise, biofeedback, relaxation techniques, soft tissue mobilization, and modalities to manage pain, such as electrical stimulation, ultrasound, and thermal modalities.
19.1.3.1 Post-Surgical Physical Therapy Intervention
Following surgery, such as mastectomy, hysterectomy, or oophorectomy, physical therapy can be beneficial to reduce pain, improve mobility, improve strength and posture, improve wound healing and scar formation, and improve cardiovascular functioning. Massage techniques can be used to mobilize scars and diminish the proliferation of scar tissue and adhesions. Range of motion, stretching, and muscle strengthening activities can help improve mobility and function. Abdominal and pelvic surgeries increase the risk for the development of deep venous thrombosis (DVT) in the lower extremities, and physical therapy can address lower extremity mobility issues that could help prevent this and other vascular disorders. Any surgery can result in a general lack of mobility, which can lead to cardiovascular and cardiorespiratory conditions, so physical therapy can be beneficial for gait training, bed mobility, general exercise, and overall mobility training to help avoid negative outcomes following surgery.
19.2 Pregnancy
Pregnancy, also referred to as gestation, typically 40 weeks in length. Counting of the weeks begins on the first day of the last menstrual period. Conceptions is assumed to occur two weeks after the first day of the last menstrual period, so for the first two weeks of a normal pregnancy, the women is not actually pregnant. Pregnancy is divided into 3 trimesters, each approximately 12 weeks in length. The terminology for the growing embryo changes from “embryo” to “fetus” at the beginning of the 11th week of gestation. The fetus is considered viable (able to survive outside the womb) at 28weeks gestation, and 50% of babies will survive if born after the 23rd week of pregnancy. Some babies born between 20 and 23 weeks gestational age do survive, but most will struggle for survival and experience life-long disability.
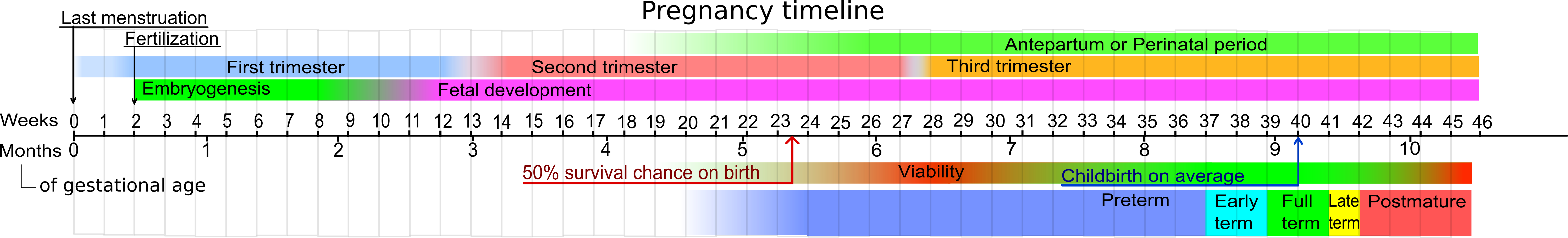
Long Description
Pregnancy Timeline
Timeline from 0 weeks to 46 weeks.
- Last menstruation is labelled at 0 weeks.
- Top layer includes Fertilization at 2 weeks and Antepartum or Perinatal period which spans week 30 to 40.
- Second layer includes First Trimester (0 to 13 weeks), Second Trimester (13 to 28 weeks) and Third Trimester (28 to 46 weeks).
- Third layer includes Embryogenisis (2 to 10 weeks) and Fetal development (10 to 46 weeks).
- Fourth layer includes “50% change on birth” at 23 to 24 weeks, Viability (24 to 31 weeks), Childbirth on average at 40 weeks.
- Bottom layer includes Preterm from 20 to 37 weeks, Early term from 37 to 39 weeks, Full term from 39 to 41 weeks, Later term from 41 to 42 weeks, and Postmature from 42 to 46 weeks.
- Fourth layer includes “50% change on birth” at 23 to 24 weeks, Viability (24 to 31 weeks), Childbirth on average at 40 weeks.
- Third layer includes Embryogenisis (2 to 10 weeks) and Fetal development (10 to 46 weeks).
- Second layer includes First Trimester (0 to 13 weeks), Second Trimester (13 to 28 weeks) and Third Trimester (28 to 46 weeks).
19.2.1 Factors that cause higher than average risk to a pregnancy include:
- age (over 35)
- lifestyle choices (smoking, drinking, drugs)
- nutritional status
- availability of prenatal care
- maternal health conditions (high blood pressure, diabetes, infection, thyroid conditions, cardio, respiratory, or vascular disorders)
- multiples (twins, triplets, etc.)
- pregnancy complications (abnormal placental condition or positioning, abnormal fetal growth, Rh incompatibility)
19.2.2 Pregnancy Body Changes
Changes occur to all body systems during pregnancy, as a woman’s body grows and provides sustenance to a growing embryo. Most women experience general fatigue and some form of gastrointestinal discomfort (morning sickness, nausea, constipation) during the early weeks of pregnancy.
Changes occur in the female body systems during pregnancy as follows:
19.2.2.1 Musculoskeletal and Neurological:
As the woman’s body changes in shape and size, the center of mass shifts anteriorly and upward. The abdomen enlarges, as do the breasts, which can be tender. The spine often becomes more lordotic in the lumbar area, which can lead to compensatory thoracic kyphosis and forward head positioning and rounded shoulders. The ribs expand inferiorly as the womb presses upward, as well as downward in the pelvic cavity. Ligamentous laxity occurs during pregnancy, especially in the third trimester, as the body prepares for delivery. It has been suggested that the laxity is due to the production of relaxin and cortisol, but some sources have refuted this assumption.1 The sacro-iliac (SI) joint is particularly vulnerable to laxity and shifting, which can lead to back pain and radiculopathy along the sciatic nerve distribution. Downward pressure from the growing fetus can cause joint movement, pressure, and pain anywhere along the kinetic chain from the spine, through the hips, knees, ankles and feet. Even the wrists can experience pain in the form of carpal tunnel syndrome because of swelling in the wrists and hands. Muscle imbalances are common during pregnancy because of postural changes. Stretching and weakening of the abdominal muscles is typical. Other muscle groups prone to stretch weakness include the lumbar extensor muscles, lower cervical extensors, scapular retractors, shoulder external rotators, and hip extensors. Muscle groups that tend to shorten and become stiff during pregnancy include the lower cervical flexors, scapular protractors, shoulder internal rotators, and hip flexors.
Diastasis recti is a longitudinal splitting of the rectus abdominis, which occurs in many pregnancies. A small split can heal without intervention following delivery, but a wide diastasis recti may require physical therapy intervention or surgery if conservative treatments fail.
19.2.2.2 Cardiovascular:
The cardiovascular system must adapt to and accommodate for the many changes that occur during gestation. Increased blood volume is necessary to supply blood to the developing fetus. The heart rate and stroke volume increase to move more blood through the increased blood vessels to the uterus and fetus. Blood pressure should NOT increase during pregnancy.
Inferior vena cava syndrome results from compression from the growing uterus on the inferior vena cava and pelvic veins. This creates more pressure in the veins in the lower extremities and can lead to dysfunction of the valves within the veins, causing varicose veins. The increased hydrostatic pressure caused by this condition often leads to peripheral edema. Many women will notice swelling in the ankles and feet. Sometimes, peripheral edema also occurs in the upper extremities, as well. It is recommended that pregnant women avoid lying supine for more than 5 minutes after the 4th month of pregnancy to lessen the effects of pressure on the inferior vena cava.
19.2.2.3 Pre-eclampsia and Eclampsia:
Preeclampsia is a pregnancy complication characterized by high blood pressure and signs of damage to another organ system, most often the liver and kidneys. Preeclampsia usually begins after 20 weeks of pregnancy in women whose blood pressure had been normal. Although poorly understood, pre-eclampsia is associated with abnormalities in the blood vessels formed to supply the placenta. The vessels are often smaller in women with pre-eclampsia, which could be associated with increased blood pressure. Other factors that are associated with the development of pre-eclampsia include genetics, and immune system deficiencies. Risk factors for developing pre-eclampsia include: maternal age (over 35, or teen-age pregnancy), first pregnancy, new paternity, history of hypertension and/or pre-eclampsia, multiple fetuses (twins, triplets), obesity, history of diabetes, migraines, lupus, or kidney disease.
- Increase in blood pressure (may be sudden or gradual)
- Excess protein in the urine
- Thrombocytopenia
- Decreased urine output
- Impaired liver function
- Shortness of breath (pulmonary edema)
- Nausea, vomiting
- Weight gain
- Edema
- Hypertension
- Pain in right upper quadrant
- Severe headaches
- Blurred vision or other visual disturbances
Negative outcomes are possible if pre-eclampsia is not corrected. These include:
- Fetal growth restriction
- Preterm birth
- Placental problems, such as placental abruption (placenta tearing away from the uterine wall prior to delivery of baby
- HELLP (hemolysis, elevated liver enzymes and low platelet count) syndrome; can be fatal for mother and baby
- Stroke
- Long-term cardiovascular conditions
- Lasting damage to the kidneys, liver, lung, heart, or eyes
- Eclampsia is a severe complication of preeclampsia. It’s a rare but serious condition where high blood pressure results in seizures during pregnancy. It can be fatal.
Treatment for pre-eclampsia is blood pressure control through medication and lifestyle choices. Scheduled or pre-term delivery of the baby may be necessary if the condition appears to be progressing to eclampsia. In the case of eclampsia, the only option is to deliver the baby, no matter how early in the pregnancy it occurs. Most women do not experience long-term effects from preeclampsia.
19.2.2.3 Pulmonary:
Progesterone causes stimulation of the respiratory center, which can lead to hyperventilation and respiratory alkalosis. Chronic respiratory alkalosis is a common finding in pregnant women. Also, as the pregnancy progresses, the uterus presses upward on internal organs. The digestive organs can be pushed up into the thoracic cavity, stretching the diaphragm and decreasing the functional reserve capacity of the lungs and total lung capacity. Many women with experience shortness of breath with exertion later in the pregnancy.
Pregnancy increases the risk of pulmonary edema due to the increase in plasma volume in the blood and the increased cardiac output in the second trimester.
19.2.2.4 Urinary:
19.2.2.5 Digestive:
- obesity
- lack of exercise
- previous gestational diabetes
- polycystic ovarian syndrome
- family history of diabetes
- previous delivery of a large baby (>9 lbs)
- race — Women who are Black, Hispanic, American Indian and Asian American have a higher risk of developing gestational diabetes
Gestational diabetes can lead to complications for both mother any baby. These include:
- preterm birth
- extreme birth weight
- respiratory distress syndrome in the baby
- hypoglycemia in the baby
- increased risk for obesity and development of type 2 diabetes in the baby later in life
- stillbirth
- C-section
- increased risk for pre-eclampsia in the mother
- increased risk for the development of type 2 diabetes after pregnancy is over
Gestational diabetes can often be managed through diet and exercise. When necessary, medications can be used to treat the condition. Most women who experience gestational diabetes and receive appropriate intervention deliver normal babies and have no residual effects.
19.2.2.6 Psychological and Emotional:
Most women experience some emotional changes during pregnancy. The many changes in hormones, body shape and size, increased levels of responsibility, and anticipated changes in lifestyle can lead to feelings of anxiousness and depression. Post-partum depression is a poorly understood condition. It is recognized as a condition that requires attention. Recently, experts have started referring to the 12 weeks after deliver as the “fourth trimester.” This period includes physical and psychological adjustments as mother and baby develop a new relationship. Some references have noted that issues previously associated with the period of time after the birth of the baby (postpartum depression) can actually begin in the third trimester. Postpartum depression can be diagnoses up to a year after the birth of a baby. Paternal postpartum depression is also recognized in new fathers who are experiencing new emotions and fears with their new role in family life. Health care providers need to be aware of the signs and symptoms of psychological stress in a pregnant or recently delivered mother or father.
Postpartum depression signs and symptoms may include:
- Depressed mood or severe mood swings
- Excessive crying
- Difficulty bonding with your baby
- Withdrawing from family and friends
- Loss of appetite or eating much more than usual
- Inability to sleep (insomnia) or sleeping too much
- Overwhelming fatigue or loss of energy
- Reduced interest and pleasure in activities you used to enjoy
- Intense irritability and anger
- Fear that you’re not a good mother
- Hopelessness
- Feelings of worthlessness, shame, guilt or inadequacy
- Diminished ability to think clearly, concentrate or make decisions
- Restlessness
- Severe anxiety and panic attacks
- Thoughts of harming yourself or your baby
- Recurrent thoughts of death or suicide
Rarely, postpartum depression can lead to postpartum psychosis. This condition generally develops within the first week following delivery. Signs and symptoms include: confusion and disorientation, compulsive or paranoid thoughts, hallucinations, delusions, excessive energy and agitation, and attempts to harm self or baby. The signs and symptoms can be quite severe, and prompt medical and psychological attention is warranted.
19.2.3 Physical Therapy and Pregnancy
Many of the issues associated with pregnancy can be addressed by physical therapy. Many physical therapy exercise interventions are helpful prior to, during, and after pregnancy. For musculoskeletal issues, including postural deviation, muscle imbalance, and pain, many tools are available to PTs and PTAs. Postural awareness training, range of motion exercises, and muscle strengthening exercises are commonly used. Abdominal muscles and pelvic floor muscles in particular are often targeted areas for strengthening. Patients can also benefit from a brace or support to help lift the abdomen and align the spine. Sometimes orthotics can be helpful for women who experience foot and lower extremity pain. Cardiovascular exercise is helpful in to maintain adequate heart, vascular and lung function during pregnancy. Aquatic therapy can be very useful in treating pregnant patients. The buoyancy of the water helps relive effects of gravity on the pregnant belly and the overall hydrostatic pressure exerted by the water helps with venous return and helps decrease peripheral edema.
Women who have undergone and Caesarian section may need additional time to heal and can benefit from a gradual abdominal exercise program to help heal the abdominal area. In addition, scar massage and in some cases, wound care could be used to help with the surgical wound.
Many modalities used in physical therapy are contraindicated for patients who are pregnant. These include heat modalities, such as ultrasound, diathermy and moist heat, electrical stimulation, and traction. Ice is generally considered safe for pregnant women.
19.2.4 Exercise During Pregnancy
In general, exercise during pregnancy is encouraged. Women should be able to maintain an active lifestyle and continue exercising at pre-pregnancy levels, with a few exceptions. Women with any of the risk factors listed above should be fully evaluated for exercise risk and only exercise to a level prescribed by a physical therapist. Any activity that puts the pregnant woman at risk for falls or abdominal injury should be avoided. Some activities that might fall into these categories include: horseback riding, downhill skiiing, and contact sports such as soccer and hockey.
19.3 Male Reproductive System
The male reproductive system includes structures as shown below. The position of the prostate gland is particularly notable, as many urinary problems in males are related to prostate conditions.

Long Description
The Male Reproductive System
An illustration with the following labels:
- bladder
- pubic bone
- suspensory ligament of penis
- puboprostatic ligament
- perineal membrane
- external urethral sphincter
- penis
- corpus cavernosum
- glans penis
- foreskin
- urethral opening
- sigmoid colon
- rectum
- seminal vesicle
- ejaculatory duct
- prostate gland
- Cowper’s gland
- anus
- vas deferens
- epididymis
- testis
- scrotum
As in females, conditions associated with the male reproductive system can be caused by a variety of reasons.
19.3.1 Genetics:
If there are 2 X chromosomes (XXY instead of XY) in a male, a diagnosis of Kleinfelter syndrome is made. Low testosterone production and reduced muscle mass, facial hair, and body hair are common signs. Most males with this condition produce little or no sperm. Treatment for Kleinfelter syndrome includes testosterone supplements and fertility counselling and intervention.
19.3.2 Cancer:
One of the most common forms of cancer in men is prostate cancer. The prostate can become enlarged, leading to problems such as difficulty urinating and erectile dysfunction. Other signs and symptoms of advanced stages of prostate cancer may include: blood in the urine or semen, bone pain, and unintentional weight loss. Many forms of prostate cancer are very slow to grow and cause few long-term effects. Some are more aggressive, growing quickly and metastasizing in other organs. Early detection is helpful in determining prognosis and treatment plan. Risk factors for prostate cancer include: age, race, family history, and obesity. Men’s risk factor increase as they age. For unknown reasons, black men have a greater risk for developing prostate cancer, and they have a higher likelihood of developing more aggressive forms of prostate cancer. Family history is important, especially if a parent, sibling, or child has been diagnosed with prostate cancer. Families that carry known breast cancer genes (BRCA1 or BRCA2) or a very strong family history of breast cancer also have a higher risk for prostate cancer in men. Digital rectal examination and prostate specific antigen testing are used as screening tools for prostate abnormality. Ultrasound, MRI, and biopsy are used to help determine the presence and type of cancer. Surgical removal of the prostate is sometimes recommended in the case of prostate cancer. Sometimes, a wait-and-see approach is utilized if the cancer is not particularly aggressive.
Testicular cancer is much less common than prostate cancer, and it occurs most often in men aged 15-35. Other risk factors include: undescended testicle, testicular abnormality, such as in Kleinfelter syndrome, positive family history, and race (more common in white men than black men). Signs and symptoms include a lump found in either testicle, heaviness in the scrotum, pain or discomfort in the scrotum or testicle, dull ache in the groin or abdomen, enlargement or tenderness of the breasts, and back pain. Diagnosis of testicular cancer can be made through self-exam with ultrasound and blood work for confirmation. Surgery may be necessary to determine type of cancer, and surgical removal of the involved testicle is often recommended. Testicular cancer is highly treatable even in advanced stages.
The top causes of death among adult men in the U.S. are heart disease, cancer, unintentional injuries, chronic lower respiratory disease and stroke, according to the Centers for Disease Control and Prevention. Healthy lifestyles including a diet rich in vegetables, regular exercise routines, limits on alcohol consumption, regular and adequate sleep habits, maintenance of healthy weight, avoidance of smoking and tobacco products, and limiting stress are recommended for all men. Motor vehicle accidents and suicide are included in the top 10 list for causes of death for men, and in the top 5 for young men.2 Attention to motor vehicle safety, especially avoiding driving while intoxicated is an area for continued vigilance. Suicidal behaviors, depression, and post-traumatic stress should be addressed by a qualified mental health professional. PTAs should encourage men to seek professional help if these conditions are suspected.
19.3.3 Erectile Dysfunction (ED):
Erectile dysfunction (inability to maintain an erection) is a common problem in men. The condition is believed to be caused by damage to the endothelial lining of the blood vessels supplying the penis. This damage is associated with other conditions which cause damage to blood vessels including: hypertension, diabetes, tobacco use, alcohol use, high serum cholesterol, obesity, low testosterone level, and advancing age. ED is known to be related to cardiovascular disease, as the damage to the inner layer of the blood vessels is problematic throughout the body, but might be first noticeable in erectile dysfunction. Men with ED should be checked and for the cause of the the problem.
Genital and Reproductive Systems Resources
Images:
19.1
a The Female Reproductive System “The Female Reproductive System” by Bruce Blaus is licensed under CC BY 3.0 – – Own work]
19.2
b Pregnancy Timeline. “Pregnancy Timeline” by Mikael Häggström is licensed under CC BY 1.0
19.3
c Male Anatomy “Male Anatomy” is licensed under CC BY 3.0
Resources:
CDC National Center for Health Statistics – 2018
American College of Obstetritians and Gynecologists
Mayo Clinic – Gestational Diabetes
Mayo Clinic – Postpartum Depression

