Chapter 20: Hepatic and Biliary Systems
Learning Objectives
After completing this chapter, the learner should be able to:
- Define the basic terminology associated with conditions hepatic dysfunction.
- Discuss basic medical diagnosis of hepatic disorders.
- List some common signs and symptoms of hepatic and biliary conditions.
- Discuss risk factors, etiologic factors, pathogenesis, and clinical manifestations for the following hepatic and biliary conditions:
- Cirrhosis of the liver
- Hepatitis
- Alcohol-related disorders
- Describe medical, surgical and physical therapy interventions associated with hepatic conditions.
- Describe the pharmacological management of hepatic conditions.
- Discuss precautions, indications and contraindications to be considered in physical therapy interventions for patients with hepatic conditions.
- Recognize the signs and symptoms of acute hepatic conditions and discuss appropriate course of action.
Chapter Contents
The Hepatic and Biliary Systems
20.1 Liver
The liver is a large and very important organ in the body. It’s varied functions are listed below:
- Stores vitamins, minerals, and sugar, which are utilized in times of stress or starvation
- Produces proteins, which are necessary for normal body functions
- Produces bile, which is necessary for digesting fats and absorbing Vitamins A, D, E, and K
- Produces substances that help in blood clotting
- Removes harmful bacteria and potentially dangerous byproducts from medications from the blood
- Metabolizes nutrients from food to store and use for energy when needed
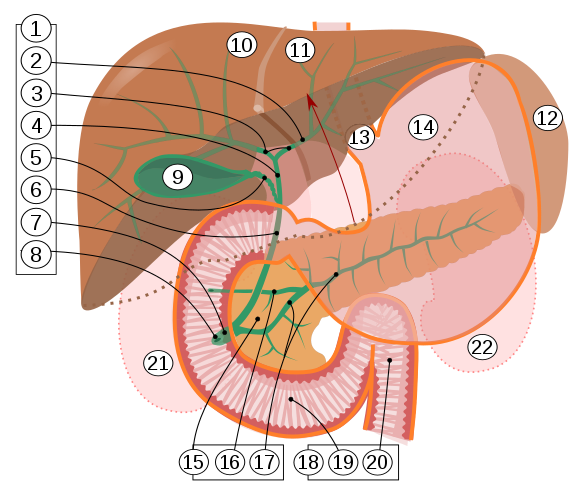
The liver is connected to the gall bladder and pancreas through a series of tubes, or ducts, which are known as the biliary system. The biliary tract refers to the liver, gall bladder and bile ducts and how they produce, secrete, and store bile. Bile is secreted by the liver, stored in the gall bladder between meals, and transported to the duodenum during meals. Bile aids in the digestion of fats and oils.
For a short video introduction to the liver and liver dysfunction, see the video at the following site:
20.1 Resource 2 – “Progression of Liver Disease Webcast Series: Cirrhosis and Signs of Liver Failure” by American Liver Foundation is licensed under CC BY 4.0
YouTube video
In the early stages of liver disease, there are often no signs or symptoms. When the liver damage is more advanced, general symptoms can be present. A list of the signs and symptoms of liver problems can be found in the text box.

Although some forms of liver disease occur in seemingly healthy individuals, there are some risk factors for many conditions affecting the liver. Risk factors include: alcohol use, injected drug use, multiple sex partners, diabetes, obesity, and food and water contamination. These risk factors will be discussed further in conjunction with specific diseases and conditions in later sections.
20.2 Conditions of the Liver
Liver conditions are diagnosed through lab tests of the blood, ultrasound of the liver and surrounding structures, endoscopy, and the gold standard, liver biopsy.
20.2.1 Cirrhosis
The most common causes of hepatic cirrhosis include alcoholic liver disease, non-alcoholic steatohepatitis (NASH), progressive fatty liver disease, and chronic hepatitis B or hepatitis C infection. When liver damage is present, the liver experiences three main stages: fatty liver, liver fibrosis, and finally, cirrhosis. The liver becomes less functional as more liver cells are replaced by fibrinous tissue.
If liver disease is diagnosed in early stages and the inciting cause is removed, the changes in the liver are fully reversible. In cirrhosis, the normal functioning liver cells are replaced by fibrinous scar tissue and the damage is not reversible. As the liver becomes increasingly fibrotic, liver function decreases and hepatic blood flow is restricted. The liver becomes hard and stiff, restricting blood flow through it. Portal hypertension (increased blood pressure in the portal vein) results, causing varices, which are large distended veins around the esophagus and stomach. These veins can easily rupture and bleed. The spleen is also involved, adversely affecting its ability to release platelets. Sometimes, liver cancer develops in association with cirrhosis. Signs and symptoms of advanced hepatic cirrhosis include:
- bleeding and bruising due to decreased circulating platelets
- hepatic encephalopathy, resulting from ammonia and other toxins not being cleared by the liver, building up in the blood and the brain and affecting cognitive function
- increased sensitivity to medication as the liver fails to metabolize substances
- acute kidney injury
- cachexia (muscle wasting)
Cirrhosis can not be cured, but some interventions can help slow progression and reduce complications. A healthy diet is important in maintaining energy. Infections need to be treated quickly with antibiotics. Alcohol consumption should be avoided, even in cases not caused by alcohol. If cirrhosis is caused by hepatitis, antivirals are important. Control of weight and diabetes is important in non-alcoholic liver disease. Liver transplantation may be appropriate for some individuals.
20.2.2 Fatty Liver Disease
Fatty liver disease is divided into two main categories: alcoholic and nonalcoholic.
20.2.3 Alcoholic Fatty Liver Disease
Fatty liver disease caused by overconsumption of alcohol, is a type of alcoholic liver disease (ALD), or alcohol-related liver disease (RLD). This disease is reversible in the “fatty” stages, but can progress to cirrhosis or liver cancer if alcohol consumption continues.
Although the mechanism of the development of ALD is not completely understood, it is know that in the presence of large quantities of alcohol, which must be metabolized by the liver, normal liver cells can be infiltrated or replaced by large, fatty globules. Pro-inflammatory cytokines are secreted in large numbers, causing inflammation, apoptosis and fibrosis of liver cells. Individuals are more likely to develop ALD and fatty liver disease if the quantity and frequency of drinking is heavy; if they have other hepatitis infection; or if they have genetic predisposition; if they have dietary deficiencies. Also, women are more susceptible to alcohol-related liver disease than men.
There are no medications available at this time that are known to treat any liver conditions related to alcoholism. The consumption of alcohol must be ceased. Once the disease progresses to cirrhosis, changes to the liver cannot be reversed, and liver transplantation may be the only option.
20.2.4 Non-Alcoholic Fatty Liver Disease (NAFLD) and Non-Alcoholic Steatohepatitis (NASH)
The disease progression in liver conditions NOT associated with alcohol are similar to those associated with alcohol, the cause of the diseases is different. Risk factors for NAFLD and NASH include: overweight, metabolic syndrome (includes hypertension, high blood sugar, and high triglycerides), diabetes, diet high in fructose, and older age. Contributing factors include alcohol use, hepatitis infection, and some medications. In NFFLD, liver function is preserved, but in NASH, liver function is severely diminished, leading to cirrhosis and liver cancer.


http://www.niddk.nih.gov/health-information/health-topics/liver-disease/nonalcoholic-steatohepatitis/Pages/facts.aspx
Retrieved from Wikipedia: Hepatitis
Management of NAFLD and NASH include weight-loss, control of blood glucose levels, diet, and exercise. There are no medications that specifically treat NAFLD or NASH. While NAFLD in early stages is completely reversible with lifestyle changes, NASH or NAFLD that has progressed to NASH are not reversible. Both conditions greatly increase the risk of liver cancer and cirrhosis. In some individuals, liver transplantation is an appropriate life-sustaining measure.
20.2.5 Hepatitis
20.2.5.1 Hepatitis A
Hepatitis A is a highly-contagious virus affecting the liver that is transmitted via injected drug use, person-to-person contact through body fluids or feces, sexual contact, or in infected food or water. People who are at the highest risk for Hepatis A infection include international travelers, homeless people, and health care workers, and men who have sex with men. Hepatitis A is an RNA virus that can remain viable outside the body for several months, so potential for transmission is significant. Once in the body, Hepatitis A incubates in the liver, causing characteristic signs and symptoms, including vomiting, loss of appetite, fatigue, abdominal pain, diarrhea, joint pain, fever, dark urine, clay colored feces, and jaundice.
For most people Hepatitis A will resolve in 6-8 weeks and the infected person will suffer no long-term effects from the virus. Hepatitis A can be detected in the blood, and laboratory examination of blood can confirm a diagnosis. Treatment is usually symptom-related. Antiviral medications can be used for people at highest risk for severe disease, mostly those with depressed immune systems. A vaccine is available and recommended for children over 1 year of age, those in high-risk groups, and anyone with a potentially depressed immune system. The hepatitis A vaccine has been part of the recommended childhood vaccination series since 1994.
20.2.5.2 Hepatitis B
The hepatitis B virus is a DNA virus with the potential to cause long-lasting health concerns for infected individuals. Hepatitis B is transmitted through contact with contaminated blood or blood products, sexual contact, and IV injections or drug use. Transmission has occurred in non-sterile environments during tattooing, acupuncture, body piercing, and manicures/pedicures. In addition, babies born to mothers with hepatitis B are at a greater than 90% risk of contracting chronic the virus and living with chronic liver disease throughout their lives.
Risk factors for contracting the virus include health care professions, IV drug use, multiple sexual partners, or one sexual partner who has hepatitis B, and being born in or travelling to counties know to have high numbers of infected individuals.
Hepatitis B is often referred to as a “silent infection” because most people do no have symptoms when they are first infected, or even in the presence of chronic infection. Only in the later stages of liver failure do symptoms present. If there are symptoms, they most often include fatigue, mild fever, muscle or joint pain, loss of appetite, abdominal pain, vomiting or diarrhea, light colored stools, and dark colored urine. Hepatitis B can lead to liver cancer, which is a very dangerous form of cancer.
Treatment for HBV in acute infections is usually symptom-related. Antiviral drugs can be useful in treating chronic HBV infections. People who are taking antiviral drugs for an extended period need to have frequent testing of liver and kidney function, as these drugs can be damaging.
The hepatitis B vaccine was developed in 1981 and became widely used in the 1990s . This vaccine was the first vaccine identified as a cancer-preventing vaccine, as the vaccine prevents hepatitis B, which is a known cause of liver cancer. In fact, it is estimated that over 80% of liver cancer is caused by hepatitis B or hepatitis C infections.
20.2.5.3 Hepatitis C
Most people do not show signs and symptoms in the acute infection with HCV. If they do show symptoms, they are usually mild, often fever, fatigue, abdominal discomfort, clay colored stool, dark urine, jaundice and loss of appetite. In chronic conditions, HCV causes liver cirrhosis, liver cancer, and liver failure.
- medical evaluation (by either a primary-care clinician or specialist [e.g., in hepatology, gastroenterology, or infectious disease]) for chronic liver disease, including treatment and monitoring;
- hepatitis A and hepatitis B vaccination;
- screening and brief intervention for alcohol consumption; and
- HIV risk assessment and testing.
Hepatitis C is curable in both the acute and chronic forms. Direct-acting antiviral drugs (DAAs), such as ledipasvir, are important standards of care for HCV infection. Harvoni, a combination drug (DAA + nucleotide analog inhibitor) is often used to treat HVC. The cost of this medication is sometimes prohibitive: The wholesale acquisition cost (WAC) for ledipasvir-sofosbuvir is $1125 per pill.
- Cost of 8-week course of therapy = $63,000
- Cost of 12-week course of therapy = $94,500
- Cost of 24-week course of therapy = $189,000
Hepatitis C Online: Ledipasvir-Sofosbuvir (Harvoni)
Other medications, such as ribavirin and protease inhibitors, and interferons are also used in treating HCV. There is no vaccine currently available for HCV. Limiting risk factors and participating in screenings are the only preventative measures known at this time.
20.2.5.4 Hepatitis D
20.2.5.5 Hepatitis E
Hepatitis E is rare in the United States. It is transmitted through the fecal-oral route and is transmitted mainly through contaminated drinking water in developing countries. People also become infected by eating raw or undercooked pork, venison, wild boar meat, or shellfish. Symptoms of hepatitis E can include fatigue, poor appetite, stomach pain, nausea, and jaundice. Most people have no symptoms or mild symptoms, and most recover without complications. Only those with weakened immune systems seem to develop chronic hepatitis E infections. There is no vaccine available for HEV in the United States. Prevention measures include maintaining adequate sanitation methods, ensuring clean drinking water, and avoiding undercooked pork, boar, and shellfish.
20.2.5.6 Alcoholic Hepatitis
Some, but not all people, who drink alcohol will get alcoholic hepatitis. The reasoning behind the differing effects on different people is not completely understood, but the damage alcohol can do to the liver is well-documented. Although this type of hepatitis is not infectious, it causes inflammation of the liver and associated symptoms that are very similar to viral hepatitis. Jaundice, abdominal pain, nausea, vomiting, fever, and fatigue are most common. If the affected individual continues to drink alcohol, the liver damage will progress to cirrhosis and symptoms could include ascites, hepatic encephalopathy, and liver and kidney failure. The risk of liver cancer becomes significant. The main treatment for alcoholic hepatitis is to stop drinking alcohol. If the damage to the liver is severe, and the patient is a good candidate for surgery, liver transplantation is an option.
Biliary System
The conditions associated with dysfunction of the biliary system are covered in the chapter on digestive disorders. Further information can be found at Kenhub: Common disorders of the biliary system.
The Hepatic and Biliary Systems
Section 20.1
Resource 01 “Biliary tract” by Jmarchn is licensed under CC BY-SA 3.0
Wikipedia: Biliary tract
Resource 2 – “Progression of Liver Disease Webcast Series: Cirrhosis and Signs of Liver Failure” by American Liver Foundation is licensed under CC BY 4.0
Resource 3 – “Hepatitis” by Centers for Disease Control and Prevention, is in the Public Domain
Wikipedia: Hepatitis
Section 20.2
Resource 1 – NAFLD Prevalence in 2019 “NAFLD Prevalence in 2019” by Signimu is licensed under CC BY 1.0
Wikipedia: NAFLD prevalence 2019
Resource 02 – “Stages of Liver Disease” by NIDDK, NIH is in the Public Domain
http://www.niddk.nih.gov/health-information/health-topics/liver-disease/nonalcoholic-steatohepatitis/Pages/facts.aspx
Retrieved from Wikipedia: Hepatitis
General resources
CDC: 2018 Hepatitis Surveillance
Hepatitis C Online: Ledipasvir-Sofosbuvir Treatment

