Chapter 12: The Integumentary System
Learning Objectives
After completing this chapter, the students should be able to:
- Define the basic terminology associated with integumentary conditions.
- Discuss basic data collection methods of integumentary disorders.
- List some common signs and symptoms of skin disease.
- Discuss changes in the skin that are associated with aging.
- Discuss risk factors, etiologic factors, pathogenesis, and clinical manifestations for selected integumentary conditions.
- Identify tissue types which are viable and nonviable in a wound.
- Identify various types of exudates in damaged tissue and list possible associated conditions.
- Describe medical, surgical and physical therapy interventions associated with integumentary conditions.
- Describe the pharmacological management of integumentary conditions
- Discuss precautions, indications and contraindications to be considered in physical therapy interventions for patients with integumentary conditions.
Chapter Contents
- 12.1 Basic Terminology
- 12.1.1 Macule
- 12.1.2 Papule
- 12.1.3 Plaque
- 12.1.4 Nodule
- 12.1.5 Tumor
- 12.1.6 Wheal
- 12.1.7 Pustule
- 12.1.8 Vesicle
- 12.1.9 Blister
- 12.1.10 Bulla
- 12.1.11 Maceration
- 12.1.12 Puritis
- 12.1.13 Uticaria
- 12.1.14 Ichthyosis
- 12.1.15 Xeroderma
- 12.1.16 Telangiectasis
- 12.1.17 Raynaud Phenomenom
- 12.1.18 Sclerodactyly
- 12.1.19 Data Collection
- 12.2 – Aging Skin
- 12.3 – Integumentary Conditions and Injuries
- 12.3.1 Noncommunicable conditions
- 12.3.2 – Communicable Integumentary Conditions
- 12.3.3 – Skin Conditions Associated With Other Conditions
- 12.3.4 – Thermal injuries, including frostbite and burns
- 12.3.4.1 Superficial (first-degree)
- 12.3.4.2 Superficial partial thickness (second-degree)
- 12.3.4.3 Deep partial thickness (second-degree)
- 12.3.4.4 Full thickness (third-degree)
- 12.3.4.5 Fourth-degree
- 12.3.5 – Tissue injury, e.g. pressure ulcers, venous and arterial wounds
- 12.3.5.1 Vascular Conditions and Ulcerations
- 12.3.5.2 Peripheral Venous Insufficiency (PVI)
- 12.3.5.3 Peripheral Artery Disease (PAD)
- 12.3.5.4 Pressure Injury
- 12.3.5.5 Wound Care
- 12.3.5.6 Viable and Nonviable Tissue
- 12.3.5.7 Viable tissu
- 12.3.5.8 Nonviable tissue
- 12.3.5.9 Scarring Complications
- 12.3.5.10 Goals of wound care
- 12.3.5.11 PTA Role in Wound Care
- 12.3.6 – Skin cancer
12.1 – Basic Terminology
The skin is the basic covering for most of the body, and changes in the skin can be associated with benign or serious conditions. The skin itself can be infected, as in cellulitis, or rashes covering the skin can be entirely the result of other conditions, such as rashes associated with measles or pox associated with chicken pox. Integumentary conditions can take many forms and there are many terms associated with changes in the integumentary system. Some of the most common are listed below.
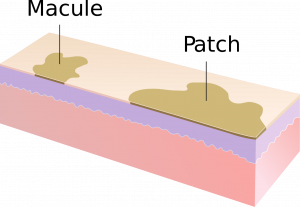
12.1.1 Macule:
a broad, flat area of skin discoloration, usually less than 1 cm in diameter; it is not raised or depressed, and the thickness of the skin is not affected. A larger area of discoloration is generally termed a patch.
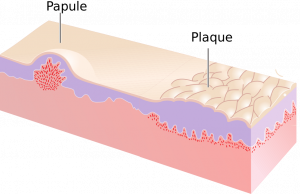
12.1.2 Papule:
a raised area of skin, with no fluid, varying in size
12.1.3 Plaque:
a large papule or grouping of papules; the diameter of a plaque is greater than its elevation
12.1.4 Nodule:
a solid raised “bump” in the skin: similar to a papule, but centered deeper in the skin
12.1.5 Tumor:
similar to a nodule, but larger in diameter and depth
12.1.6 Wheal:
a papule or plaque that disappears in 48 hours or less
12.1.7 Pustule:
raised area of the skin, containing cloudy liquid or pus (acne pimple is a good example of a pustule)
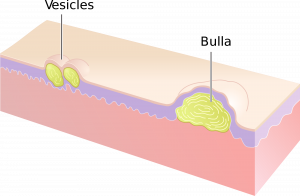
12.1.8 Vesicle:
small raised area of the skin, which is filled with serous fluid (clear); small blister
12.1.9 Blister:
elevation of the skin with serous fluid inside; often appearing in areas of wear and tear or in response to burns
12.1.10 Bulla:
a large blister, generally greater than 5-10 mm in diameter
12.1.11 Maceration:
softening and whitening of the skin as the result of wetness; often occurs with poor attention to people who are incontinent of urine and or stool
12.1.12 Pruritus:
itchiness
12.1.13 Urticaria:
hives; patches of red, raised, itchy bumps on skin

12.1.14 Ichthyosis:
extremely dry, scaly skin; most commonly used to describe a specific group of genetically-based skin disorders
12.1.15 Xeroderma:
condition of very dry skin; usually milder than ichthyosis
12.1.16 Telangiectasis:
visible, small, superficial veins seen in the skin; spider veins

12.1.17 Raynaud phenomenon:
decrease in circulation to the fingers or toes (rarely other parts of the body) causing blanching (whiteness) followed by redness as circulation returns; symptoms triggered by exposure to cold temperatures or emotional stress

12.1.18 Sclerodactyly:
localized thickening of the skin on the fingers and/or toes
12.1.19 Data Collection:
Inspection of the integumentary is always important in providing patient care in any setting. Skin integrity, color, and temperature can provide valuable information for the PT or PTA. It is essential that therapists recognize skin conditions and identify possible communicable conditions and those conditions that need to be referred to another health care professional.
The state of the integumentary system should be assessed in every patient. Obvious wounds, rashes, bumps, or other abnormalities of the skin should be observed and documented. Size, shape, color, depth in the case of a depression or wound, or height in the case of a raised area should be documented. Areas of redness or other discoloration or temperature change (too hot or too cold) should be noted. The skin should be assessed for intact or altered sensation, particularly if thermal modalities are considered. Other indications of integumentary issues that could be associated with other problems include lack of hair growth and lack of sweating, as the hair follicles and sweat glands can be damaged when skin is damaged.
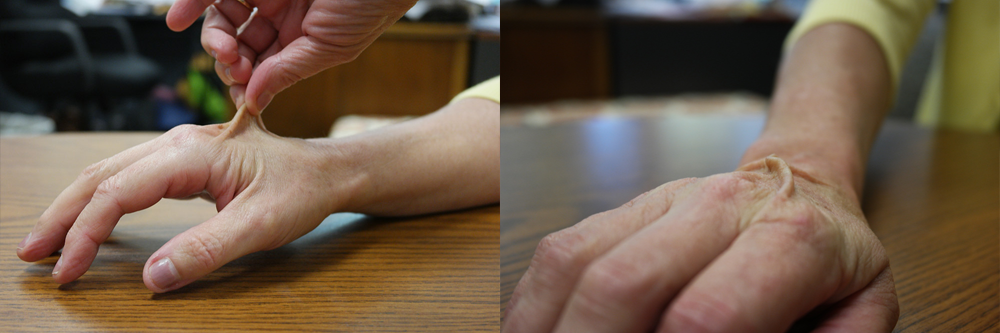
The test for skin turgor is often used to help determine possible dehydration in a patient. In this test, the skin on the forearm or dorsum of the hand is pulled outward, and then let go. Normally, the skin will immediately resume its normal appearance, but in the case of dehydration it will remain “tented,” requiring several seconds or longer to return to its flat appearance.
12.2 Aging skin
As skin ages, the composition changes so that the amount of elastin decreases, the collagen becomes weaker, subcutaneous fat diminishes, and fluid content of the skin decreases. These integumentary changes are responsible for characteristic wrinkling and sagging of older skin. They also cause the skin to be more easily broken, irritated, or sunburned. The effects of aging of the skin are exacerbated by exposure to sunlight and other forms of UV light, smoking, dehydration, exposure to low humidity, and some medications. With age, veins become more visible on the skin and bruises and wounds and abrasions are slower to heal.
For all the reasons mentioned above, the PTA must be cautious when with the skin of older individuals. Shearing forces associated with less-than-perfect transfers can easily damage dry, thin skin. If the patient is incontinent, maceration is likely to add to the problem and set up a perfect storm for sacral pressure ulcers. It is also very important to consider the condition of the skin when applying or removing tape or other adhesives. Skin should be checked regularly for signs of pressure or breakdown, especially in patients who are not independently mobile. Common areas for pressure include scapula, elbows, sacrum, ischial tuberosity, greater trochanter, malleoli, heels, and metatarsal heads. Orthotics and prosthetics can cause rubbing, and areas of skin contact with these devices should be checked frequently. Even the rubbing and pressure of elastic resistance can cause problems for older patients, so PTAs need to be aware of potential problems to avoid injuring fragile skin.
Some specific age-related changes to the skin are listed below:
12.2.1 Age spots/ liver spots (solar lentigo):

benign areas of increased pigmentation occurring in areas of sun exposure; result of skin’s inability to recover from UV light damage with age.
12.2.2 Seborrheic keratoses:
wart-like, raised, dark patches of skin; can occur in younger people, but more common in people over age 50; not problematic, but can be confused with or mask some skin cancers
12.2.3 Skin tags (acrochordons):

Small, benign growths, small excess skin patches that often form in areas of skin folds, where skin rubs other skin, such as armpits, neck, or groin
12.3 – Integumentary Conditions and Injuries
12.3.1 Noncommunicable Integumentary Conditions
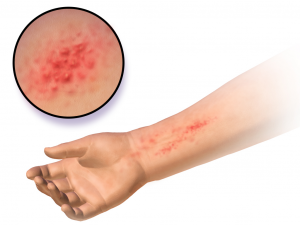
12.3.1.1 Atopic dermatitis
Atopic dermatitis is the most common form of eczema. It most often affects infants and young children but can affect any age group. It is a chronic condition, causing red, dry, itchy skin, most commonly on the cheeks, arms, and legs. It is often found as part of a cluster of symptoms with asthma and hay fever. The cause of atopic dermatitis is unknown. It is generally treated with over-the-counter moisturizing creams or steroidal applications in times of exacerbation. Infections can occur if the skin is broken, and antibiotics may be prescribed to treat possible infection.
12.3.1.2 Contact Allergic Dermatitis
Contact allergic dermatitis occurs in response to a hypersensitivity reaction to a substance. Allergies to antibiotics, latex, or poison ivy often result in contact allergic dermatitis, which can cause blistering of the skin and intense itching sensations. Why some people develop these allergies is unknown but presumed to be genetic. Contact allergic dermatitis is best treated with avoidance of the allergen. The rash caused by contact allergic dermatitis is treated symptomatically with calamine lotion, oatmeal baths, and sometimes steroidal creams. Overuse of topical steroid medications can cause thinning of the skin, so these are generally prescribed sparingly. Antibiotics may also be prescribed in the presence of open skin and suspicion of infection.
12.3.1.3 Eczema or Dermatitis

Eczema (dermatitis) is a group of inflammatory skin conditions, some of which are described below. The etiology of dermatitis is largely unknown, and treatments vary with the specific type of dermatitis.
12.3.1.4 Rosacea

Rosacea is a chronic condition found in middle-aged and older adults. It is more common in women than men, and there is no know cause. Symptoms include redness, enlarged superficial blood vessels and small pustules on the face. Symptoms can be exacerbated by exposure to sunlight, exposure to extreme temperatures, or moving from a cold environment to a warm one, such as coming in from the cold in winter. Emotional stress, anxiety, and strenuous exercise are also associated triggers.
Most people who have rosacea do not require medical intervention. Antibiotics, either topical or oral are used in more severe cases.
12.3.1.5 Psoriasis
Psoriasis is a chronic skin condition thought to be genetic in nature with triggers tied to stress, infection, skin injury, smoking, alcohol use, some drugs (many medications used in hypertension), and changes in weather. Autoimmune in nature, psoriasis causes T-cells to attack skin cells, causing an over-production of skin cells. This leads to the characteristic plaques and patches of red or purple, often with a coating of white or silvery scale. The fingernails and toenails are often affected, as well, with pitting and color change. Depending upon the type of psoriasis, skin lesions can occur on any part of the body.

The most common type (85-90%) of psoriasis is plaque psoriasis, which typically presents as plaques on the elbows, knees, scalp, and back. The plaques are red, dry, and itchy. Other, less common forms of psoriasis include pustular, inverse, napkin, guttate, oral, and seborrheic-like.
Arthritic psoriasis occurs in about 30% of people with psoriasis. The arthritis most often affects the joints of the fingers and toes and is usually not as severe as other forms of arthritis. The swelling in these joints can cause a sausage-like appearance of the associated digits.
Psoriasis increases the risk of developing other conditions including type 2 diabetes, cardiovascular disease, hypertension, metabolic syndrome, obesity, other autoimmune diseases, eye disorders, Parkinson disease, kidney disease, and emotional disorders.

The most common forms of medical intervention include topical moisturizers, steroidal applications, and U-V light therapy. Other interventions include Vit D cream and immunosuppressive medications (methotrexate). Lifestyle changes, such as smoking cessation, discontinuation of alcohol use, weight loss, avoidance and early treatment of infection, and stress-reduction may help decrease outbreaks of psoriatic plaques.
The most common forms of medical intervention include topical moisturizers, steroidal applications, and U-V light therapy. Other interventions include Vit D cream and immunosuppressive medications (methotrexate). Lifestyle changes, such as smoking cessation, discontinuation of alcohol use, weight loss, avoidance and early treatment of infection, and stress-reduction may help decrease outbreaks of psoriatic plaques.
12.3.1.6 Cellulitis and Erysipelas (Skin Infections)
Watch the YouTube video on Cellulitis and Erysipelas
12.03 – Resource 06 – “Bacterial Skin Infection – Cellulitis and Erysipelas (Clinical Presentation, Pathology, Treatment)” by Armando Hasudungan is licensed under Fair Use
After viewing the video, answer the following questions.
12.3.2 Communicable Integumentary Conditions
12.3.2.1 Fungal Infections: Parasites / Dermatophytosis / Tinea / Ringworm
Fungal infections can affect the skin in any part of the body. They are common in the population and they are named differently according to the type of parasite and the area infected. Some of the common infections are listed below. For all types, risk factors include: using public showers, walking barefoot, participation in contact sports, such as wrestling, sweating, obesity, and poorly functioning immune system.
Dermatophytosis, or ringworm, usually appears as one or more circular, raised red patch on the skin. The patch sometimes appears as a ring, with most of the redness on the outside of the circle. Oozing, blistering, and bald patches occur as the lesion progress. Finger- and toenails are common areas of infection, leaving them dry, brittle, often yellowish, and cracking
Ringworm can spread from person-to person through sharing of personal items, such as razors. Some forms can be passed from other animals to humans or vice versa. It can be managed through topical application of anti-fungal cream. In some cases, oral antifungal medications are used.
Tinea faciei: fungal infection of the face
Tinea pedis (athlete’s foot): fungal infection of the feet
Tinea unguium: fungal infection of the nails or nailbeds
Tinea corporis: fungal infection of the arms, legs, or trunk
Tinea cruris (jock itch): fungal infection of the groin area
Tinea manuum: fungal infection of the hands
Tinea capitis: fungal infection of the scalp
Tinea barbae: fungal infection of facial hair (beard area in men)
12.3.2.2 Herpes Simplex Types 1 and 2
Herpes is a virus that is found in many forms. Herpes simplex 1 generally presents as lesions on the face, head or neck, often around the mouth (cold sores), while herpes simplex 2 generally causes genital herpes. It is important to remember that either type can cause eruptions of lesions anywhere on the body.
Since herpes is a viral infection, it must invade a host to survive and replicate. An infected individual can spread the herpes virus to another person through physical contact or body fluid transmission. Even asymptomatic carriers can spread the virus. In fact, these are considered the most dangerous carriers because they are often unaware of their state of transmission. The herpes virus remains within the individual forever, lying in wait on the nerves near the site of the previous lesion. It can reemerge at any time, most often in times of stress, illness, or injury.
Prevention of herpes spread is accomplished through limiting close contact with infected individuals. Condoms are an effect barrier to the spread of genital herpes and most other sexually transmitted diseases. Antiviral medications are used to control outbreaks and decrease the likelihood of transmission. Topical anesthetic agents help control the pain and itchiness of the lesions. Analgesics, such as ibuprofen (Advil) can help relieve pain and fever.
Some specific types of herpes infections are listed below:
Herpetic gingivostomatitis: Infection of the inside of the mouth; often the first herpes infection; usually mild
Herpes labialis: infection of the lip; typical cold sore
Herpes genitalis: Infection of the genitals
Herpetic whitlow: Infection of the fingers
Herpes gladiatorum: infection of the face, ears, or neck (sometimes eyes) associated with contact sports, such as wrestling; fever, headache, sore throat, swollen glands common; sometimes called mat herpes
Herpesviral encephalitis and herpesviral meningitis: herpes infection thought to enter the brain through nasal cavity; can be fatal; uncommon
Herpes esophagitis: infection of the esophagus; difficulty swallowing; associated with HIV/AIDS and organ transplant
12.3.2.3 Impetigo

Impetigo is a bacterial infection of the integument, usually on the face, and sometimes on the arms or legs. It is most common in young children and can spread easily through schools, daycare centers, or any place where people are in close contact and share objects. Impetigo is characterized by blisters which get a yellowish crust. The blisters may be painful or itchy. Antibiotic creams or oral antibiotics are used to manage the condition. Handwashing and attention to appropriate hygiene are important to limit the spread of impetigo. Some forms of antibiotic-resistant impetigo have been recognized.
12.3.2.4 Pediculosis (Lice)

Pediculosis is a lice infection. Pediculosis capitis is head lice; pediculosis corpus is body lice; and pediculosis pubis is pubic lice, or crabs. All types are caused by an infectious ectoparasitic insect that can easily spread between people. Lice cause itching as they bite into skin to extract blood from the host. They do not burrow but remain outside the skin. In the case of head lice and crabs, the insects lay eggs (nits) on hair, which hatch into new lice, and the cycle continues. Body lice are a bit different in that they lay eggs on clothing rather than hair. Body lice are also considered the most dangerous form of lice, because they carry other diseases, such as typhus. Head lice and crabs are not known to carry other diseases.
Lice are a problem world-wide, and the numbers of infestations continue to grow. There is no absolute treatment for lice, although there are several effective chemicals available to help manage the condition. Special combs can be used to help remove the nits from hair. Shaving of hair can be an effective intervention.
12.3.2.5 Scabies
Scabies is a skin condition caused by a mite, Sarcoptes scabiei. It borrows under the skin, causing a rash and severe itchiness, which may be worse at night. The rash contains small vesicles, which may be in a line or burrow. Commonly affected areas are the fingers and toes (webspaces, typically), the wrists, and Scabies is often found in communal living areas, such as child care facilities, group homes, and prisons.
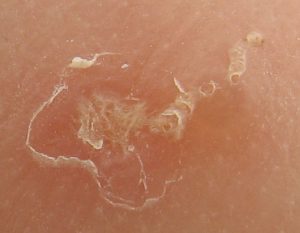
Symptoms can take up to 6 weeks to appear after infestation because the characteristic rash is an allergic reaction in the skin to the mite. Subsequent infections cause symptoms to occur in days, rather than weeks.s The mites can spread between people even before symptoms appear.
Scabies are treated with several different specific anti-insecticide medications. The infected individual, anyone living with the individual and recent sexual partners should all be treated. Bedding, clothing, and towels used in the last 3 days should be washed in hot water and dried in a hot dryer. Since the scabies mite can only live outside of the body for 3 days, only items used in that time period need to be treated. Antihistamines and anti-inflammatory medications are used to help control the itchiness.
12.3.3 Skin Conditions Associated With Other Conditions
12.3.3.1 Discoid lupus erythematosus
Discoid lupus erythematosus is the most common form of chronic cutaneous lupus, which is a group of autoimmune skin disorders. This disorder should not be confused with systemic lupus erythematosus (SLE), which affects internal organs and joints. It is not uncommon for people who have SLE to develop discoid lupus lesions, but it is uncommon for people with discoid lupus to develop SLE.
Discoid lupus erythematosus causes skin lesions to develop on the scalp, face, or neck, and rarely elsewhere in the body. The initial lesions are raised, firm, and usually red or purplish in color. They become scaly and oozing and result in scarring, which can be significant. Skin color changes can also occur, most often white skin turning graying, and darker skin becoming lighter. Baldness is also a complication in some people with discoid lupus. Exposure to sunlight (UV light) and smoking are associated risk factors for lesion development.
People with discoid lupus are advised to avoid UV light exposure, always wear sunscreen, and avoid smoking. Topical and injected steroids are used to diminish the skin thickening and scarring. Immunosuppressive medications, antimalarial medications, and retinoids are also used in the management of the disorder.
12.3.3.2 Varicella zoster virus/ Herpes zoster (Shingles)
Herpes zoster (VZV) is a virus that causes chicken pox then remains dormant on the nerve roots. Many years later, it can reemerge as shingles. This latent form of the virus causes symptoms along nerve roots on the face, trunk, or extremities. Pain and burning sensations along a nerve distribution on one side of the face or body may be the first symptoms, followed by vesicle eruption in the same area a few days later. Fever, chills, headache, or gastrointestinal upset may also be present for a few days. The vesicles scab over in 7-10 days and disappear in 2-4 weeks. Residual nerve pain, called postherpetic neuralgia (PHN), may persist, for months or years following the outbreak. Other complications of VZV include: pneumonia, hearing loss, encephalitis, and death. Vision loss can also occur if the area of involvement includes the eye. All of these complications are rare.
Advancing age is a major risk factor for shingles. Other risk factors include any condition that causes decreased immune function: HIV, organ transplant, other autoimmune disease, or anyone taking immunosuppressive medications for any reason. Most research shows a predominance in the number of women affected over men, and the number of Caucasians affected over African-Americans.
Although shingles cannot be directly transmitted from person to person, someone with active shingles’ vesicles that are open or oozing can transmit VZV to a person who has no immunity to the virus, either through vaccination or by previously having the disease. The newly infected person would get chicken pox, and therefore, be at risk for developing shingles.
Antiviral medications, such as acyclovir, valacyclovir, and famciclovir are used to shorten the duration of, and decrease the pain during, the outbreak. Antiviral medications need to be started early in the course of the outbreak to be most effective. Over-the-counter pain relievers can be used for pain, and calamine lotion and oatmeal baths can be used for the itching associated with a VZV outbreak. For patients with significant PHN, prescription pain medications can be useful, but these need to be prescribed with caution to avoid dependency and addiction.

Most people who experience an outbreak of shingles will not experience another. Some people do experience two or more outbreaks.
Anyone who has had chicken pox or received the vaccine for chicken pox is at risk for developing shingles. Two different shingles vaccines are available, Shingrix and Vostivax. Shingrix is regarded as most effective. Vaccines are recommended for everyone over the age of 50. (CDC Wikipedia page for Discoid lupus erythematosus)
| Category | Content |
|---|---|
| Description |
English: John Pozniak, with zoster blisters on his neck and shoulder. Taken May 5, 2006, in San Jose, California, United States. Copyright © 2006, John Pozniak, and released under the terms of the GNU Free Documentation License ver. 1.2 or any later version.
|
| Date | 6 May 2006 (original upload date) |
| Source | No machine-readable source provided. Own work assumed (based on copyright claims). |
| Author | No machine-readable author provided. Gentgeen assumed (based on copyright claims). |
12.3.3.3 Scleroderma
Scleroderma is divided into two main categories: localized and systemic. Both are autoimmune disorders of the connective tissue, and both affect the skin. Localized scleroderma or limited cutaneous systemic sclerosis, affects the skin only of the face, hands, and feet. Systemic scleroderma (also called diffuse scleroderma or systemic sclerosis) affects the skin and internal organs, such as the kidneys, heart, lungs, and GI tract. Systemic scleroderma is much more serious than localized scleroderma, with about half of all patients succumbing to organ failure within 10 years of diagnosis.
The skin becomes thick, hard, inflexible, and scarred in either form of scleroderma. Muscle weakness and wasting occurs in areas of involvement, commonly the hands, feet, face and neck. Severe itching is also common in areas of involvement. Scleroderma is associated with CREST syndrome (calcinosis (formation of calcium deposits in soft tissue), Raynaud’s phenomenon, esophageal dysfunction, sclerodactyly, and telangiectasis). Involvement of the esophagus can lead to swallowing difficulties, and as internal organs become involved, functions associated with those organs can be affected. Ulcerations can occur, most often in the hands, which can lead to open, infected wounds.
The basis of scleroderma is unclear, but genetic predisposition is suspected. Exposure to certain viruses (CMV) as a trigger is an area of research for scleroderma. Women are affected more often than men. Most people develop scleroderma between the ages of 30 and 50. There is no cure for the condition, but topic and oral medications are used to alleviate symptoms and soften the skin, primarily steroids. NSAIDs can be used to decrease pain. Immunosuppressive medications, such as methotrexate, can be prescribed to slow the disease process. If other organs are involved in systemic scleroderma, additional medications and interventions can be employed in accordance with the specific problems seen as organ function diminishes.
Watch this video for more information on CREST and limited cutaneous systemic sclerosis.
12.03 – Resource 12 – “CREST syndrome – causes, symptoms, diagnosis, treatment, pathology” by Osmosis is licensed under Fair Use
12.3.3.4 – Systemic Lupus Erythematosis
12.3.4 Thermal injuries, including frostbite and burns
Watch the following video on thermal injuries (burns). This video is designed for medical students, so it has some information (medical interventions) that is beyond the expected knowledge of the PTA. Most of the information IS appropriate for the PTA, and the medical interventions addressed for med students are a minor part of the video.
https://www.osmosis.org/learn/Burns:_Clinical_sciences
12.03 – Resource 13 – “Burns” by Osmosis is licensed under Fair Use
Please note that extreme cold can cause frostbite, which affects the integumentary system in essentially the same manner as does extreme heat.
Review the following to learn more about the various types of burns. Visit this Wikipedia page to view detailed information and a table of burns.
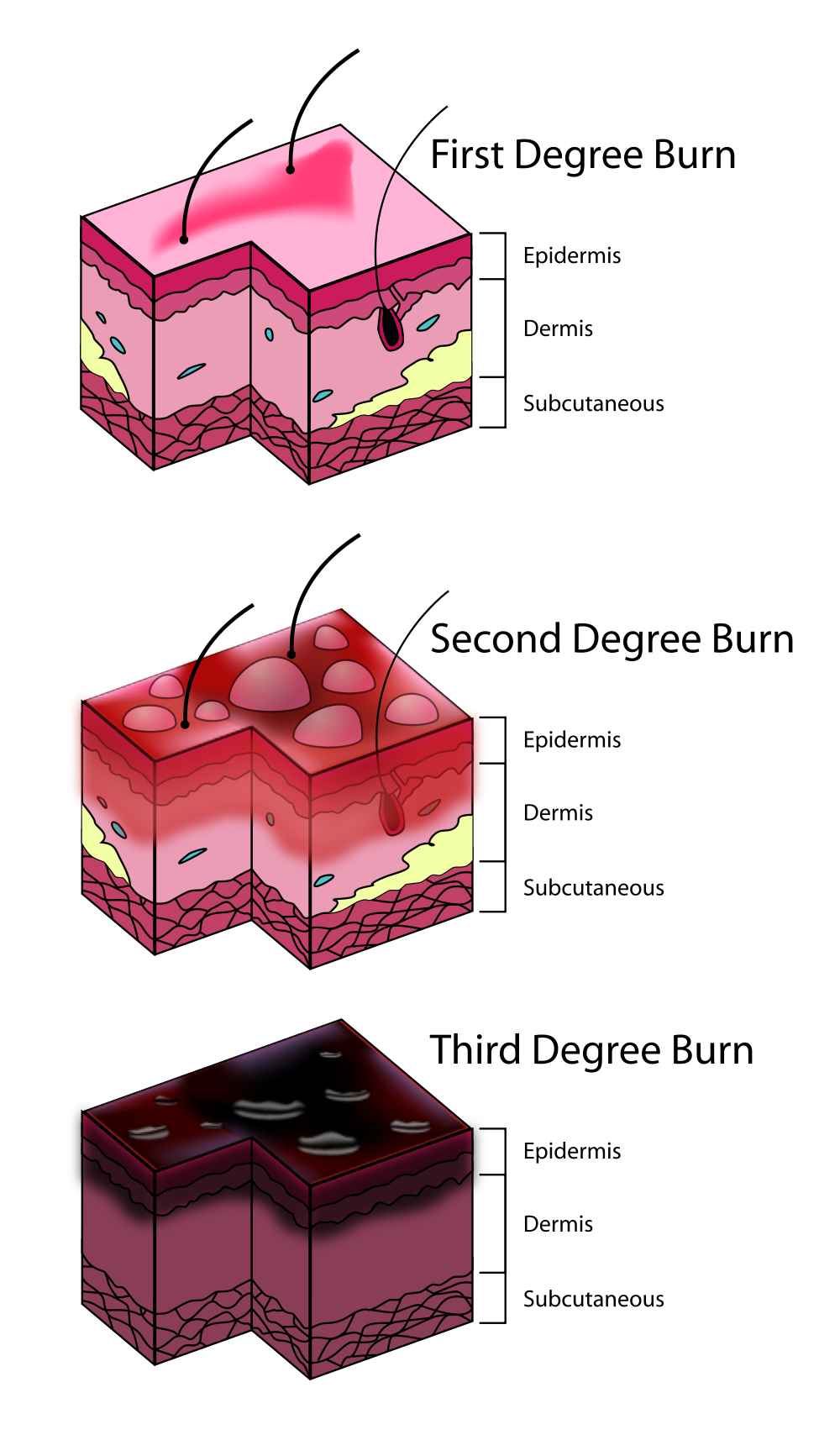
12.3.4.1 Superficial (first-degree)

Wikipedia page on burns.
12.3.4.2 Superficial partial thickness (second-degree)

Second-degree burn of the thumb
12.3.4.3 Deep partial thickness (second-degree)

12.3.4.4 Full thickness (third-degree)

12.3.4.5 Fourth-degree

12.03 – Resource 17 –
| Type[2] | Layers involved | Appearance | Texture | Sensation | Healing Time | Prognosis and Complications | Example |
|---|---|---|---|---|---|---|---|
| Superficial (first-degree) | Epidermis[10] | Red without blisters[2] | Dry | Painful[2] | 5–10 days[2][20] | Heals well.[2] Repeated sunburns increase the risk of skin cancer later in life. [21] |
 |
| Superficial partial thickness (second-degree) | Extends into superficial (papillary) dermis[2] | Redness with clear blister.[2] Blanches with pressure.[2] | Moist[2] | Very painful[2] | 2–3 weeks[2][15] | Local infection (cellulitis) but no scarring typically[15] |  |
| Deep partial thickness (second-degree) | Extends into deep (reticular) dermis[2] | Yellow or white. Less blanching. May be blistering.[2] | Fairly dry[15] | Pressure and discomfort[15] | 3–8 weeks[2] | Scarring, contractures (may require excision and skin grafting)[15] |  |
| Full thickness (third-degree) | Extends through entire dermis[2] | Stiff and white/brown.[2] No blanching.[15] | Leathery[2] | Painless[2] | Prolonged (months) and unfinished/incomplete[2] | Scarring, contractures, amputation (early excision recommended)[15] |  |
| Fourth-degree | Extends through entire skin, and into underlying fat, muscle and bone[2] | Black; charred with eschar | Dry | Painless | Does not heal; Requires excision[2] | Amputation, significant functional impairment and, in some cases, death.[2] |  |
Answer the following questions regarding thermal injuries:
12.3.5 Tissue Injuries
12.3.5.1 Vascular Conditions and Ulcerations
Abnormalities in the arteries and veins can cause problems for the skin, particularly in the lower extremities. Peripheral vascular disease (PVD), which includes both venous and arterial insufficiencies, can lead to ulcerations in the lower extremities, which put a person at risk for infection and even amputation. The differences between venous and arterial insufficiencies are important, as their appearances, etiologies, and treatments are very different.
12.3.5.2 Peripheral Venous Insufficiency (PVI)

Since the veins are responsible for carrying blood from the extremities back to the heart, any problems with venous return results in pooling of blood in the feet and ankles. Risk factors for developing venous insufficiency include: damaged valves in the veins or thrombus formation within a vein can prevent blood from passing through and returning to the heart. Deep venous thrombosis, superficial venous thrombosis, phlebitis, and varicose veins are risk factors for developing PVI. Poorly functioning valves or the formation of clots in the veins cause pooling of blood and fluid retention in the legs and feet. This manifests as increased pigmentation (darkening) of the skin). Eventually, the condition can be come chronic (chronic venous insufficiency). The lack of blood flow in the veins is termed venous stasis, and ulcerations called venous stasis ulcer can appear as shallow, irregularly shaped ulcerations in the lower legs and feet. The dorsal pedal and tibial pulses should be palpable in the case of venous insufficiency, as the pulses are palpated over the arteries, not the veins. The tissues remain oxygenated, as well, because arterial blood continues to flow to the area.

Venous ulcers in the legs can be dangerous, as they can become infected and lead to cellulitis, ostemyelilitis, and malignant changes.
Most ulcers associated with PVI can be treated with patient education, lower extremity elevation and compression. Compression bandaging is used to help reduce fluid retention and help blood return to the heart and lymph move to the trunk. Lower extremity elevation (above the level of the heart) is recommended to help alleviate swelling in the feet and legs. It is important to keep the area clean and lubricated, as the skin can be dry and inelastic and the wounds are at risk for infection. Various wound coverings and topical ointments are available for use in healing ulcers. Medications used to treat venous stasis include: pentoxifylline and aspirin. In some cases, surgery might be warranted to remove or close insufficient veins that are prone to clotting or to stent some larger veins to improve blood flow. Evidence for surgery over conservative treatment is lacking. Recurrence of venous stasis ulcers is common.
(Source: LAUREN COLLINS, MD, and SAMINA SERAJ, MD,Diagnosis and Treatment of Venous Ulcers Am Fam Physician. 2010 Apr 15;81(8):989-996. American Family Physician: Diagnosis and Treatment of Venous Ulcers)
12.3.5.3 Peripheral Artery Disease (PAD)
Smoking, diabetes, hypertension, and high cholesterol are known risk factors for PAD. All cause damage to blood vessels, which allows atherosclerotic plaques to form in the vessels. If the arteries are clogged and are not able to supply oxygenated blood to distal extremities, tissues in this area can become ischemic, and eventually, necrotic. The dorsal pedal and tibial pulses will be weak or absent and the skin will be pale, cold, and often hairless. Skin ulcerations that develop in the presence of PAD are circular, red, and deep. Intermittent claudication occurs, and as the condition worsens, pain is present even at rest and severe paresthesia can develop. Since the tissues in the extremity are lacking oxygen, wounds do not heal well and any injury to the skin is dangerous and may result in amputation. Ulcers resulting from PAD are less common than venous stasis ulcers. Because of the deoxygenated condition of the tissues in PAD, the resulting ulcers are much more dangerous and result in amputation much more often than those from PVI.
While treatment for venous insufficiency includes elevation of the legs to allow gravity to assist with blood flow return, in PAD, elevation of the legs actually increases pain and impedes blood flow down the legs, so lower extremity elevation is contraindicated in these patients. Instead, patients with PAD should be encouraged to rest with the legs hanging or dangling, allowing gravity to assist in blood flow down to the toes. Exercise is important any type of vascular disease, both as prevention and treatment, to improve circulation through the lower extremities. Medications for arterial insufficiency include blood thinners and anticoagulants (aspirin, Plavix) and cholesterol lowering drugs (statins). It is important to keep the wound clean to prevent infection and treat any signs of infection immediately. Debridement is an important component of wound care for ulcers associated with PAD. Necrotic tissue needs to be removed so that healthy granulation tissue can grow. Fluid balance needs to be maintained by the application of wet dressings to dry tissue, and dry dressings to wet tissue. Some important dressings used in wound care include: films, hydrocolloids, hydrogel dressings, foam, hydrofibers, composite dressings and alginate dressings. Daily inspection of feet, proper shoe wear, and professional toenail care are essential in the presence of PAD.

Angioplasty, either with balloon or stenting can be used to open the blood vessel. A surgical bypass graft can be done to re-route blood around a clotted area. An endarterectomy is also an option, where the vessel is surgically opened, and the blockage removed.
For a quick review of PVD, PAD, and PVI (be careful, the presenter often says PVD when he means PVI), watch this nursing video.
12.3.5.4 Pressure Injury
Pressure injuries (pressure sores, pressure ulcers, decubitus ulcers, bed sores) can occur anywhere in the body where pressure from outside the body meets pressure from inside the body. The sacrum, greater trochanter of the femur, malleoli, metatarsal heads, calcanei, scapular spines, and elbows are common places for pressure injuries to occur. When the skin is compressed between a bony area and an external surface, such as a bed, chair, or orthotic, the capillaries supplying the tissues with oxygen are crushed, and the skin cells die. Deep, cone-shaped, necrotic wounds can be the result. Lack of mobility, incontinence, decreased sensation, cognitive impairment, thinning skin, and compromised blood flow are risk factors. The frail elderly population is at particular risk, but other high-risk populations include those people with spinal cord injury, stroke, spina bifida, cerebral palsy, muscular dystrophy, and other neuro-muscular conditions.
Prevention of pressure injury is very important. PTs and PTAs need to be aware of, and assist with, frequent position changes for patients. They should inspect the feet and other areas associated with pressure or wear and tear every time they see a patient at risk for pressure injury. They should check for areas of wetness, such as incontinence issues, and see that the patient’s skin is not subject to maceration.
Once a wound has developed, PTs and PTAs could be involved in wound care including debridement and dressing changes. As described earlier, films, hydrocolloids, hydrogel dressings, foam, hydrofibers, composite dressings and alginate dressings can be used to assist in wound healing. PTAs are able to assist in wound care but are not allowed to perform selected sharp debridement. (APTA PDF)
More information on pressure injuries can also be found in the chapter on Injury, Inflammation, and Repair.
12.3.5.5 Wound Care
Any wound on the skin is a potential infection risk and should be monitored and treated immediately if signs and symptoms of infection or other complications arise. Many people die because of pressure injuries, mostly due to renal failure or amyloidosis. Read the short article on the NIH site on wound pressure injury management. Wound Pressure Injury Management
(Ahmad M. Al Aboud; Biagio Manna. Wound Pressure Injury Management. Copyright © 2019, StatPearls Publishing LLC.
This book is distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-NC-ND 4.0), which permits use, duplication, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, a link is provided to the Creative Commons license, and any changes made are indicated.)
Bookshelf ID: NBK532897PMID: 30422492)
12.3.5.6 Viable and Nonviable Tissue
When a wound occurs, frequent (most often, daily) assessment of the wound is recommended. The condition of the wound and the surrounding area are important to note and document. Infection and other complications can develop quickly and prompt attention to possible complications is important for the PTA and other health care workers.
Several types of tissue can be seen in wounds. These types are often divided into viable and nonviable tissue.
12.3.5.7 Viable tissue includes:
Granulation tissue: bright red, beefy tissue that is highly vascular and moist
Epithelial tissue: new growth around the edges of a wound. It usually appears pinkish or purplish. It sometimes develops as “islands” within a large wound.
Muscle: appears red or pink and smooth. Striations are sometimes noticeable.
Tendons or ligaments: appear white or light yellow when healthy
Bone: milky white, smooth, and often glistening, when healthy
12.3.5.8 Nonviable tissue includes:
Eschar, or necrotic eschar: black and dry tissue
Fibrinous slough: yellow or green moist tissue
12.3.5.9 Scarring Complications
Scars develop on wounds in relation to the size, location, and severity of the wound. A car develops when normal tissue that has been destroyed is replaced by fibrinous tissue, inelastic tissue. Larger and/or deeper wounds that heal by 2nd intention or tertiary intention (see Injury, Inflammation, and Healing chapter) will scar because of the significant amount of fibrin and collagen laid down in the healing process. Wounds that are on body surfaces subject to wear and tear, or irritation, are more likely to scar. Wounds that have been subject to other complications, such as infection or ischemia, are more likely to heal slowly and develop scar tissue.

Keloid scarring occurs in some individuals. These large, raised scars are due to a genetic predisposition, rather than the condition of the wound. Hypertrophic scarring, which is also raised and red or brown, are due to excessive collagen formation in the scar. The risk factors for hypertrophic scarring are genetics and mechanical tension (pulling on the healing wound).

12.3.5.10 Goals of wound care
The goals of wound care include achieving or maintaining a clean wound that allows for healing, promoting healing of the wound, and promoting optimal function for the individual with the wound. Prevention of complications including infection, adhesions, excessive scar formation, and scar immobility is important to goal attainment. The prevention of wounds, such as pressure ulcers is also essential in caring for all patients, especially when mobility is limited, and sensation is decreased.
12.3.5.11 PTA Role in Wound Care
The PTA can play an important role in the prevention and treatment of wounds. Patient education regarding preventative measures including foot inspection, proper footwear, positioning and weight-shifting, and appropriate transfer techniques can be helpful in patients at risk for pressure injury. PTAs can participate in all aspects of wound care, except for selected sharp debridement, using scissors, scalpel or scissors. PTAs and PTA students are encouraged to check with state practice acts for further information regarding allowable treatment interventions for PTAs in their particular state.
12.3.6 Skin Cancer
There are three main types of skin cancer:
- Basal cell carcinoma (BCC)
- Squamous cell carcinoma (SCC)
- Melanoma
Watch the Osmosis video on these 3 types of skin cancer and answer the questions that follow.
12.03 – Resource 26 – “Skin cancers” by Osmosis is licensed under Fair Use
The Integumentary System Resources:
Resource 06 – “Bacterial Skin Infection – Cellulitis and Erysipelas (Clinical Presentation, Pathology, Treatment)” by Armando Hasudungan is licensed under Fair Use
Resource 07 – A case of childhood impetigo in a typical location around the mouth – “File:OSC Microbio 21 02 impetigo.jpg”, CNX OpenStax is licensed under CC BY 4.0
Resource 08 – Pediculus humanus var capitis AKA head louse – “File:Pediculus humanus var capitis.jpg” by the Centers for Disease Control and Prevention is in the Public Domain
Resource 09 – Scabies, showing burrow. Mite is at the end of the burrow in the upper right hand corner. – “File:Scabies-burrow.jpg” by Michael Geary is in the Public Domain
Resource 10 – Discoid lupus erythematosus – “Discoid lupus erythematosus” by Eva Rinaldi is licensed under CC BY-SA 2.0
Resource 11 –“File:Herpes zoster neck.png” by Gentgeen is licensed under CC BY-SA 3.0
Resource 12 – “CREST syndrome – causes, symptoms, diagnosis, treatment, pathology” by Osmosis is licensed under Fair Use
Resource 14 – “File:Sunburn.jpg” by QuinnHK is in the Public Domain
Resource 15 – “File:Scaldburn.jpg” by Snickerdo is licensed under CC BY-SA 3.0
Resource 16 – “File:Major-2nd-degree-burn.jpg” by User:Westchaser is in the Public Domain
Resource 17 – “File:8-day-old-3rd-degree-burn.jpg” by Craig0927 is in the Public Domain
Resource 18- “4th-degree burn – File:Ожог кисть.jpg” by goga312 is licensed under CC BY-SA 3.0
Resource 19 – “File:Burn Degree Diagram.svg” by K. Aainsqatsi is licensed under CC BY-SA 3.0
Resource 20 – “File:513 Degree of burns.jpg” by OpenStax College is licensed under CC BY 3.0
Resource 21 – “File:VenousInsufficiency-left-a.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0
Resource 22 – “File:Chronicvenousinsufficiency.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0
Resource 23 – “File:Arterial ulcer peripheral vascular disease.jpg” by Jonathan Moore is licensed under CC BY 3.0
Resource 24 – “File:Keloid, Post Surgical.JPG” by Htirgan is licensed under CC BY-SA 3.0
Resource 25 – “File:Hypertrophic scar -4 months after incident- 2013-04-05 00-46.jpg” by User:Cgomez447 is licensed under CC BY-SA 3.0
Resource 26 – “Skin cancers” by Osmosis is licensed under Fair Use

