Chapter 17: The Digestive System
Learning Objectives
After completing this chapter, the learner should be able to:
- Define the basic terminology associated with conditions of the digestive system.
- Discuss basic medical diagnosis of digestive disorders.
- List some common signs and symptoms of digestive conditions.
- Discuss risk factors, etiologic factors, pathogenesis, and clinical manifestations for the following digestive conditions:
- GERD
- Ulcerative conditions
- Pancreatitis
- Peritonitis
- Appendicitis
- Inflammatory bowel conditions
- Diverticular conditions
- Obstructive conditions
- Hernia
- Describe medical, surgical and physical therapy interventions associated with digestive conditions.
- Describe the pharmacological management of digestive conditions.
- Discuss precautions, indications and contraindications to be considered in physical therapy interventions for patients with digestive conditions.
- Recognize the signs and symptoms of acute digestive conditions and discuss appropriate course of action.
Chapter Contents
17.0 The Digestive System
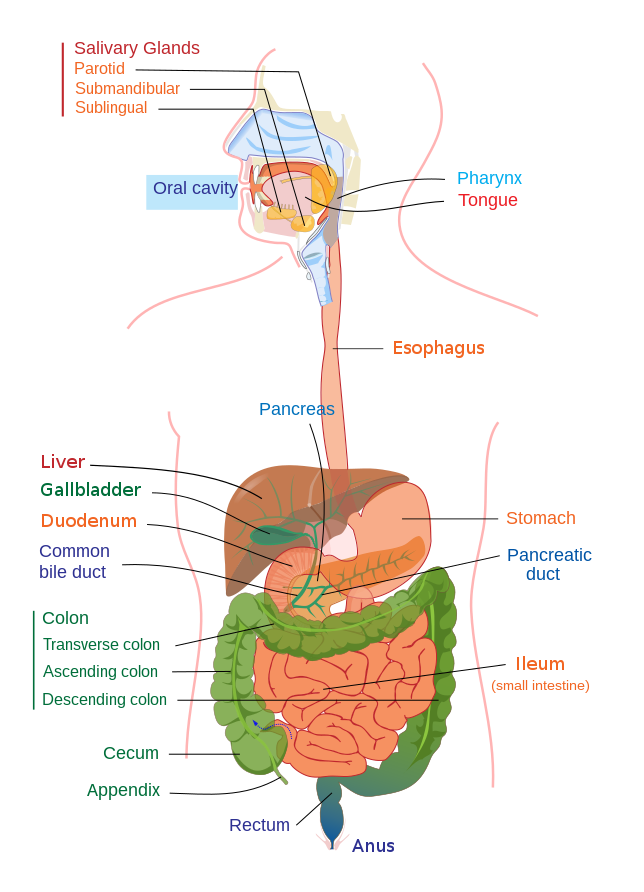
The digestive system includes all structures and organs associated with digestion from the mouth to the anus. Autonomic muscle control (peristalsis) is used to move food and waste products along the tract. Several structures produce substances that aid in the digestion of food and the extraction of nutrients.The focus of this chapter will be to discuss some of the conditions of the digestive system that PTAs are most likely to encounter in their work with patients. Particular attention will be paid to the gastrointestinal system and associated conditions.
Wikipedia page: Gastrointestinal tract
Long Description
Title: The Digestive System
An illustration shows the internal organs of the digestive system. The following organs are labelled.
- Salivary Glands
- Parotid
- Submandibular
- Sublingual
- Oral cavity
- Pharynx
- Tongue
- Esophagus
- Pancreas
- Liver
- Gallbladder
- Duodenum
- Common bile duct
- Colon
- Transverse colon
- Ascending colon
- Descending colon
- Cecum
- Appendix
- Stomach
- Pancreatic duct
- Ileum (small intestine)
- Cecum
- Appendix
- Rectum
- Anus
17.1 Gastrointestinal (GI) Disorders
General signs and symptoms of GI disorders include abdominal or chest pain, heart burn, bloating, nausea, vomiting, change in bowel habits, and hematochezia (blood in stool) and hematemesis (vomiting blood).
Digestive disorders can be diagnosed through various means. Signs and symptoms and physical exam are often quite telling of conditions related to digestion. Pain, area of pain, type of pain, presence of vomiting , and bowel habits and consistency are usually the first clues in the diagnosis of conditions. Further investigation could be in the form of x-ray or CT scan (static or dynamic, with or without contrast dye), MRI, upper endoscopy, colonoscopy, laboratory studies, or biopsy. Sometimes, several diagnostic tests are necessary before diagnosis can be achieved.
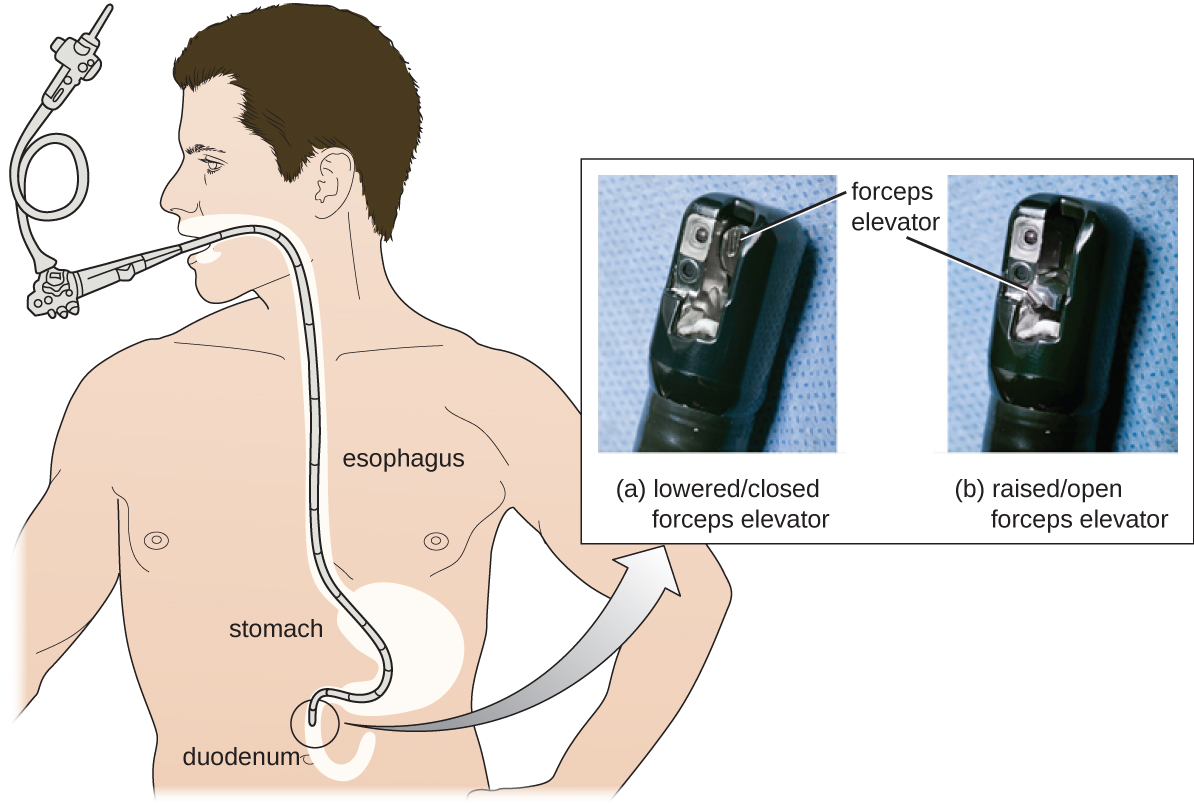
Wikipedia page: Esophagogastroduodenoscopy
Long Description
Title: DuoScope
Illustration shows a duodenoscope tube inserted into a patient’s mouth all the way down through the stomach to their duodenum. An inset photo shows the end of the scope with the forceps and elevator labelled closed and open.
17.1.1 Gastroesophogeal Reflux Disease (GERD)
GERD is a condition in which the stomach contents back-up into the esophagus. A weak esophageal sphincter is the most common cause of the disorder. It is also associated with obesity, pregnancy, hiatial hernia, and smoking. Typical signs and symptoms are include:
- Heartburn
- Bad breath, bad taste in the mouth
- Chest pain
- Vomiting
- Breathing difficulties
- Wearing away of enamel on teeth
Specific recommendations for lifestyle changes that help manage the condition include refraining from lying down for 3 hours after eating, avoiding irritating foods, losing weight, if necessary, and avoiding smoke, including second-hand smoke. Medications can be helpful in the management of GERD. Other lifestyle changes that can help include: avoiding overeating, sleeping with the head of the bed elevated, and not wearing clothing that is tight around the abdomen. Some specific medications used are proton pump inhibitors and H2 blockers to decrease acid production in the stomach, antacids to counteract stomach acid, and prokinetics, and erythromysin to help empty the stomach faster. In some cases, surgery is recommended to tighten the esophageal sphincter.
17.1.2 Peptic Ulcer Disease
Peptic ulcer disease results in the break in the inner lining of the stomach, duodenum, small intestine, or esophagus. It is most often caused by infection by the Heliobacter pylori bacterium, and is also associated with the use of many non-steroidal anti-inflammatory drugs (NSAIDS), such as aspirin, motrin, and Advil. Other risk factors include smoking, Crohn’s disease and hepatic disorders. People who have peptic ulcer disease often complain of abdominal pain, which can be a burning pain, bloating, vomiting, belching, weight loss, and poor appetite. As the disease progressed, perforation of the stomach lining and GI bleeding may occur. These are dangerous complications which require prompt medical attention.
In terms of treatment, first, a patient is required to stop taking any NSAIDs and stop smoking. A course of antibiotics can be use to treat the H. pylori bacteria, if present. For bleeding ulcers, more aggressive measures may need to be taken, including blood transfusions, cauterization, endoclip placement, and epinephrine injections.
17.1.3 Pancreatitis
Inflamation of the pancreas can be caused by several associated conditions or disorders. Cholelithiasis(gallstones) is one of the most common causes of pancreatitis. The gallstones are released from the gallbladderinto the common bile duct. From there, they can travel to the pancreatic duct, where they can become lodged. If the gallstones block the pancreatic duct, the result is pancreatitis. Alcohol abuse, cystic fibrosis, and trauma can affect the pancreas and cause it to become inflamed, as well. Nutritional or metabolic disorders such as hypercalcemia, hyperlipidemia, and hypertriglyceremia are also associated with pancreatitis. Heredity also plays a role in some forms of pancreatitis.
The signs and symptoms of pancreatitis include pain in the upper abdomen, which can be severe, nausea, and vomiting. In acute pancreatitis, fever is present. In chronic pancreatitis, weight loss, fatty stool, and diarrhea may occur.
Pancreatitis is usually diagnosed through blood tests, as the enzymes, amylase and lipase, are high acute pancreatitis. In chronic disease, these enzymes may be at normal levels and ultrasound or CT scan is often the best diagnostic tool.
In pancreatitis, strong digestive enzymes are released into the pancreas. These enzymes cause the inflammation. The condition can be either chronic or acute and can lead to the development of diabetes if insulin production is affected.
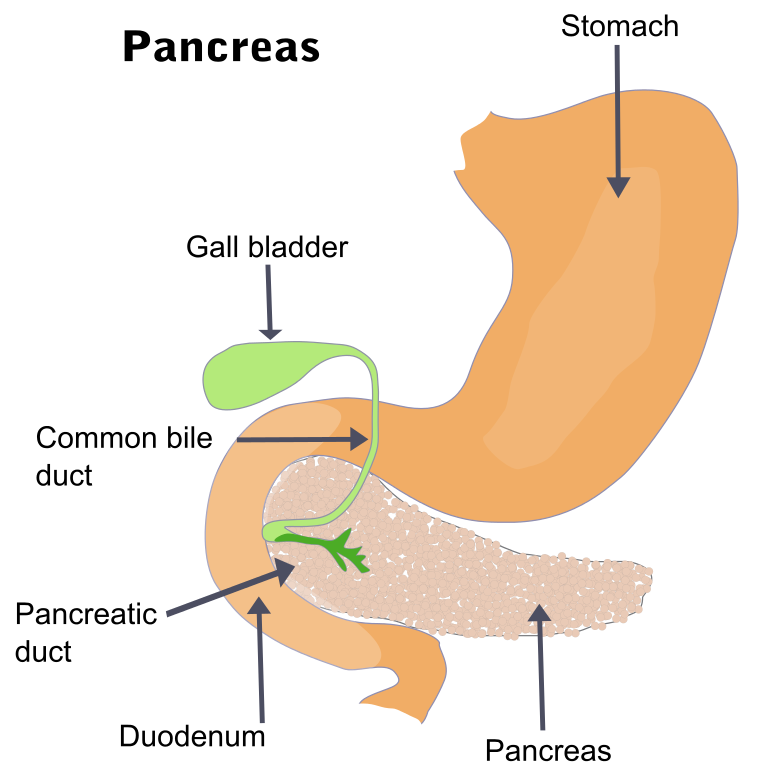
Wikipedia page: Pancreatitis
Treatment for pancreatitis is dependent upon the cause. Mild, acute pancreatitis is often treated with nasogastric tube feeding and the administration of oxygen. Dehydration is a concern, so the administration of IV fluids is prudent. If gallstones are the cause of the pancreatitis, surgery to remove the gallbladder is most often the intervention of choice.
Severe, acute pancreatitis can be very serious, causing organ failure and necrosis. Feeding tubes, breathing tubes, and IV fluids are all necessary, and treatment occurs in an intensive care unit with constant monitoring of vital signs. A major concern is hypovolemic shock, in which fluid levels and the volume of blood available to supply vital organs can drop dangerously low. The gallbladder will need to be removed if gallstones are the precipitating factor.
If chronic alcoholism is associated with either acute or chronic pancreatitis, all drinking of alcoholic beverages should cease. Even if alcoholism is not the cause, it is generally recommended that a person who has experienced pancreatitis refrain from alcohol consumption for at least 6 months following the episode of pancreatitis.
17.1.4 Peritonitis
Peritonitis refers to inflammation of the peritoneum, which can occur for a number of reasons. Infectious agents including bacteria, viruses, fungi, and other pathogens can attack the peritoneum, either as a primary site or as a secondary site associated with infections in other areas of the body. Perforation of the large or small bowel, appendix, stomach, or other abdominal organ can cause peritonitis. Other etiologies include ruptured appendix, cirrhosis of the liver, pancreatitis, and ascities. People who have kidney dysfunction and undergo daily peritoneal dialysis are also at risk for peritonitis.
Signs and symptoms of peritonitis include severe abdominal pain, fever, and abdominal swelling. Diagnosis is generally based on physical examination, blood tests, and diagnostic imaging.
A major issue with peritonitis is that the peritoneum is dispersed throughout the abdominal cavity, so the infected area is widespread. Major concerns for complications include shock and respiratory distress syndrome. When a person is diagnosed with peritonitis, they will most likely be admitted to ICU care for IV antibiotic treatment. Surgery is an option for some patients.
17.1.5 Appendicitis
The appendix is a small pouch-like sac attached to the large intestine in the lower right side of the abdomen. It can become blocked by mucous or stool, and bacteria inside the appendix multiply and cause it to become inflamed. This is an appendicitis, which most often causes pain and tenderness in the lower right quadrant of the abdomen. Other signs and symptoms include loss of appetite, nausea, and vomiting. If the appendix continues to expand with bacteria, it can lead to rupture and peritonitis. If a patient has an appendicitis, the treatment of choice is surgery as quickly as possible to remove the appendix before it causes further damage.
17.1.6 Inflammatory Bowel Conditions
Inflammatory bowel disease (IBD) is generally divided into two major types: Crohn Disease and ulcerative colitis. Both conditions are chronic irritations of the lining of the digestive tract which are diagnosed via colonoscopy or sigmoidoscopy, diagnostic imaging and biopsy. Signs and symptoms are similar for the two conditions, including abdominal pain, diarrhea, nausea, bowel urgency, fatigue, weight loss, and anemia. Both are managed through medication and dietary changes, Periods of remission are likely. Neither condition is curable. A comparison between the two disorder is summarized below.
Although neither diagnosis has as definitive etiology, both Crohn Disease and ulcerative colitis are believed to be cause by a combination of environmental, immune, and bacterial factors that affect people with a susceptibility to the condition. Smokers are more than twice as likely to have Crohn disease than nonsmokers. The risk factors for developing ulcerative colitis include positive family history, Jewish descent, being between the ages of 15 and 30, or older than 60 years.
17.1.6.1 Crohn Disease
- Inflammation occurs in patches all along intestine
- Affects any part of GI tract: esophagus to anus
- Blood and mucous LESS common in stool
- Nausea and vomiting MORE common
- Inflammation in mucosa and muscle tissue; Granulomas present
- Fistulas and strictures MORE common
- More common in smokers
- Treated with steroids, immunosuppressive medications, biologics; 5-ASAs (Aminoscicylates) NOT usually effective
- Surgery usually does NOT cure condition
- Complications/associated conditions include skin condition, seronegative spondyloarthropathy (rheumatic arthritic condition affecting one or more joints), and ankylosing spondylitis
- Increases risk for colon cancer
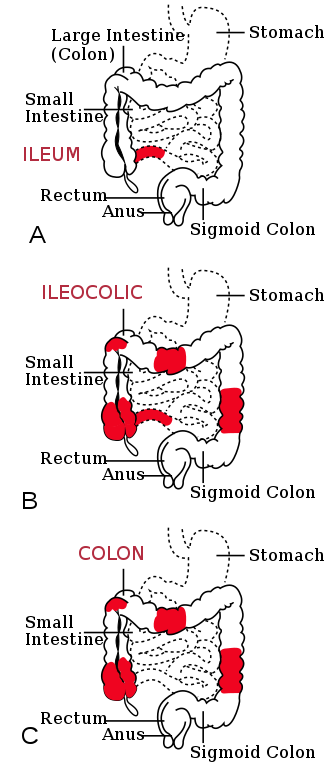
Wikipedia page: Crohn’s disease
Long Description
Illustration in 3 parts: A, B and C, of digestive tract with Crohn’s disease. All 3 have the following labelled:
- Stomach
- Large Intestine (Colon)
- Small Intestine
- Rectum
- Anus
- Sigmoid Colon
A: Ileum – a small segment of the small intestine is colored red.
B: Ileocolic – same red segment as A, plus 4 segments of the large intestine are colored red.
C: Colon – same 4 red segments as B, but no red segment of small intestine.
17.1.6.2 Ulcerative Colitis
- Inflammation uniform or continuous, often confined to one area
- Affects large bowel and rectum only
- Blood and mucous MORE common in stool
- Nausea and vomiting LESS common
- Inflammation in the mucosa only
- Granulomas uncommon
- Fistulas and strictures LESS common
- More common in ex-smokers or non-smokers
- Treated with steroids, immunosuppressives, biologics; 5-ASAs effective
- Surgery to remove in inflamed area can resolve the disease in some cases
- Complications/associated conditions seronegative spondyloarthropathy (rheumatic arthritic condition affecting one or more joints) and anklylosing spondylitis
- Increases risk for colon cancer
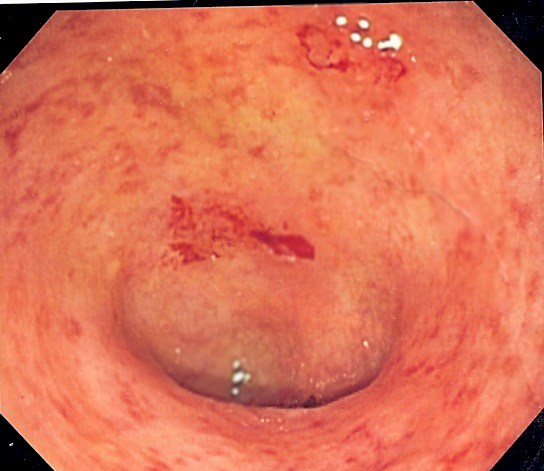
Wikipedia page: Ulcerative colitis
17.1.7 Diverticular Conditions
Diverticular conditions include two types of disorders: diverticulosis and diverticulitis. Diverticulosis is a condition that occurs when small pouches, or sacs, form and push outward through weak spots in the wall of the colon. In diverticulitis, one or a few of the pouches in the wall of the colon become inflamed.
17.1.8 Epiploic Appendagitis
https://www.osmosis.org/answers/epiploic-appendagitis
Please see link above for an Osmosis article on epiploic appendagitis. This is a relatively rare condition that has become recognized as an important source of abdominal pain. Epiploic appendages are small pouch-like appendages that line the intestinal wall. These pouches are filled with fat, and the purpose of these structures is not well understood. They may at times provide blood to the intestinal wall, provide cushioning abdominal cavity, and/or assist in immune function. These pouches can be come twisted or otherwise cut off from adequate blood supply, which can lead to necrosis. Abdominal pain associated with this condition can be quite severe, most often occurring in the left lower quadrant, although pain can occur at any area of the abdomen. The condition can me mistakenly diagnosed as acute diverticulitis or acute appendicitis. The pathophysiology of this conditions is being investigated, and the condition seems to be self-limiting. Treatment includes analgesics (NSAIDS) and monitoring, possibly with colonoscopy. Surgery or other invasive procedures are not warranted.
Resources
*NIDDK = National Institute of Diabetes and Digestive and Kidney Diseases

