Chapter 15: Genetic and Developmental Conditions
Learning Objectives
After completing this chapter, the learner should be able to:
- Define the basic terminology associated with genetic and developmental conditions..
- Differentiate between congenital, genetic, chromosomal, developmental, and multifactoral conditions.
- Discuss inheritance patterns associated with genetic conditions.
- Identify risk factors, etiologic factors, pathogenesis, clinical manifestations, diagnosis and medical management for selected genetic and developmental disorders, including:
- Cystic fibrosis
- Marfan syndrome
- Muscular dystrophy
- Fragile X Syndrome
- Down Syndrome
- Cerebral palsy
- Spina Bifida
- Fetal Alcohol Syndrome
- Mitochondrial Disorders
Chapter Contents
- 15.1 Genetic and Developmental Conditions: Basic Terminology and Concepts
- 15.2 Genetic Disorders
- 15.3 Dominant Traits
- 15.4 Recessive Traits
- 15.5 X-linked Traits
- 15.6 Marfan Syndrome
- 15.7 Cystic fibrosis
- 15.8 Duchene Muscular Dystrophy
- 15.9 Fragile X syndrome
- 15.10 Down Syndrome
- 15.11 Cerebral Palsy
- 15.12 Spina Bifida (Myelomeningeocele)
- 15.13 Fetal Alcohol Syndrome
- 15.14 Mitochondrial Disorders
15.1 Genetic and Developmental Conditions: Basic Terminology and Concepts
Genetic and developmental conditions is a huge topic area. This chapter attempts to discuss basic concepts and a few disorders most likely to be seen by physical therapist assistants in the clinic. Some general terminology is a good place to start.
Genes: A gene is the basic physical and functional unit of heredity. Genes are made up of DNA. Some genes act as instructions to make molecules called proteins. However, many genes do not code for proteins. Instead, they might provide sites for proteins to bind or provide instructions for turning on or off certain mechanisms.
Genes are made up of DNA. Each chromosome contains many genes.
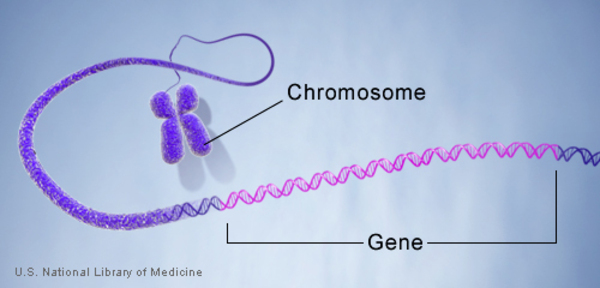
Alleles: forms of the same gene with small differences in their sequence of DNA bases. These small differences contribute to each person’s unique physical features.Chromosomes:
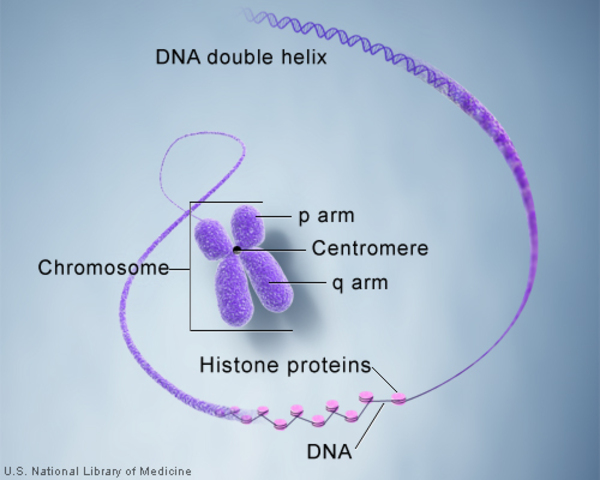
Chromosome: a is a threadlike structure houses in the nucleus of a livingbcell. Chromosomes are made up of DNA tightly coiled many times around proteins called histones that support its structure.
DNA and histone proteins are packaged into structures called chromosomes.
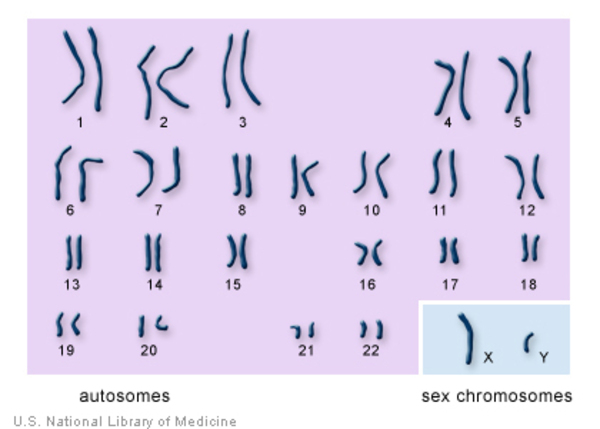
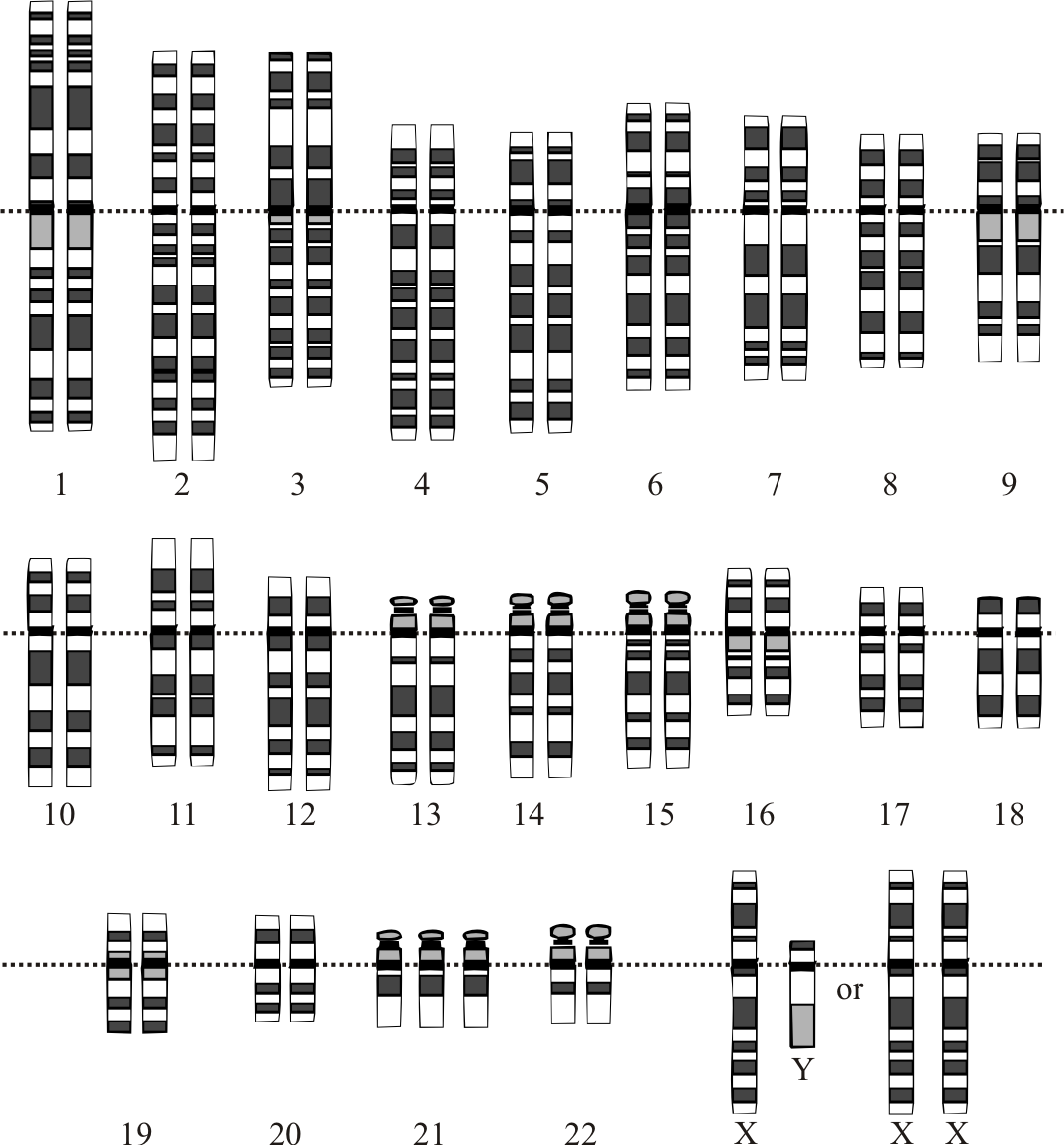
The typical number of chromosomes in humans is 23 pairs, or 46 all together. One pair of chromosomes , the 23rd pair, determines sex. If there are 2 X chromosomes in the 23rd position, the individual is female; if there is one X and one Y chromosome, the individual is male.
The 22 autosomes are numbered by size. The other two chromosomes, X and Y, are the sex chromosomes. This picture of the human chromosomes lined up in pairs is called a karyotype.
Genetic: having to do with the genes; hereditary
There are three types of genetic disorders:
- Single-gene disorders, where a mutation affects one gene. Sickle cell anemia and cystic fibrosis are examples.
- Chromosomal disorders, where chromosomes (or parts of chromosomes) are missing or changed in number or configuration. Chromosomes are the structures that hold our genes. Down syndrome is a chromosomal disorder.
- Complex disorders/ multifactoral disorders, where there are mutations in two or more genes. Often, lifestyle and environment also play a role in allowing the genetic condition to occur. Many forms of cancer fall into this cancer. Some types of cerebral palsy are also in this category.
Source: Retrieved from NIH Library
Most genetic and chromosomal conditions can be diagnosed through a blood test that identifies abnormalities in the genes or chromosomes. General signs and symptoms are also useful in diagnosing these kinds of conditions.
Congenital: present at birth or occurring very soon after birth; can also include genetic, but not the same as genetic; congenital conditions can be caused by birth injuries, maternal conditions, or developmental problems in utero. Spina bifida, cerebral palsy, fetal alcohol syndrome, and many heart conditions are examples of congenital conditions.
Full-term pregnancy: A pregnancy is now considered “full term” at 39 weeks. Any birth occurring before 37 weeks of pregnancy is considered “pre-term.”
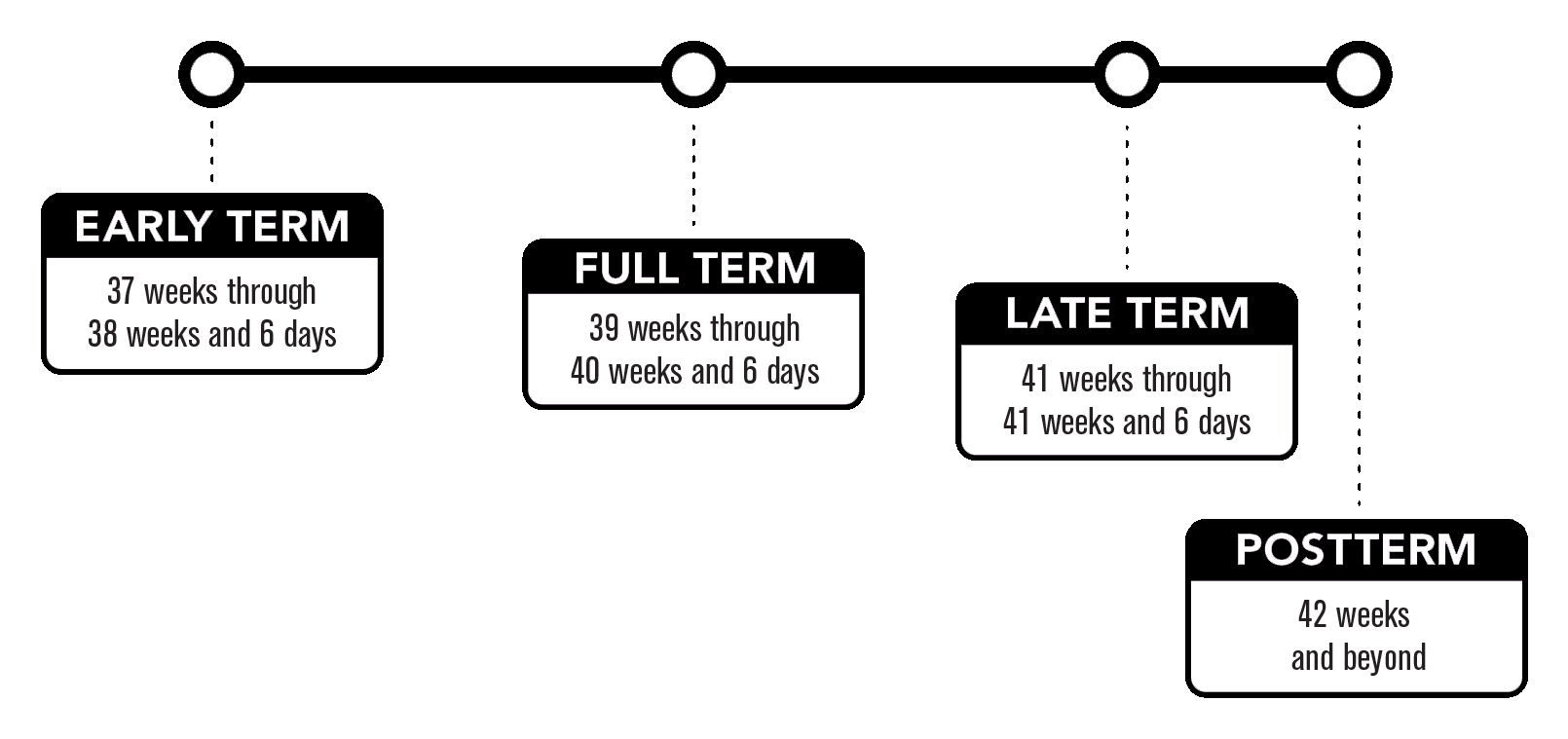
Pre-term births present higher risk for many complications and conditions. Because lung development occurs late in the pregnancy, many babies born early have difficulty breathing and could need ventilatory assistance. Heart defects are also common in pre-term babies, many of which are mild, but some can be severe. Other risk associated with pre-term delivery include cerebral palsy, learning disabilities, attention disorders, stroke, eating disorders (suck and swallow difficulties), failure to thrive conditions, poor body temperature regulation, and abnormal muscle tone.
If babies are born post-term (after 42 weeks), their risk of complications, disability, and other problems is also increased.
15.2 Genetic Disorders
Single-Gene Disorders
Single-gene disorders can be sub-categorized into autosomal dominant, autosomal-recessive, X-linked dominant and X-linked recessive.
15.3 Dominant
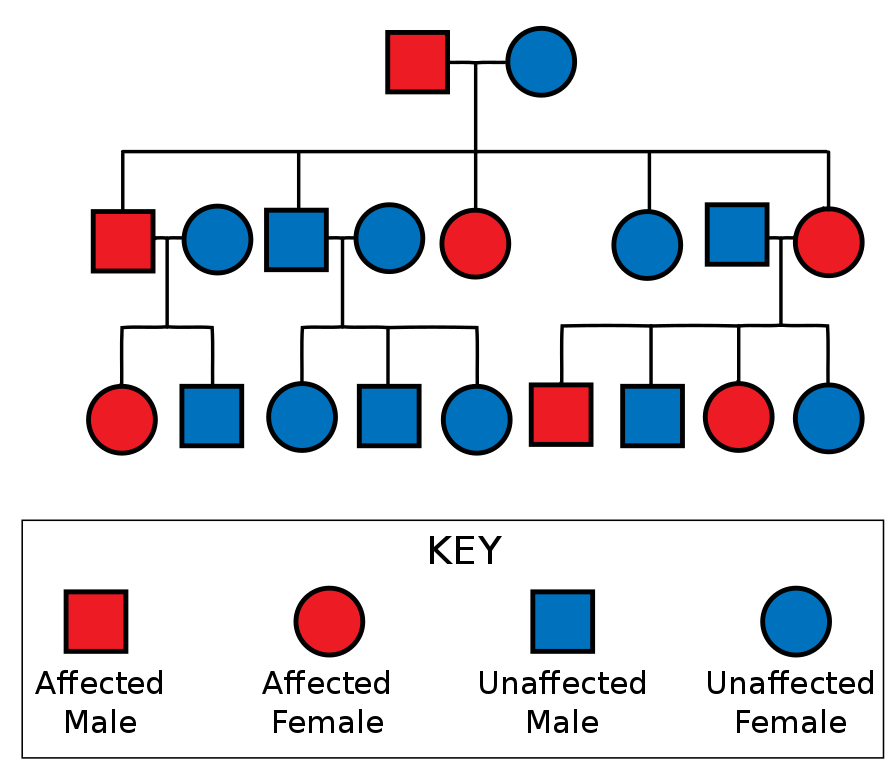
Autosomal dominant disorders require only one abnormal gene in the allele pair in order for the offspring to be affected by the genetic condition. Usually one parent actually has the disorder in dominant inheritance patterns, although the disorder might not be evident in the adult until after the offspring is born. The autosomal pattern of inheritance can be observed in the following diagram. So, if either mother or father possesses the gene for a disorder such as Huntington disease, neurofibromatosis, Marfan’s syndrome, polycystic kidney disease, and most cases of osteogenesis imperfecta, each child has a 50% chance of having the disease. Each child also has a 50% chance of not having the disease, as well. No carrier state exists in an autosomal dominant pattern of inheritance.
Source: Huntingdon’w disease
15.4 Recessive
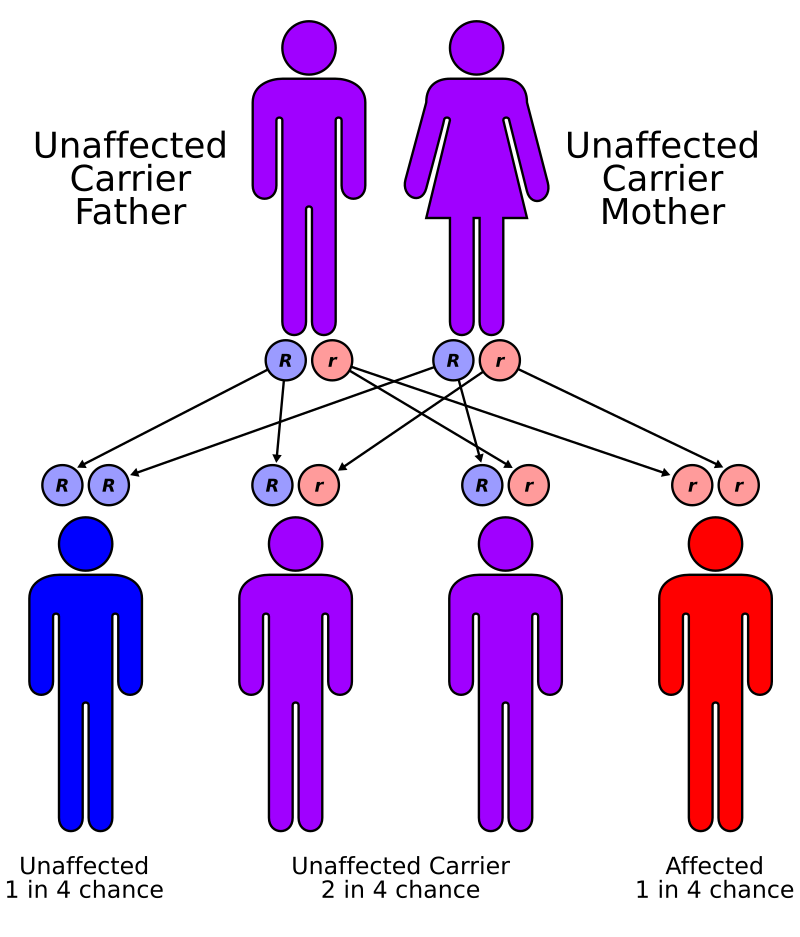
In autosomal recessive disorders, both parents must possess the abnormal gene in order for a child to have the disease or disorder. Each child has a 25% chance of expressing the gene (having the disorder), each has a 50% of being a carrier of the abnormal gene, and each has a 25% chance of being free of the abnormal gene. The diagram below shows a recessive inheritance pattern.
Long Description
Autorecessive
Illustration with human stick figures labelled and connected by arrows. 2 parents are shown: an unaffected carrier father and mother. Below each is a blue R and a red R. Below the parents are 4 children. Child 1 is labelled “Unaffected, 1 in 4 chance” and has 2 blue R’s, 1 from dad and 1 from mom. Child 2 is labelled “Unaffected carrier: 2 in 4 chance” and has 1 blue R from dad and 1 red r from mom. Child 3 is also labelled “Unaffected carrier: 2 in 4 chance” and has has 1 blue R from mom and 1 red r from dad. Child 4 is labelled “Affected: 1 in 4 chance” and has 2 red R’s, 1 from dad and 1 from mom.
If only one parent possess an abnormal recessive gene, each child has a 50% chance of being a carrier of the gene, but no child will express the gene (have the disorder).
15.5 X-Linked
The X chromosome supplied by the mother can carry abnormal genes, as occurs in conditions including Fragile X syndrome and Duchene’s muscular dystrophy. If the mother is a carrier for one of these disorders, each son will have a 50% chance of inheriting the disorder, and each daughter will have a 50% chance of inheriting the carrier state. Since this is a recessive gene, daughters will have have a normal copy from the father, which is dominant. Boys will receive a Y chromosome from the father, so they will only have one X chromosome. If it is the abnormal one, they will show the effects of that gene. In the case of a genetic disorder, they will have the disorder. Boys can not be carriers of X-linked genetic disorders. The inheritance pattern of X-linked disorders is shown below.
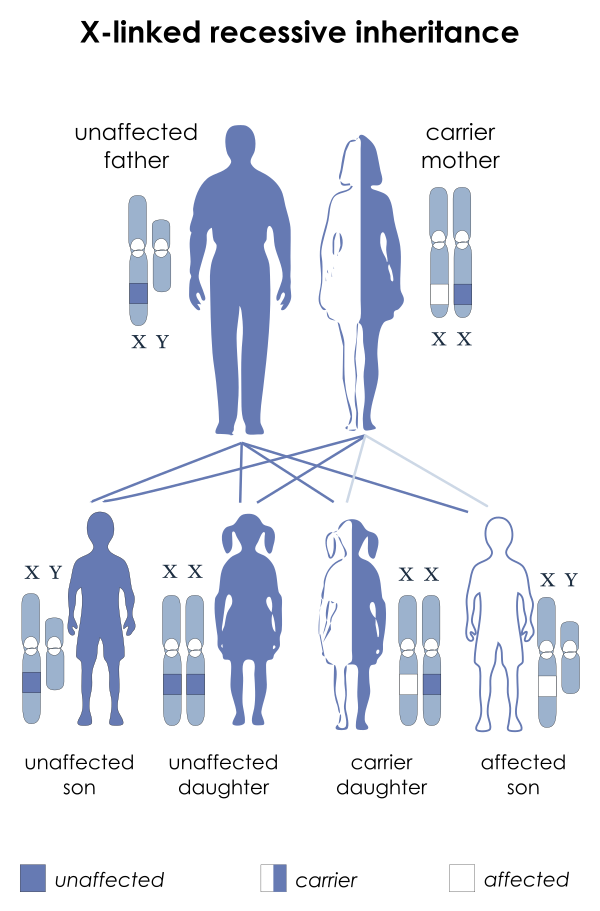
Long Description
Title X-linked recessive inheritance
An illustration shows an unaffected father (entirely blue) and a carrier mother (half blue and half white). Below them are 2 sons and 2 daughters. One son and one daughter are unaffected (entirely blue). They are connected to their parents by 2 blue lines each. One daughter is a carrier (half blue and half white). She is connected to the parents by 1 blue line (father) and 1 white line (mother). The other son is affected (entirely white). He is also connected to his parents by 1 blue line (father) and 1 white line (mother).
Source: Muscular dystrophy
X-linked dominant pattern disorders do exist, but they are very rare and will not be covered in this text.
15.6 Marfan Syndrome – Dominant
Marfan syndrome is caused by an abnormal gene on chromosome 15. Since it is an autosomal dominant trait, only one copy of the abnormal gene is necessary for the disorder to be expressed in the individual. So, only one parent has to carry the Marfan gene in order for a child to have Marfan syndrome. Sometimes, a spontaneous mutation of the gene causes Marfan syndrome. Marfan syndrome may not be noticeable at birth and might not be diagnosed until much later in life.
When the abnormal gene for Marfan syndrome is present, the coding for formation of connective tissue is affected. Connective tissue is less elastic and more fragile in people with Marfan syndrome than in those without. Since connective tissue is everywhere in the body, the effects can be widespread. Also, the messaging system to turn off growth in the long bones is turned off, so the individual tends to be very tall, with long arms, legs, fingers, and toes. Scoliosis and abnormal formations of the rib cage are also common in people with Marfan syndrome.
The most serious effects of Marfan syndrome are in the aorta. Because of weak connective tissue in the walls of the aorta, it is prone to aneurysm and rupture. These can be fatal occurrences and can happen without warning to a seemingly healthy individual. Other problems that can develop include bulla and pneumothorax in the lungs, detached retina or dislocated lens in the eye, mitral valve prolapse in the heart.
Although there is no cure for Marfan syndrome, many of the effects can be corrected or controlled. Surgery can correct most aortic and heart problems. Some drugs (beta blockers and angiotensin receptor blockers) can help slow the dilation of the aorta, as well. Retinal and lens problems in the eye can be corrected with surgery.
A good video on Marfan syndrome.
“Marfan Syndrome – causes, symptoms, diagnosis, treatment, pathology” by Osmosis
15.7 Cystic Fibrosis – Recessive
Cystic fibrosis is a common genetic disease within the white population in the United States. The disease occurs in 1 in 2,500 to 3,500 white newborns. Cystic fibrosis is less common in other ethnic groups, affecting about 1 in 17,000 African Americans and 1 in 31,000 Asian Americans.(Source). The disorder is caused by a mutation on chromosome 7 that both parents must carry in order for their children to be affected. Since it is a recessive trait, if both parents are carriers, each child has a 25% chance of having the condition, a 50% chance of being a carrier, and a 25% chance of neither being a carrier or having the disorder.
Cystic fibrosis is a disease that causes mucous to be thick and sticky. The effects are most serious in the lungs, but the digestive system and reproductive system also can be affected. This disorder was discussed in the Respiratory System chapter. For a quick review, this video is available.
“Cystic fibrosis – causes, symptoms, diagnosis, treatment, pathology” by Osmosis
15.8 Duchenne Muscular Dystrophy: X-linked
Duchenne muscular dystrophy is the most common type of muscular dystrophy. The many types of muscular distrophy occur in various inheritance patterns, but Duchenne muscular dystrophy (DMD) is carried on the X chromosome. It is carried by mothers and passed on to sons in the form of the disorder. Daughters may be carries. Each son has a 50% chance of having the disorder and each daughter has a 50% chance of being a carrier. Spontaneous mutations do occur, which can cause DMD, and some women have only some eggs affected with the defective dystrophin gene, so the inheritance pattern can be complicated.
DMD causes a lack of functional dystrophin, which is a protein found mainly in skeletal and cardiac muscle tissue. Without dystrophin, muscle tissue is easily damaged, causing inflammation. The overall effect of the dystrophin deficiency is muscle weakness.
Boys usually begin to show signs of muscle weakness between 1 and 6 years of age. The disease progresses affecting gait (waddling gait) and other functional activities. Standing up from the floor becomes difficult, and the child will demonstrate a positive “Gower’s sign,” walking his hands up his thighs in order to stand upright. Another indication of DMD is pseudohypertrophy of the calf muscles. The gastrocnemius and soleus muscles become enlarged as muscle tissue is replaced by fat and connective tissue, increasing calf girth. In time, joint contractures and scoliosis can develop as a result of immobility and positioning problems. By early teenage years, most boys are using a wheelchair most of the time. Death due to respiratory failure or heart failure usually occurs between the ages of 16 and 35 in most individuals with DMD.
Physical therapy can be helpful for people with DMD to help maintain mobility. Bed rest and immobility are harmful, as they can accelerate the muscle loss, joint contractures, and cardiorespiratory problems. PT generally includes ROM, gentle exercise to maintain strength, cardiovascular activity to tolerance, and breathing technique training. Orthotics or other lower extremity or trunk bracing maybe useful as posture and mobility become problematic. Assistive device and wheelchair training are important aspects of physical therapy services. Family members and caregivers can also benefit from instruction on transfer techniques, positioning, and general mobility expectations and assistance for the patient.
Medical diagnosis is initiated through medical examination of signs and symptoms and confirmed through muscle biopsy and genetic testing. Medical treatment for DMD revolves mainly around glucocorticoid (prednisone) therapy. Exon skipping therapy is a new pharmaceutical therapy that is being studied and is showing some promising results.
“Duchenne Muscular Dystrophy and Dystrophin” , Medicurio is licensed under CC
Source: youtube.com/watch?v=Ebu8W8Osuxk
Source: youtube.com/watch?v=DGOmN6rnsNk
“Duchenne & Becker muscular dystrophy – causes, symptoms, treatment & pathology” by Osmosis is licensed under CC
15.9 Fragile X Syndrome: X-linked
This video provides a good overview of the genetic differences in Fragile X syndrome.
Source: CDC Fragile X Syndrome
Fragile X syndrome results from an abnormality in the X chromosome in which the FMR-1 gene produces too little of the protein, FMRP, resulting in a number of different symptoms, most notably cognitive functioning delays and abnormalities. Both males and females can be affected by fragile x syndrome, but because they have two X chromosomes and only one may be affected, females tend to show milder symptoms. Family traits such as tremors and early menopause are symptoms of disorders that can be related to fragile X syndrome. If these traits exist in a family, offspring are at a greater than average risk for developing fragile X syndrome.
Children are usually diagnosed with fragile X syndrome around the age of 3 years. Conditions associated with fragile X syndrome include: learning disabilities, hyperactivity, attention problems, developmental delays, and seizures. Children with fragile X syndrome also have a higher risk of a diagnosis of autism spectrum disorder. Some people with fragile X syndrome have physical features, such as large ears, but not all do.
Treatment and intervention for children and adults with fragile X syndrome depends upon the severity of the condition. Early intervention in speech and language therapy, physical and occupational therapy, and specialized preschool experiences can help improve a young child’s readiness for education at school age. Many children with fragile X syndrome are able to participate in regular education; some require special education services. Behavior treatments and some medications are also useful in the treatment of fragile X syndrome. The disorder is non-progressive, that is, it does not get worse over time. People with fragile X syndrome do not have a shortened life expectancy. Behavioral issues can become more problematic at different times over the lifespan. There is no cure for fragile X syndrome, and the severity of the condition is quite variable. Some behavioral problems such as anxiety, compulsive/perseverative and mood symptoms can be managed with antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs). Some commonly prescribed SSRIs include:
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Paroxetine (Paxil, Pexeva)
- Sertraline (Zoloft)
Physical therapy can be useful in a team approach to managing fragile X syndrome, especially in young children. Developmental delays are common in the condition, and children may be quite delayed in the development of their gross motor milestones, such as crawling and walking. Higher-level coordinated activities, such as jumping, ball skills, and sporting activities can be particularly challenging. Physical therapy can help improve muscle strength and balance and coordination to help children with fragile X syndrome develop gross motor skills to be able to participate in activities with their peers.
15.10 Down Syndrome: Chromosomal Number Disorder
Although there are several different chromosomal abnormalities that can cause different types of Down syndrome (DS), the most common type involves an extra chromosome in the 21st position in a phenotype, so it is named, “trisomy 21.” For the purposes of this text, trisomy 21 and DS will be used interchangeably, and discussion will be limited to that type of Down syndrome.
The alterations in chromsome number result in some or all of the following characteristics: diminished cognitive ability, stunted growth, umbillical hernia, speech and language problems, ligamentous laxity, flatened nasal bridge, slanted eyes, flat head, separation between first and second toes, abnormal teeth, obstructive sleep apnea, and congenital heart disease.
People with DS are also at higher risk for the development of leukemia and Alzheimer disease. Obesity and diabetes are also more common in people with DS. The expected lifespan of people with DS has increased dramatically, from and average of 9 years in 1929 to 60 years or more today. (Zhu J, Hasle H, Correa A, Schendel D, Friedmant J, Olsen J, Ramussen S. Survival among people with Down syndrome: a nationwide population-based study in Denmark. Genetics in Medicine 2013;15:64-69. (accessed Feb 18, 2020))
DS is diagnosed through clinical presentation and genetic study. There is no specific treatment for DS and it is a life-long non-degenerative condition. If congenital cardiac anomalies are present, they are often correct early in life. Interventions including physical therapy, occupational therapy, and speech therapy are usually instituted early, as well, to help with the anticipated developmental delays.
Physical therapy interventions include muscle strengthening, facilitation of movement, gait training, balance and coordination activities, and sometimes orthotic application and assistive device training. Physical therapy can occur on land or in a pool and can include a variety of child-centered activities. Most children with Down Syndrome are ambulatory and are able to participate in many recreational activities. There is a concern regarding a prevalence toward instability between vertebral segments C1 and C2, so children should be screened before participating in sports where physical contact or falling is likely, such as horseback riding, football, or gymnastics.
The transition between childhood and adulthood can be difficult for someone with DS. The number of services available to adults with DS is lower than are available to children. Also, knowledge of services, transportation to and from services, and assistance in maintaining attendance can all be barriers to employment. Even access to exercise is difficult for adults with DS, as social stigma and cost can be problems in a typical recreational or “work-out” facility, and there are very few settings that are comfortable and accommodating to people with disabilities. It is important for people with DS to maintain an exercise regime, as they are prone to obesity. Most people with DS lead sedentary lives, and this only compounds the problem. Regular daily exercise should be a goal for every person with DS.
For a great lesson on Down syndrome from kids with Down syndrome, watch “In Their Words” at the following site: In Their Words Fantastic!
For a more serious explanation, check out the Osmosis video.
Source: YouTube
“Down syndrome (trisomy 21) – causes, symptoms, diagnosis, & pathology” by Osmosis is licensed under CC
15.11 Cerebral Palsy: Developmental Disorder
Cerebral palsy (CP) is actually a group of disorders. There are several definitions of CP, but all include the following important components.
- Etiology: CP results from an injury, lesion or malformation in the brain that occurs before, during, or soon after a baby’s birth.
- Non-progressive damage: The area of damage remains unchanged and is permanent. That is, the disorder is non-progressive. Functional abilities can improve, and changes in motor skills can occur, but the actual area of brain damage remains the same.
- Motor function: The impairments include problems with motor function. Other impairments may also exist, but impaired motor function is always part of CP.
For a good introduction to cerebral palsy, watch the videos below.
Source: youtube.com/watch?v=7fUGWKM32hE
“Cerebral Palsy – (DETAILED) Overview” by Armando Hasudungan is licensed under CC
Source: YouTube
“Cerebral palsy (CP) – causes, symptoms, diagnosis, treatment & pathology” by Osmosis is licensed under CC
There are many possible causes and risk factors for CP. They include:
- preterm birth (most prevalent risk factor; the earlier the baby, the higher the risk)
- low birth weight
- anoxia in fetus / baby (prenatal, during birth, or just after birth)
- fetal or neonatal stroke/ intracranial hemorrhage
- intrauterine infection
- postnatal infection in infant (especially meningitis and encephalitis)
- maternal event (eclampsia, toxemia)
- maternal seizure
- lack of prenatal care (maternal ill health, drug use, smoking, etc.)
- genetics
As shown in the video, there are three main types of cerebral palsy, each associated with different areas of brain damage. The first and most common type of CP is Spastic CP, which is associated with damage to the cerebral cortex. The next type is Dyskinetic CP, which is associated with damage to the basal ganglia. The third type is Ataxic CP, which is associated with damage to the cerebellum. Each type can include involvement from very mild to very severe. Some children will experience minimal disability due to CP, while others will require special educational arrangements and lifelong care and healthcare services. Most children with CP experience delays in motor milestone achievement, so it is important that physical therapists and physical therapists assistants understand and appreciate typical gross and fine motor skill acquisition.
Another important categorization scheme for CP is by area of involvement. If all 4 limbs are involved, the term is quadriplegia, three limbs is triplegia, 2 limbs (LEs) is diplegia or paraplegia, and one limb is monoplegia. If either just the right or left side is involved, hemiplegia is the term applied.
Children and adults with CP by definition must have motor involvement, but other kinds of disability often accompany a CP diagnosis. Impairments in cognition, vision, hearing, speech, feeding, and mood are not uncommon in people with CP. The risk for experiencing seizures is higher in individuals with CP. Orthopedic concerns, such as spinal scoliosis and hip dysplasia are also common.
Spastic CP (Pyramidal CP)
Spastic CP affects the voluntary muscle control by causing increased muscle tone. The area of damage in spastic CP is the motor cortex (cerebral cortex) of the brain. The tone can be affected in any muscles, but the most common areas of spasticity include the hip flexors and adductors, knee flexors, and ankle plantar flexors in the lower extremities and the shoulder adductors, and elbow, wrist and hand flexors in the upper extremities.
Children with spastic CP generally show decreased ranges of motion in the affected limb(s) and have limited options on patterns of movement. If they are ambulatory, they often walk with a scissors gait (thighs and knees together, feet sometimes crossing) because of short hip adductor muscles, and an equinus gait (walking on toes) because of short plantar flexors in the ankle. Their range of motion is limited in affected areas and they are likely to develop muscle contractures.
Dyskinetic CP (Athetoid CP)
Dyskinetic CP is marked by atypical movement patterns, such as dystonia, chorea, and athetosis. Dystonia refers to involuntary movements leading to sustained positions and unusual postures. Chorea is a series of irregular, nonpurposeful, uncontrolled movements that can occur in a limb or throughout an entire body. Athetosis refers to slow, writhing movements that are often repetitive or rhythmic. This type of CP used to be called Athetoid CP because of these characteristic motions. The muscle tone varies from low to high in an individual with dyskinetic CP, and the lack of motor control is evident in all movements. The area of damage in this type of CP is the basal ganglia, and the movements of people with dyskinetic CP look similar to the movement patterns seen in Parkinson disease or Huntington disease, which also effect the basal ganglia.
Ataxic CP
The third type of CP is Ataxic CP. The cerebellum is the area of involvement in this type of CP. The muscle tone tends to be decreased (hyptonic) in ataxic CP. Characteristics of ataxic CP include coordination disorders and balance problems. Children and adults with ataxic CP usually learn to walk, but often do so with a wide base of support and heavy footfall. They have difficulty with more complex skills requiring higher levels of coordination, such as jumping, balancing on one foot, and karaoke (grapevine) stepping.
Mixed-Type CP
Some children exhibit characteristics from more than one of the categories listed above. They are often diagnosed with mixed-type CP.
CP is diagnosed through clinical presentation and can sometimes be confirmed with an MRI of the brain. The causative factors of the damage need to be addressed immediately, but once the brain damage has occurred, there is no treatment for the actual damage. There are many interventions available to help improve the lives of children and adults who have CP, however. Physical therapy, occupational therapy, and speech/language therapy should be initiated as soon as possible to observe developmental milestones, provide frequent therapeutic interventions, and provide caregivers with activities to help children progress in their development. Adaptive seating, bracing and orthotics, assistive device training, wheelchair selection and training, and adaptive assistance for home and school are included in the therapeutic team’s work with the patient. Pharmacological interventions can include muscle relaxants for spasticity, pain reducing medications, anti-seizure medications, and sleep aids. surgical interventions can include orthopedic surgeries for scoliosis and hip dysplasia. For spasticity, short, spastic muscles can be surgically stretched and lengthened. Specific nerves can be cut in selected dorsal rhizotomies in order to decrease spasticity in certain muscles. Botox injections can help decrease spasticity, or an intrathecal pump can be inserted in to help relax spastic muscles through the delivery of medications, such as baclofen. The following website has more information on botox injections and baclofen pumps. Botox injections and baclafen pumps.
Information on selected dorsal rhizotomy can be found at the Cleveland Clinic website.
15.12 Spina Bifida (Myelomeningocele): Developmental Disorder
Watch the video below to learn about spina bifida.
source: youtube.com/watch?v=jlDZA2PNW2o
“Spina bifida (myelomeningocele, meningocele, occulta) – causes, symptoms, treatment” by Osmosis is licensed under CC
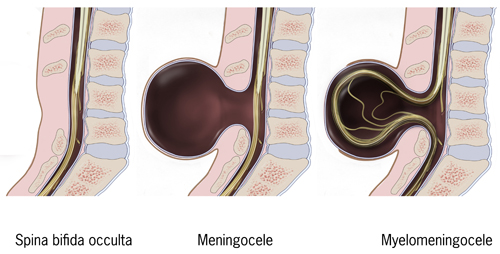
Spina bifida is a defect in the neural tube that occurs early in the pregnancy. There are several types of spinal bifida, as listed below:
- Spina bifida occulta: No neurological impairments, just a defect in the vertebra (pars interarticularis). Sometimes, a hairy patch, mole or dimple is evident on the skin over the site of the bony defect.
- Meningocele: A cystic swelling of the dura and arachnoid, protrudes through the spina bifida defect in the vertebral arch. Usually little or no neurological involvement.
- Myelomeningocele or Meningomyelocele (MMC): The spinal cord tissue extends into the meningocele, resulting in neurological damage below the level of the lesion.
Several risk factors are known to be associated with spina bifida. Maternal low RBC cell folate levels (folic acid supplements are recommended during pregnancy), exposure to some drugs (anti-seizure medications in particular), exposure to chemicals or environmental pollutants, maternal hyperthermia (fever, hot tubs, saunas, tanning beds), poorly controlled diabetes, and maternal obesity are risk factors. Women who have had one child with spina bifida are at a slightly higher risk for spina bifida to occur in subsequent pregnancies.
The neural tube in the embryo closes between day 17 and 30 in the gestation. If this window is missed, the neural tube will not close properly later in the pregnancy, resulting in spina bifida. If spina bifida is detected during the pregnancy by serum alpha-fetoprotein test, ultrasound, or amniocentesis, it is possible for surgical intervention in utero to help lessen the negative impacts of the disorder. Surgery can also be performed to close the defect after the baby is born. It is usually done within days of delivery.
For the purposes of this text, we will examine MMC, as this condition will be most important to physical therapists and physical therapist assistants.

Many children with MMC also have an Arnold-Chiari II formation in which the brainstem and cerebellum slip downwards into the foramen magnum. This disrupts the flow of cerebral spinal fluid, causing hydrocephalus, which is an abnormal accumulation of cerebral spinal fluid (CSF) in the brain.
In MMC, many other problems can occur. These include: flaccid or spastic paralysis of the lower limbs, urinary and or fecal incontinence, poor trunk control, musculoskeletal complications, scoliosis, hip dysplasia, hip dislocation, hip/knee muscle contracture, clubfoot, muscle atrophy. (Physiopedia: Meningomyelocele) Because of decreased sensation and mobility, children and adults with MMC are at risk for developing skin irritation and pressure sores. Allergy to latex is common in people with spina bifida.
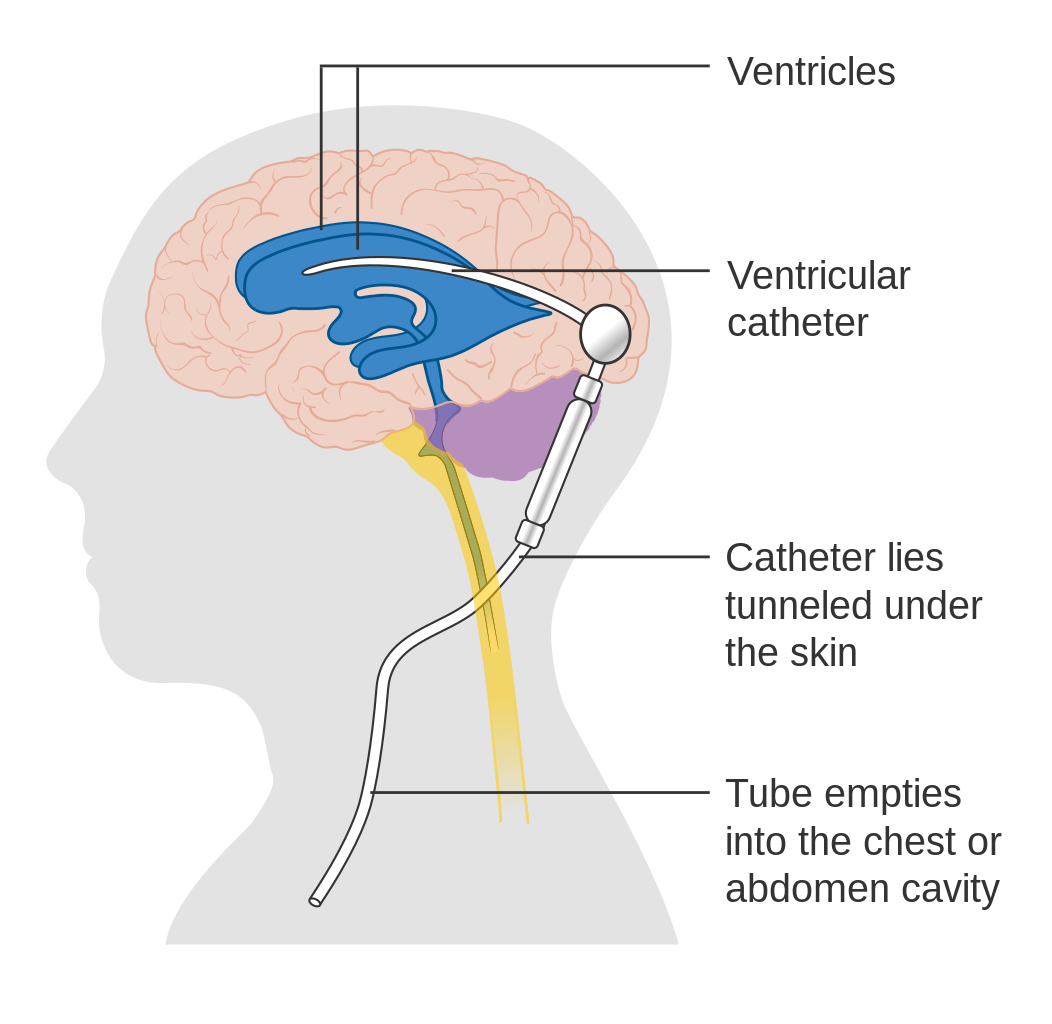
Surgical intervention is common in children with MMC, even after the defect is surgically closed. Ventro-peritineal (V-P) shunts are often used to treat the hydrocephalus.
Source: Cancer Research UK; retrieved from Wikipedia
Other interventions include surgeries to repair club feet, scoliosis, and hip dysplasia. Wheelchairs, bracing, and assistive devices are often required for mobility. Urinary and bowel problems are managed through self-catheterization are able to use a bowel management programs. Intellectual disabilities are more common in children with spina bifida than in the general population, and special assistance might be required in educational settings.
Children with MMC are usually referred to physical therapy for assitance with motor skills, especially mobility, as developmental delays are common. Depending upon the level and severity of the lesion, they might need assistive devices and braces or orthotics, or they might require a wheelchair for mobility. Stretching, muscle strengthening, and general mobility and fitness should be addressed.. Obesity is common as children with spina bifida age, so maintaining a physically active lifestyle is important. Physical therapists and PTAs can also help children and adults with MMC with prevention and treatment of skin breakdown through education about positioning, pressure relief, and skin inspection.
Many other health care professionals are involved in the care of children and adults with spinal bifida. Occupational therapists and assistants, speech-language pathologists, orthopedic surgeons, neurological surgeons, pediatricians, dietitians, and social services personnel are important team members in providing adequate health care. The transition to adulthood and finding meaningful employment can be difficult. A supportive family and network of professional social services and health care workers can help make this transition easier.
15.13 Fetal Alcohol Syndrome
This video gives a good summary of fetal alcohol syndrome (FAS).
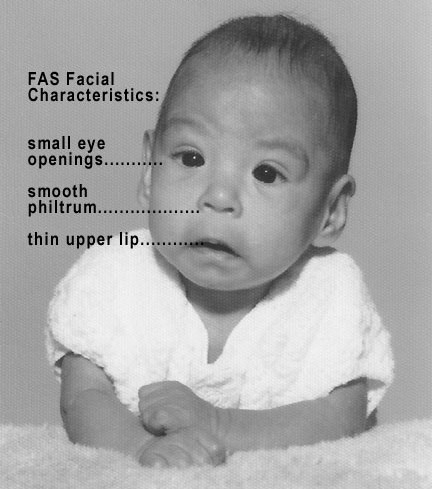
Fetal alcohol syndrome, or fetal alcohol spectrum syndrome, is a result of maternal alcohol use during pregnancy. It is characterized by growth retardation, cognitive disabilities, and physical disabilities in the child. Heart problems and limb dislocations are also more common in children with FAS. Many children with FAS experience seizures. Microcephaly is often seen in FAS. Facial features are also affected, usually small eyes and flattened upper lip area. All areas of the brain can be affected in FAS. Areas that are most often noted as affected in FAS are the corpus callosum, frontal lobe, hippocampus, and cerebellum. There is no specific diagnostic tool to identify FAS, so diagnosis is made through maternal history, and physical appearance and disabilities of the child. The brain damage in FAS is permanent. Children with FAS may need special education to manage intellectual disability, behavioral therapy to manage emotional and behavioral problems, physical and occupational therapy to manage motor delays, and speech language therapy to manage receptive and expressive speech difficulties. Medications are often used to control seizure disorders.
15.14 Mitochondrial Disorders
The following video (link) gives a good explanation of mitochondrial disorders. These disorders affect multiple organs and have multiple genetic causes. The scientific community is just beginning to understand these disorders. No truly effective treatment or cure is available for mitochondrial disorders at this time. Exercise to tolerance is known to be helpful in developing new mitochondria and in preserving function in affected mitochondria. Nutrition and vitamin supplements also seem to be helpful in managing mitochondrial diseases and in maintaining organ function. Antioxidants and coenzyme production stimulants are proving to be particularly useful in the treatment of mitochondrial disorders.
Mitochondrial Diseases: Current State of Understanding
Check Your Knowledge
General References:
MedlinePlus: Basic Information about Genes
MedlinePlus: Basic Information about Chromosomes
MedlinePlus: How Many Chromosomes do People Have?
Rare Diseases: Duchenne Muscular Dystrophy
Kravis, Elizabeth Berry. Medications in Fragile X. RUSH-Presbyterian-St. Luke’s Medical Center, Chicago, Illinois
Physio-Pedia: Down Syndrome (Trisomy 21)
NICHD: Maternal and Obstetric Manipulation
MedlinePlus: Genetic Disorders

