Chapter 14: Mental Health Conditions
Learning Objectives
After working through this chapter, the learner should be able to discuss risk factors, etiologic factors, pathogenesis, and clinical manifestations for the following mental health conditions:
- Dementia
- Schizophrenia
- Depression
- Bipolar disorder
- Post-traumatic stress disorder
- Generalized Anxiety disorder
- Autism spectrum disorder
- Substance abuse and addiction
Chapter Contents
14.1 Dementia
Dementia is defined as a decline in cognitive functioning. It is often associated with aging, but can be seen as a symptom of many neurological conditions which can affect younger individuals. Dementia can include many different symptoms, including memory loss, confusion, problem-solving difficulties, language and communication problems, motor planning problems, apraxia, spacial-dimensional dysfunction, perseverative behavior, and social and emotional problems. It is important to note that confusion and other symptoms of dementia can be caused by infections (especially UTI), medication side effects, alcohol use, fever, depression, dietary deficiencies, and thyroid problems. It is important that medical personnel consider these possibilities for a patient who seems uncharacteristically forgetful or confused.
There are several types of dementia. In this chapter, we will consider Lewy Body Dementia and Vascular Dementia. Alzheimer’s disease was covered in the chapter on Degenerative Neurological Disorders.
14.1.1 Lewy Body Dementia
In Lewy Body Dementia (LBD), specific abnormal deposits of a protein, called alpha-synuclein occur in the brain. These deposits are know as Lewy bodies. The Lewy bodies are associated with changes in brain chemicals, or neurotransmitters, such as dopamine and acetylcholine. The chemical changes are responsible for the symptoms of cognitive decline, movement problems, and alterations in mood and behavior. This type of dementia is quite common and is seen in Parkinson Disease. Not all people with LBD have Parkinson Disease, but most demonstrate parkinsonism, or characteristic movement patterns associated with Parkinson Disease (tremor, bradykinesia, muscular rigidity).
Some specific characteristics of LBD that distinguish it from other forms of dementia include:
-
- Memory problems often not present initially; cognitive problems more commonly include deficits in attention, visual and spatial abilities, planning, multitasking, problem solving, and reasoning.
- Fluctuations in cognitive function: A person with LBD may seem lucid one day and completely unable to function the next. They also often fluctuate in levels of attention. They can be alert and oriented at times, and at other times be very drowsy and sleepy.
- Hallucinations are more common in LBD than in other forms of dementia. The hallucinations are most often visual, although people sometimes hear voices or other sounds. The hallucinations usually involve realistic images, such as children or animals.
- Sleep disturbances often occur with LBD. People can have difficulty with REM sleep, insomnia, excessive sleepiness, and restless leg syndrome.
- Mood changes, including depression, anxiety, agitation, delusions, and paranoia are common.
- Other problems that can be found in people with LBD: changes in body temperature, changes in blood pressure, dizziness, falls, and urinary incontinence.
There is no cure for Lewy Body Dementia. There are medications available which might help slow the disease progression. Support for patients and caregivers is necessary and home modifications can help keep the patient at home. Many patients with LBD eventually are placed in a long-term care facility.
14.1.2 Vascular Dementia
If the brain does not receive adequate oxygen via the blood vessels in and around the brain, tissues will be damaged and one result can be dementia. One common cause for this type of dementia is stroke. Another is Alzheimer’s Disease. Even small clots in the arteries and capillaries can cause
changes in cognitive function, so any person with vascular inflammation and potential for blood clots (e.g. peripheral vascular disease, atherosclerosis, hypertension, diabetes) is at risk for vascular dementia.
Symptoms most commonly associated with vascular dementia include problems with reasoning, planning, judgement, memory or other cognitive function. The area of the brain that is anoxic is the most important factor in determining the exact symptoms of the condition.
As with other forms of dementia, there is no cure for vascular dementia. The diagnosis is generally made upon clinical presentation and can be supported by CT or MRI. There are medications available to slow the process, and “blood thinner” medications may help prevent future clots. Any comobities need to be treated and home modifications or placement in long-term facility will most likely be considered.
14.1.3 Treatment for Dementia
Treatment for different kinds of dementia is available. All interventions are aimed at maintaining communication, personal interaction, physical abilities and independence for as long as possible. Presently, there are no “cures” available for dementia, but there is help for patients and families. Some medications such as antidepressants, anti-anxiety medications, sleep aids, and medications used to treat Parkinson Disease can be prescribed to help with some of the symptoms and possibly slow the progression of dementia. Most patients with dementia will eventually lose the ability to live alone and care for oneself. In-home care or placement in a facility (memory unit) is often required. Support for caregivers and family members is important to consider when working with a patient with dementia.
For a good general introduction to neurology and the processes causing dementia, watch the following video:
“Dementia – Causes, Symptoms and Treatment Options” by Rehealthify is licensed under CC BY 4.0
14.2 Schizophrenia
Schizophrenia is a condition in which there is an abnormal perception of reality. It is a serious medical condition which requires life-long medical attention. It is generally diagnosed in the early 20’s in men and later 20’s in women and rarely diagnosed in children or older adults.
Signs and symptoms of schizophrenia include:
14.2.1 Delusions: Untrue thoughts. The thoughts and ideas of people with schizophrenia are often not based on reality and can be bizarre and highly unusual. People can believe others are “out to get them” or that someone they don’t even know, perhaps a celebrity, actually loves them. Delusions are the most common symptom of schizophrenia.
14.2.2 Hallucinations: Seeing things or hearing voices that are not real. People experiencing hallucinations truly experience the vision or sound. The most common hallucinations in schizophrenia are voices that often direct the behavior of the person with schizophrenia.
14.2.3 Disorganized thinking or speech: Inability to communicate meaningful thoughts. People with schizophrenia often cannot answer questions appropriately, either because their thoughts are disorganized or their speech is disorganized. This can lead to answering questions with unrelated information, beginning a thought with one idea, then quickly moving to a completely unrelated idea, or stringing unrelated words or syllables together in speech patterns that do convey recognizable thoughts or ideas.
14.2.4 Extremely disorganized or abnormal motor behavior: Performing inappropriate or unexpected activities or behaviors. Sometimes people with schizophrenia appear to be “acting out” with agitation or silliness. Sometimes the behavior is repetitive. The behavior is not goal-directed and can present an obstacle to purposeful behavior. Behaviors such as assuming an unusual posture, resisting directions, and complete lack of response are possible.
14.2.5 Negative behaviors: Often withdrawal-type behaviors. Social withdrawal, lack of eye contact, and neglect of personal hygiene are examples of negative behaviors.
The etiology of schizophrenia is unknown, but most researchers believe it is caused by a combination of genetics, brain chemistry, and the environment. Brain studies of people with schizophrenia show abnormalities in neurotransmitters and brain activity. Risk factors for developing schizophrenia include a family history of the condition, maternal malnutrition in the prenatal period, other prenatal or birth event (e.g. viral infection), and exposure to psychotrophic (mind-altering) drugs in the teen years.
Schizophrenia is a serious condition with many associated problems. Suicidal thought and actions are more common in people with schizophrenia than in people without the disorder. Other possible problems include depression, anxiety, alcohol abuse or other addictive behavior, social isolation, homelessness, other medical conditions, victimization, and rarely, aggressive behavior.
Unfortunately, schizophrenia is a life-long condition. It can be managed with medication, but the nature of the condition makes it difficult for the patient to follow-through with interventions. It is also difficult for the patient to maintain employment and form long-term relationships. For this reason, people with schizophrenia are at risk for financial problems, homelessness, and jail-time.
Medications used to treat schizophrenia include antipsychotic medications, psyhcosocial therapy for the patient, and coordinated specialty care (CSC) for the patient and family. CSC shows promise in helping patients and families manage this condition.
Sources: Mayo Clinic. Mayo Clinic: Schizophrenia
NIH: Schizophrenia
The following video helps explain important aspects of schizophrenia.
Osmosis.org video on schizophrenia
“Schizophrenia – causes, symptoms, diagnosis, treatment & pathology” by Osmosis is licensed under CC
14.3 Depression
Depression is a common and serious mental health condition. It is often referred to as “clinical depression” or “major depressive disorder.” It can affect people of any age and in any ethnic or socioeconomic group. In order to be diagnosed with depression, some of the following symptoms must be present for at least 2 weeks:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness, or pessimism
- Irritability
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Decreased energy or fatigue
- Moving or talking more slowly
- Feeling restless or having trouble sitting still
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, early-morning awakening, or oversleeping
- Appetite and/or weight changes
- Thoughts of death or suicide, or suicide attempts
- Aches or pains, headaches, cramps, or digestive problems without a clear physical cause and/or that do not ease even with treatment
Risk factors for developing depression include experiencing traumatic or upsetting life event, personal or family history of depression, and associated illness or medication.
Some forms of depression are slightly different, or they may develop under unique circumstances, such as:
- Persistent depressive disorder (also called dysthymia) is a depressed mood that lasts for at least two years. A person diagnosed with persistent depressive disorder may have episodes of major depression along with periods of less severe symptoms, but symptoms must last for two years to be considered persistent depressive disorder.
- Postpartum depression is much more serious than the “baby blues” (relatively mild depressive and anxiety symptoms that typically clear within two weeks after delivery) that many women experience after giving birth. Women with postpartum depression experience full-blown major depression during pregnancy or after delivery (postpartum depression). The feelings of extreme sadness, anxiety, and exhaustion that accompany postpartum depression may make it difficult for these new mothers to complete daily care activities for themselves and/or for their babies.
- Psychotic depression occurs when a person has severe depression plus some form of psychosis, such as having disturbing false fixed beliefs (delusions) or hearing or seeing upsetting things that others cannot hear or see (hallucinations). The psychotic symptoms typically have a depressive “theme,” such as delusions of guilt, poverty, or illness.
- Seasonal affective disorder is characterized by the onset of depression during the winter months, when there is less natural sunlight. This depression generally lifts during spring and summer. Winter depression, typically accompanied by social withdrawal, increased sleep, and weight gain, predictably returns every year in seasonal affective disorder.
(Source: NIH. Depression)
Depression can have serious consequences including poor interpersonal relationships, poor job performance, physical illness, and suicide. It is important that people with depression are treated. The most common interventions include antidepressive medications, such as selective seratonin reuptake inhibitors (SSRIs), psychotherapy (talk therapy), and brain stimulation therapy (electroconvulsive therapy, or ECT). Transcranial Magnetic Stimulation (TMS) is a newer type of electronic brain stimulation therapy that is showing some promise in the treatment of depression. TMS is generally conducted for one month.
The following video presents a good overview of clinical depression, causes, symptoms, and treatments.
Source: youtube.com/watch?v=QhukM33VLgo
“Clinical depression – major, post-partum, atypical, melancholic, persistent” by Osmosis is licensed under CC
14.4 Bipolar Disorder
Bipolar disorder, which used to be called manic-depressive disorder, is a condition in which the patient experiences periods of depression (lows), alternation with periods of extreme activity and even euphoria (highs or manic episodes). Bipolar disorder is less common than clinical depression, but it does affect many people. During lows, people demonstrate the same symptoms as depression (see above section). In manic episodes, people feel productive, confident, and happy. While the lows are easy to see as a “bad” thing, it is not as easy to see the highs as a “bad” thing. The manic periods can be dangerous, as they can lead to overspending, poor decision-making, feelings of grandeur, risk-taking, and extreme over-activity. A good video on bipolar disorder, types, associated risk factors, symptoms and behaviors, and treatments is below:
source: youtube.com/watch?v=KSvk8LLBo2g
“Bipolar disorder (depression & mania) – causes, symptoms, treatment & pathology” by Osmosis is licensed under CC
The cause of biploar disorder is not know, but it appears to be linked to genetics, as it is much more likely to be affected by bipolar disorder if one or more family members also has the disorder. Brain chemistry seems to play a part, as well, as some drugs that alter brain chemistry can trigger manic episodes.
Many people who have bipolar disorder may also demonstrate symptoms of other disorders, including anxiety, attention deficit and hyperactive disorder (ADHD), and substance abuse. The presence of accompanying symptoms and disorders makes the diagnosis of bipolar disorder difficult.
Bipolar disorder is treated with medications, including antidepressive (SSRI) medications, anti-anxiety medications, antipsychotic medications, and mood-stabilizing medications, such as lithium salts. It is not uncommon for people with bipolar disorder to dislike the “flat” feeling they might have when taking some of these medications, which can lead to poor compliance. Additional interventions include psychotherapy (talk therapy), ECT, and TMS.
14.5 Post-Traumatic Stress Disorder (PTSD)
The following video provides a good overview of PTSD.
source: youtube.com/watch?v=hzSx4rMyVjI
“Posttraumatic stress disorder (PTSD) – causes, symptoms, treatment & pathology” by Osmosis is licensed under CC
PTSD occurs in response to experiencing or witnessing a traumatic event. Many different kinds of events can be the source of PTSD, but war experiences and sexual trauma are two of the most common. It is not common to experience PTSD following a natural disaster.
PTSD symptoms are generally grouped into four types: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions. Symptoms can vary over time or vary from person to person.
Intrusive memories come in the form of nightmares, flashbacks, or obsessive thoughts. Avoidance behaviors include avoiding situations that might remind a person of the traumatic event or avoiding thinking about it all together. Mood or changes in thinking can take many forms with PTSD. People with PTSD might describe a feeling of numbness. They might have difficulty forming and maintaining close personal relationships. They might have negative feelings about themselves or feel hopeless about their present and future situations. Physical and emotional reactions vary greatly between individuals. Insomnia, intense anger or agitation, being easily startled or frightened, and concentration problems are common in PTSD.
People who have PTSD are at risk for other problems, as alcohol or other drugs or substances are often used to “self medicate.” Addiction is therefore a risk for people with this disorder.
Treatment for PTSD includes medications (anti-anxiety medications (SSSRs), antidepressants, and sleep aids) and psychotherapy. Group therapy seems to be important for people with PTSD and a social support network is valuable to avoid difficult future PTSD episodes.
source: Mayo Clinic Post-traumatic stress disorder (PTSD)
14.6 Generalized Anxiety Disorder
Generalized Anxiety Disorder (GAD)is defined as anxiety over everyday stresses that is persistent, excessive, or unreasonable. The exact cause of GAD is not known, but it seems to be associated with genetics, brain chemistry, and the environment. It is more common in women than men, in fact, women are twice as likely to be diagnosed with GAD. This disorder can lead to a lack of confidence and productivity and social isolation. It is also associated with physical conditions such as headaches , sleep problems, and digestive issues. Like many other mental health conditions discussed in this chapter, GAD may be most successfully treated with a combination of medications (anti-anxiety medications and antidepressants) and psychotherapy. Many people can learn useful strategies for overcoming their anxiety through cognitive behavior therapy.
Please watch the following video to learn more about GAD:
source: youtube.com/watch?v=9mPwQTiMSj8
“Generalized anxiety disorder (GAD) – causes, symptoms & treatment” by Osmosis is licensed under CC
14.7 Anorexia Nervosa (Anorexia)
Anorexia is a dangerous eating disorder that is associated with low body mass index (BMI), fear of weight gain, and unrealistic body image. Although anorexia is more common in girls and women than in males, it is important to note that it does occur in men, too.
People with anorexia may have specific eating rituals or avoid eating in front of people. In some individuals with anorexia, restriction of food intake and excessive exercise are present. Some individuals also engage in purging behaviors, such as self-induced vomiting or laxative use. Although anorexia has been reported in most of the world, it is much more common in cultures that value thinness and present a specific body image as “ideal.”
Some disorders that are likely to occur in conjunction with anorexia include perfectionism, need for control, anxiety, and depression.
People with anorexia are in danger of experiencing dysfunction in all body systems as the body is starved over time. Cardiac, neurological, respiratory, integumentary, hormonal, and immune systems can all be adversely affected by anorexia. The disorder can be very serious, even fatal.
Anorexia can be treated, but medical attention is necessary. The re-introduction of food and achievement of a normal weight needs to be progressed slowly with careful monitoring of vital signs, hormonal levels, and electrolyte levels. Treatment should include psychotherapy as well as medical monitoring. Family therapy is often beneficial, especially in younger patients.
Please watch the following video.
source: youtube.com/watch?v=olIz9MqtW-U
“Anorexia nervosa – causes, symptoms, diagnosis, treatment & pathology” by Osmosis is licensed under CC
14.8 Autism Spectrum Disorder
Autism spectrum disorder (ASD) is gaining attention in the United States as the number of people diagnosed with ASD has soared over the last few decades. According to the CDC, 1 in 59 children has ASD, with boys being four times more likely than girls to be affected by ASD. (source: Autism Speaks)
ASD is a life-long condition that is highly variable in its presentation. Asperger’s syndrome is a commonly used diagnostic term for people who are higher functioning (higher IQs, greater communication abilities, more successful in school and in social settings). Some people who have ASD also have very low IQs and other social and communication disorders that make functioning in a regular school setting or work environment difficult or impossible. Behavioral symptoms of ASD often include repetitive or restricted behaviors, interests or activities. With the wide range of disability posed by ASD, it is called a “spectrum disorder” and people with characteristics of ASD are often said to be “somewhere on the spectrum.”
The cause of autism is largely unknown. The prevailing belief is that it is cause by a genetic mutation or one or more specific genes. No environmental factors (parenting styles, vaccines, diets) have been scientifically proven to have an association with ASD. Autism is generally diagnosed between the ages of 2 and 10. Interventions include developmental therapy (Speech/Language, PT, OT, educational therapy) and academic accommodations. Talk therapy can also be quite effective in helping people identify and meet reasonable goals, and learn strategies to gain success in school and in social situations.
There exists a lack of understanding about ASD: what causes it and how to manage it. It presents as a different way of thinking that, in many cases, makes it difficult for people to be successful in life. People with ASD are helped by early intervention and assistance in communication and support from families and professionals. Accommodations are often necessary in educational settings.
The below video is geared toward diagnostic criteria. Since ASD is usually diagnosed in childhood, the video focuses on children. It is important to remember that people with ASD grow up and the symptoms persist through adulthood and can affect the ability to make and maintain relationships and find a successful employment path. Some individuals with ASD require highly specialized care and in some cases, placement in a facility that can provide a safe environment.
source: youtube.com/watch?v=x2hWVgZ8J4A
“Autism – causes, symptoms, diagnosis, treatment, pathology” by Osmosis is licensed under CC
14.9 Substance Abuse and Addiction
Substance abuse is a topic that covers a wide array of substances and problems. Addiction, as defined by the CDC is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences. Many different substances can lead to abuse and addiction. Some drugs are either illegal or available legally by prescription only . Some substances, such alcohol and tobacco/nicotine, are commonly used and highly addictive. All cause harm to the user and possibly to others, especially to family members and close acquaintances. This harm can be in the form of direct violence, physical, sexual, or psychological abuse, second hand smoke, or as a source of mental or psychological distress.
Opioid use in the US has become a particularly noteworthy problem, although as awareness has increased, opioid addiction and deaths from opioid overdose seem to be trending downward. This is true for most drugs.
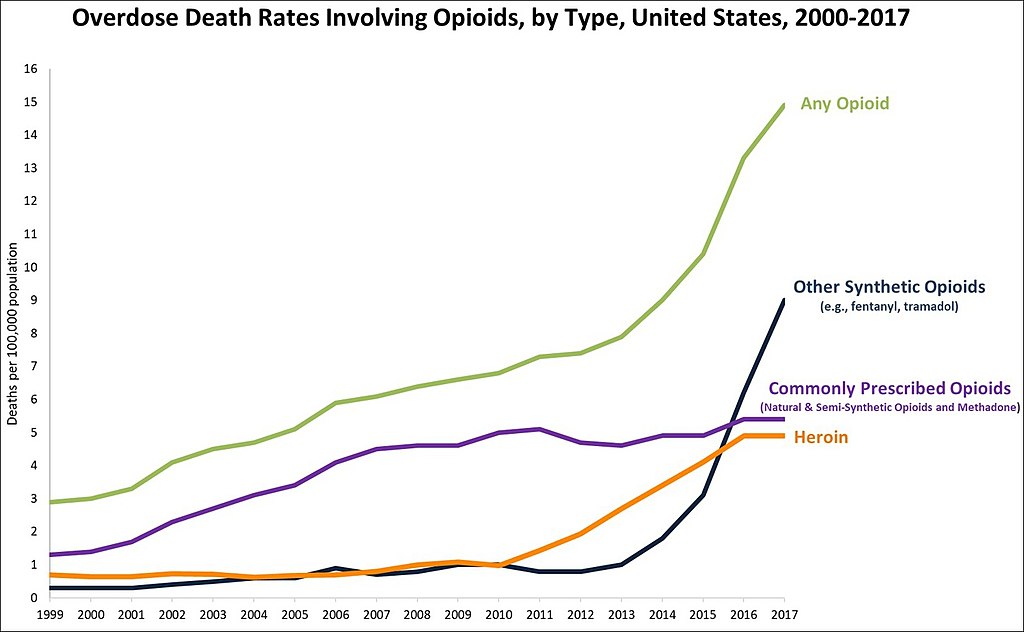
Source: This image is a work of the Centers for Disease Control and Prevention, part of the United States Department of Health and Human Services, taken or made as part of an employee’s official duties. As a work of the U.S. federal government, the image is in the public domain. Retrieved from Wikipedia : Drug overdose
Recent investigation of middle and high school students in the US show decreases in alcohol and most drug use. The ares of concern mainly center around increases in marijuana use and vaping, both of which are dangerous substances, particularly to young, immature brains.
National Institute on Drug Abuse (NIDA/NIH)
“Dr. Nora Volkow | A Message to Parents” by National Institute on Drug Abuse (NIDA/NIH) is licensed under CC BY
14.9.1 Drug Withdrawal and Detox
Addictions to substances need to be treated under medical supervision. Medications are available to help decreased the need for the drug and help calm anxiety and pain associated with withdrawal.During the initial stages of recovery, the body must rid itself of drugs. This is called the detox period. Detox can last several days to several weeks depending on the drug. Coping with withdrawal symptoms is often the most challenging part of detox. During detox, former drug users experience many uncomfortable symptoms. Some of these may include:
-
- Anxiety
- Depression
- Nausea
- Seizures
- Muscle aches
- Sweating
Different medications are used to treat different withdrawal symptoms. Some of the drugs that physicians prescribe in detox include:
-
Benzodiazepines
These drugs reduce anxiety and irritability. Anxiety is a common symptom of withdrawal from many drugs, including cocaine and opiates like heroin. Benzos have a sedative effect, which helps ease alcohol withdrawals. Doctors are cautious about prescribing benzos because they are addictive.
-
Antidepressants
Without drugs, an addicted person cannot produce natural amounts of happiness-inducing chemicals in their brain. Because they’ve relied on drugs to keep them happy for so long, people in detox often experience depression. Antidepressants like Zoloft and Prozac can help relieve these feelings until the brain is able to produce happiness-inducing chemicals on its own again.
-
Clonidine
Used to treat alcohol and opiate withdrawals, Clonidine reduces sweating, cramps, muscle aches and anxiety. Clonidine can also stop tremors and seizures.
Detoxing from alcohol or benzodiazepines like Valium or Xanax can be deadly, so people with these addictions should never quit “cold turkey.” Withdrawals from other drugs aren’t always life-threatening, but complications can still arise. Medical help ensures safety and success in detox. If you are suffering from an addiction, talk to someone who can help now.
14.9.2 Alcohol Addiction Medications
Abusing alcohol on a regular basis for a long time can prolong withdrawal symptoms, lasting anywhere from weeks to months. This phenomenon is called prolonged or post-acute withdrawal syndrome (PAWS). Maintenance therapy can relieve PAWS and may also curb cravings or make the user unable to stomach alcohol. These medications usually come as a tablet that patients take each day.
Medications for alcohol addiction include:
-
Naltrexone (Vivitrol)
Naltrexone blocks receptors in the brain that produce alcohol’s pleasurable effects. It also subdues the urge to drink. Naltrexone may cause some nausea or headaches. It may be given via injection every four weeks.
-
Acamprosate (Campral)
This medication relieves emotional and physical distress caused by alcohol addiction. Recovering alcoholics can start taking acamprosate after completing detox. Acamprosate reduces the urge to drink by preventing negative feelings like anxiety and depression.
-
Disulfiram (Antabuse)
Disulfiram was the first medication approved for alcoholism. If a person taking disulfiram drinks, the medication causes side effects such as nausea and vomiting. The idea is that those taking disulfiram won’t drink if it makes them sick.
14.9.3 Heroin and Opiate Addiction Medications
Opiates include heroin, morphine and narcotic painkillers like Oxycontin. Medications for opiate and heroin treatment ease cravings and withdrawal symptoms. These medications are usually provided in tablet form on a daily basis. Some people experience heroin and opiate withdrawal for as little as a week. Others may have long-term withdrawal symptoms. The symptoms of withdrawal can last for months or years in some cases. Long-term replacement medications can stop cravings and PAWS. Former users can typically take medications for as long as necessary.
Addiction medications for heroin and painkillers include:
-
Methadone
Methadone is an opiate used for moderate to severe opiate addictions. It works by binding to the same receptors in the brain as heroin and painkillers, but methadone doesn’t get the user high. This helps suppress cravings and withdrawal symptoms. Methadone is used with caution because some people have become addicted to it in place of heroin and painkillers. Methadone clinics dispense the drug on a daily basis to prevent abuse. Learn more about methadone.
-
Buprenorphine (Suboxone)
Buprenorphine works in the same manner as methadone but is less closely regulated because the addiction potential is lower. Buprenorphine users can often take the drug home with them instead of going to a clinic every day to get it.
-
Naltrexone
Naltrexone works the same way for opiate addiction as it does for alcohol addiction. It stops the urge to use. It works for both addictions because alcohol and opiates activate some of the same receptors in the brain.
14.9.3 Medical Detox and Rehab
Some people choose to detox on their own. This is not only harder, but also more dangerous than detoxing with a doctor. Medical detox is the best way to get sober in a safe, comfortable environment. For those addicted to alcohol or benzos, medical detox is a must.
A supervised detox can alleviate health issues. Physicians track the patient’s heart rate, temperature, breathing rate and fluid levels. Physicians help relieve any discomfort the patient may be feeling. They also adjust any medication doses according to the patient’s needs and make long-term plans for medication. Those with separate health issues should also seek medical detox. Withdrawals can complicate problems like high blood pressure. A physician can prevent any issues.
Detox is often a part of inpatient rehabs. In most cases, inpatient rehab takes 30 to 90 days. The first week consists of closely observed detox. Rehab includes other treatments, such as behavioral therapy, to make recovery more successful.
source: Addiction Center: Treatment Medications
One additional drug that should be mentioned is Naloxone (Narcan), which is used as a fast-acting counteracting drug to opioid overdose.
For nicotine addiction (cigarettes, chewing tobacco, vaping, cigars, pipes), nicotine withdrawal medications are available over the counter and in stronger doses via prescriptions. These medications are usually administered orally in gum or transdermal patch (skin patch).
Understanding Drug Use and Addiction
Revised June 2018
Many people don’t understand why or how other people become addicted to drugs. They may mistakenly think that those who use drugs lack moral principles or willpower and that they could stop their drug use simply by choosing to. In reality, drug addiction is a complex disease, and quitting usually takes more than good intentions or a strong will. Drugs change the brain in ways that make quitting hard, even for those who want to. Fortunately, researchers know more than ever about how drugs affect the brain and have found treatments that can help people recover from drug addiction and lead productive lives.
What Is drug addiction?
Addiction is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences. The initial decision to take drugs is voluntary for most people, but repeated drug use can lead to brain changes that challenge an addicted person’s self-control and interfere with their ability to resist intense urges to take drugs. These brain changes can be persistent, which is why drug addiction is considered a “relapsing” disease—people in recovery from drug use disorders are at increased risk for returning to drug use even after years of not taking the drug.
It’s common for a person to relapse, but relapse doesn’t mean that treatment doesn’t work. As with other chronic health conditions, treatment should be ongoing and should be adjusted based on how the patient responds. Treatment plans need to be reviewed often and modified to fit the patient’s changing needs.
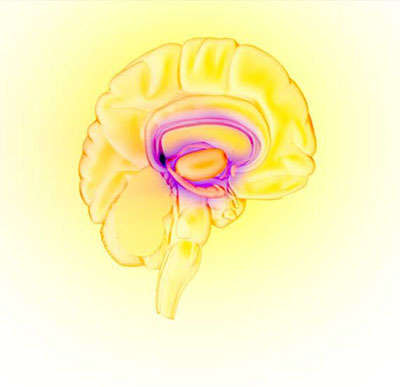
Image by NIDAThe brain’s reward circuit
What happens to the brain when a person takes drugs?
Most drugs affect the brain’s “reward circuit,” causing euphoria as well as flooding it with the chemical messenger dopamine. A properly functioning reward system motivates a person to repeat behaviors needed to thrive, such as eating and spending time with loved ones. Surges of dopamine in the reward circuit cause the reinforcement of pleasurable but unhealthy behaviors like taking drugs, leading people to repeat the behavior again and again.
As a person continues to use drugs, the brain adapts by reducing the ability of cells in the reward circuit to respond to it. This reduces the high that the person feels compared to the high they felt when first taking the drug—an effect known as tolerance. They might take more of the drug to try and achieve the same high. These brain adaptations often lead to the person becoming less and less able to derive pleasure from other things they once enjoyed, like food, sex, or social activities.
Long-term use also causes changes in other brain chemical systems and circuits as well, affecting functions that include:
- learning
- judgment
- decision-making
- stress
- memory
- behavior
Despite being aware of these harmful outcomes, many people who use drugs continue to take them, which is the nature of addiction.
Why do some people become addicted to drugs while others don’t?
No one factor can predict if a person will become addicted to drugs. A combination of factors influences risk for addiction. The more risk factors a person has, the greater the chance that taking drugs can lead to addiction. For example:

- Biology. The genes that people are born with account for about half of a person’s risk for addiction. Gender, ethnicity, and the presence of other mental disorders may also influence risk for drug use and addiction.
- Environment. A person’s environment includes many different influences, from family and friends to economic status and general quality of life. Factors such as peer pressure, physical and sexual abuse, early exposure to drugs, stress, and parental guidance can greatly affect a person’s likelihood of drug use and addiction.
- Development. Genetic and environmental factors interact with critical developmental stages in a person’s life to affect addiction risk. Although taking drugs at any age can lead to addiction, the earlier that drug use begins, the more likely it will progress to addiction. This is particularly problematic for teens. Because areas in their brains that control decision-making, judgment, and self-control are still developing, teens may be especially prone to risky behaviors, including trying drugs.
Can drug addiction be cured or prevented?
As with most other chronic diseases, such as diabetes, asthma, or heart disease, treatment for drug addiction generally isn’t a cure. However, addiction is treatable and can be successfully managed. People who are recovering from an addiction will be at risk for relapse for years and possibly for their whole lives. Research shows that combining addiction treatment medicines with behavioral therapy ensures the best chance of success for most patients. Treatment approaches tailored to each patient’s drug use patterns and any co-occurring medical, mental, and social problems can lead to continued recovery.
More good news is that drug use and addiction are preventable. Results from NIDA-funded research have shown that prevention programs involving families, schools, communities, and the media are effective for preventing or reducing drug use and addiction. Although personal events and cultural factors affect drug use trends, when young people view drug use as harmful, they tend to decrease their drug taking. Therefore, education and outreach are key in helping people understand the possible risks of drug use. Teachers, parents, and health care providers have crucial roles in educating young people and preventing drug use and addiction.
Points to Remember
- Drug addiction is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences.
- Brain changes that occur over time with drug use challenge an addicted person’s self-control and interfere with their ability to resist intense urges to take drugs. This is why drug addiction is also a relapsing disease.
- Relapse is the return to drug use after an attempt to stop. Relapse indicates the need for more or different treatment.
- Most drugs affect the brain’s reward circuit by flooding it with the chemical messenger dopamine. Surges of dopamine in the reward circuit cause the reinforcement of pleasurable but unhealthy activities, leading people to repeat the behavior again and again.
- Over time, the brain adjusts to the excess dopamine, which reduces the high that the person feels compared to the high they felt when first taking the drug—an effect known as tolerance. They might take more of the drug, trying to achieve the same dopamine high.
- No single factor can predict whether a person will become addicted to drugs. A combination of genetic, environmental, and developmental factors influences risk for addiction. The more risk factors a person has, the greater the chance that taking drugs can lead to addiction.
- Drug addiction is treatable and can be successfully managed.
- More good news is that drug use and addiction are preventable. Teachers, parents, and health care providers have crucial roles in educating young people and preventing drug use and addiction.
Learn more
For information about understanding drug use and addiction, visit:
- National Institute on Drug Abuse: Drugs, Brains, and Behavior: The Science of Addiction
- National Institute on Drug Abuse: Adolescent Brain
- National Institute on Drug Abuse: Drugs, Brains, and Behavior: Parents & Educators
For more information about the costs of drug abuse to the United States, visit:
For more information about prevention, visit:
For more information about treatment, visit:
To find a publicly funded treatment center in your state, call 1-800-662-HELP or visit:

Long Description
Title: Graph of harm caused by drugs.
A horizontal bar chart displays the harm caused by drugs which include total harm, harm to others and harm to the user. The following table lists the values.
| Drug | Total Harm | Harm to Others | Harm to Users |
|---|---|---|---|
| Alcohol | 72 | 45 | 27 |
| Heroin | 54 | 22 | 32 |
| Crack cocaine | 53 | 18 | 35 |
| Methamphetamine | 33 | 2 | 31 |
| Cocaine | 27 | 8 | 19 |
| Tobacco | 26 | 9 | 17 |
| Amphetamine | 23 | 4 | 19 |
| Cannabis | 20 | 8 | 12 |
| GHB | 18 | 2 | 16 |
| Benzodiazepines | 16 | 3 | 13 |
| Ketamine | 16 | 2 | 14 |
| Methadone | 14 | 3 | 11 |
| Mephedrone | 13 | 1 | 12 |
| Butane | 11 | 1 | 10 |
| Anabolic steroids | 10 | 2 | 8 |
| Ecstasy | 9 | 1 | 8 |
| Qat/khat | 9 | 1 | 8 |
| LSD | 7 | 0 | 7 |
| Buprenorphine | 7 | 2 | 5 |
| Mushrooms | 6 | 0 | 6 |
Source:“Scoring drugs”, The Economist, data from “Drug harms in the UK: a multi-criteria decision analysis”, by David Nutt, Leslie King and Lawrence Phillips, on behalf of the Independent Scientific Committee on Drugs. The Lancet. 2010 Nov 6;376(9752):1558-65. doi:10.1016/S0140-6736(10)61462-6 PMID:21036393
Drug Science: MCDA Comparison of Drug and Alcohol Harms in the UK
Resources
NIH: National Institute on Drug Abuse
NIH: Understanding Drug Use and Addiction DrugFacts
WHO – World Health Organization: Opioid overdose

