Chapter 4: Infection
rlb18
Learning Objectives
After completing this chapter, the learner should be able to:
- Define the basic terminology associated with infection.
- Discuss micro-organisms that cause infection.
- Explain the principles of infection including transmission, host resistance, pathogenesis of micro-organisms, and control of transmission.
- Discuss the development of selected infections, including onset, signs and symptoms, diagnostic tests, and precautions.
- Discuss antibiotic-resistant organisms and implications for health care workers.
- Discuss basic diagnosis and medical management of infectious conditions.
Chapter Contents
- 4.1 Infection
- 4.2 Chain of Infection
- 4.3 Micro-organisms that Cause Infection
- 4.3.1 Bacteria
- 4.3.2 Viruses
- 4.3.3 Fungi
- 4.3.3.1 Selected Fungal Infections
- 4.3.3.1.1 Ringworm
- 4.3.3.1.2 .Candidiasis
- 4.3.3.1.3 Histoplasmosis
- 4.3.3.1.4 Parasites (plasmodia: malaria)
- 4.3.3.1.5 Protozoa
- 4.3.3.1.6 Giardia
- 4.3.3.1.7 Malaria
- 4.3.3.1.8 Helminths
- 4.3.3.1.9 Ectoparasites
- 4.3.3.1.10 Prion Disease
- 4.3.3.1.11 Creutzfeldt-Jakob disease (CJD)
- 4.3.3.1.12 Bovine Spongiform Encephalopathy (BSE or Mad Cow Disease)
- 4.3.3.1 Selected Fungal Infections
4.1 Infection
Infection is a condition in which cells of the body are invaded by pathogenic organisms, such as bacteria, viruses, fungi, and protozoa. The outcomes of infection can be benign to life-threatening. Many of the micro-organisms discussed in this chapter are normally kept in check by our immune systems. If immunity is weak or compromised by conditions such as stress, malnutrition, sleep deprivation, fatigue, medications, or other infections or conditions, micro-organisms can infect normal cells. These types of infections are termed opportunistic infections. Physical therapist assistants need to be aware of common causes of infection, methods of transmission, and actions to be taken to prevent and treat infection. This chapter will explore these concepts and discuss a few infectious agents that PTAs are most likely to encounter in clinical situations.
4.2 Chain of Infection
The chain of infection is important to the understanding of infectious diseases. Breaking the chain at any point can control the spread of disease, so efforts are made to intervene at each level.
The discussion of the chain of infection begins with an infectious agent, a pathogen or microbe that is capable of causing infection. There are many different infectious agents including bacteria, viruses, fungi, parasites, and prions, which are discussed in the following sections. The infectious agent needs a reservoir for survival. This could be a person, animal, insect, food, or water. The infectious agent is released from the reservoir through a portal of exit. Common portals in humans and animals include saliva, mucus, blood, feces, urine, semen, vaginal fluid, and vomitus. The mode of transmission is an important element of the chain, as it links one infected reservoir to another. Pathogens can be transmitted through different means: direct contact (skin-to-skin or skin to eyes or through handling contaminated foods, fluids or objects), or droplets (body fluids), or airborne (coughing, sneezing). The portal of entry is necessary to allow the infectious agent to enter the next host. Eyes, nose, mouth, and breaks in the skin are the most common portals of entry. There must be a susceptible host for the infectious agent to live and reproduce. People with depressed immune systems are more susceptible to infectious disease. Some of the most susceptible include: the very young; the very old; people with autoimmune diseases, such as rheumatoid arthritis or multiple sclerosis; people with other chronic conditions, such as diabetes mellitus or pulmonary conditions; people who are malnourished or obese, people who have had an organ transplantation; people with open wounds or burns; and people who are taking certain drugs, such as steroids or immunosuppressive medications.
This cycle continues as the pathogen continues to reproduce and be transmitted. If the chain of infection is broken, the spread of the disease can be slowed or stopped. Early identification of the infectious agent helps the medical community develop and administer appropriate interventions and target interventions in the appropriate populations. If the reservoir is a person, isolation of that person is common. If the reservoir is water or food, public health announcements, recalls, and efforts to decontaminate the supply are employed. Exit, transmission, and entry are controlled through hand-washing and other forms of hygiene. Maintenance of a clean environment and attention to proper handling of potentially infectious body fluids and contaminated objects is essential to controlling the spread of disease. The susceptibility of the host is controlled through vaccination and maintenance of healthy diet and lifestyle. For PTAs and other health care workers, it is extremely important to pay attention to the chain of infection and assist with efforts to interrupt the chain to maintain personal health and the health and well-being of patients and the community.
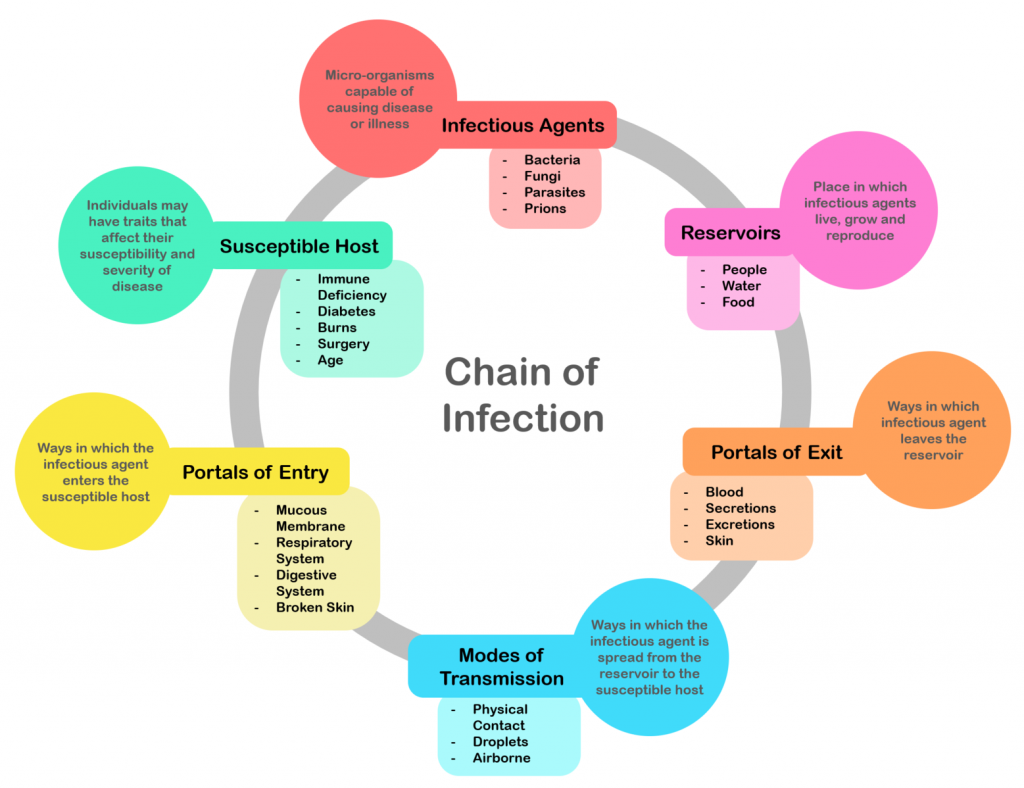
Long Description
Title: Chain of Infection
An illustration shows a circle with the 6 following categories. “Infectious Agents” is at the top and the rest are clockwise from the top.
Infectious Agents
Micro-organisms capable of causing disease or illness
- Bacteria
- Fungi
- Parasites
- Prions
Reservoirs
Place in which infectious agents live, grow and reproduce
- People
- Water
- Food
Portals of Exit
Ways in which infectious agent leaves the reservoir
- Blood
- Secretions
- Excretions
- Skin
Modes of Transmission
Ways in which the infectious agent is spread from the reservoir to the susceptible host
- Physical Contact
- Droplets
- Airborne
Portals of Entry
Ways in which the infectious agent enters the susceptible host
- Mucous Membrane
- Respiratory System
- Digestive System
- Broken Skin
Susceptible Host
Individuals may have traits that affect their susceptibility and severity of disease
- Immune Deficiency
- Diabetes
- Burns
- Surgery
- Age
4.3 Micro-organisms that Cause Infection
4.3.1 Bacteria
Bacteria are single-celled micro-organisms that are abundant in our bodies and in our environment. Most bacteria are harmless, in fact, the bacteria found in our digestive tracts and other parts of our bodies are essential for normal function. Even most bacteria in the environment are not harmful if the immune response is adequate. In the presence of virulent strains of bacteria or in the case of a depressed immune response, medical attention is necessary to help the body rid itself of the pathogenic organisms.
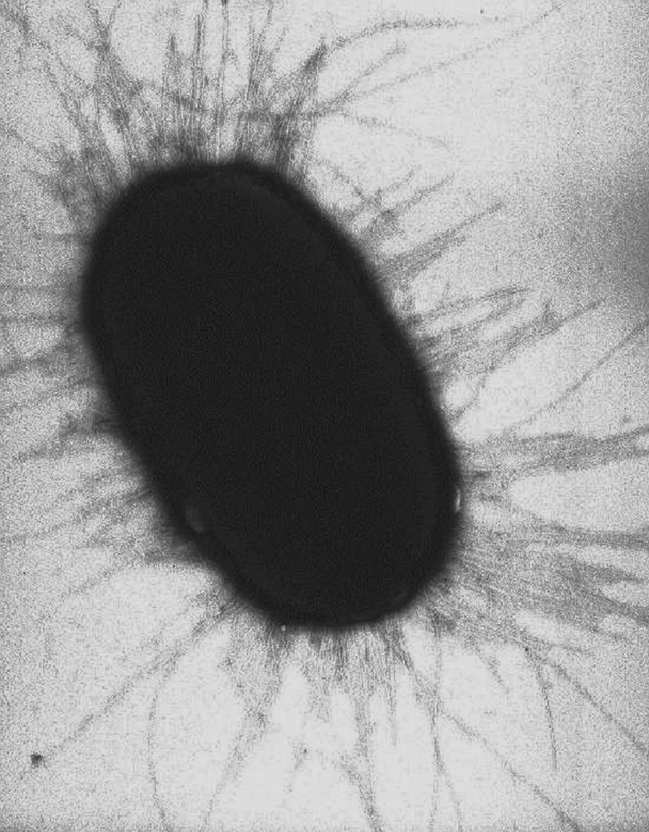
All bacteria have a few characteristics in common: a cell wall, a cell membrane, ribosomes, DNA and RNA. Some have flagella (long thick “tails”) to help them move, and some have fimbriae (small, thin hairs) that help them move and help them attach to other cells. The shapes of bacteria vary, with the most common being round (cocci), rod-shaped (bacilli), and spiral-shaped (spirilla). Bacteria are named for the manner in which they group together, also. Bacteria arranged in clusters, like grapes, are termed staphylococci. Those in chain are called streptococci. Staph and strep infections are among the most common types of infections.
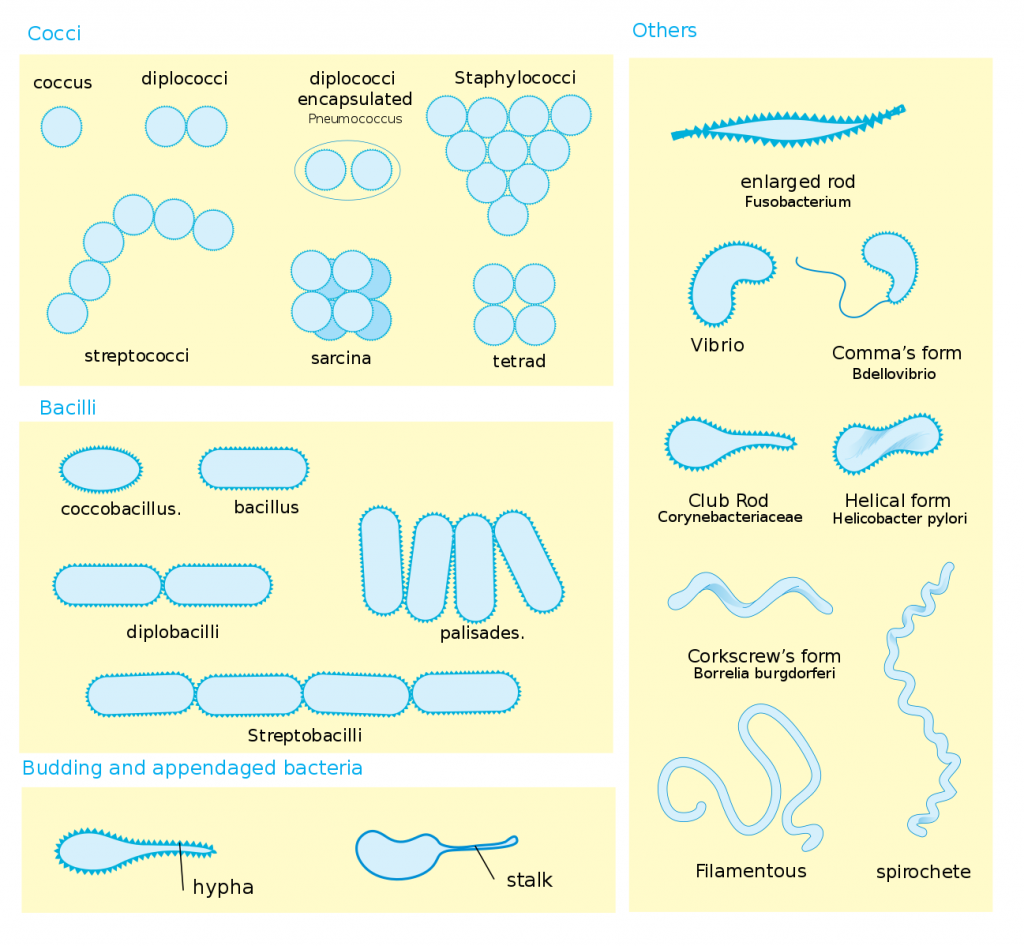
Long Description
Title: Types of Bacteria
An illustration with four panels.
Panel one is cocci which are round. Seven different versions are shown:
- Coccus: single cell
- Diplococci: 2 cells
- Diplococci encapsulated (Pneumococcus): 2 single cells in a balloon-type enclosure
- Staphylococci: cells in a cluster like grapes
- Streptococci: a chain of cells
- Sarcina: 2 sets of 2 by 2 cells
- Tetrad: 4 cells, 2 by 2
Panel 2 is basilli which are rod and oval shaped. 5 versions are shown:
- Coccobacillus: oval shaped
- Bacillus: rod shaped
- Diplobacilli: 2 rod shaped cells together like train cars
- Streptobacilli: 4 cells like train cars
- Palisades: 4 cells side by side (not like a train)
The third panel is labeled “Budding and appendaged bacteria” and shows hypha and stalk which are tear-drop shaped.
The 4th panel is labeled “Others” and shows:
- Enlarged rod, Fusobacterium
- Vibrio
- Commas form, Bdellovibrio
- Club Rod. Corynebacteriaceae
- Helical form, Helicobacter pylori
- Corkscrews form, Borrelia burgdorferi
- Filamentous
- Spirochete

In a bacterial infection, bacteria enter the body and begin replicating through binary fission. They can use the nutrients intended for body cells to fuel their own reproduction. The immune response begins soon after bacteria enter and can last for many days or weeks until the infection is cleared. Some particularly dangerous bacteria can create infections that spread throughout the body via the blood and lymphatics, killing many body cells and causing organ failure (septicemia).
In less developed parts of the world, bacterial infections such as tuberculosis, typhoid fever, diphtheria, and cholera are a major cause of mortality and morbidity. In developed countries, the overuse and misuse of antibiotics has led to the development of antibiotic-resistant strains of bacteria. Because bacteria can change slightly in response to the environment with each new generation, new cells can contain new genetic codes that create resistance to incompatible environments, as are created in the presence of antibiotics.
Common bacterial infections include foodborne illnesses (e.g. salmonella, e. coli), Helicobacter pylori (peptic ulcer disease), chlamydia, syphilis, gonorrhea, staphylococcus, streptococcus, clostridium difficile (C-diff) and Lyme disease.
Bacteria can be transmitted to and between people in many ways. Bacteria on the hands of health care providers are responsible for transmission of many infections, such as C-diff, strep and staph infections. Food handlers or on equipment used in food preparation cause bacterial infections, such as salmonella and E. coli. Airborne or droplet transmission is the major transmission route for tuberculosis. Body fluid contamination is responsible for chlamydia, gonorrhea, and syphilis. Insects can transmit harmful bacteria to humans in Lyme disease, and Rocky Mountain Spotted Fever.
Antibiotic medicines are used to treat bacterial infections. The development and use of antibiotics have been extremely helpful in reducing the morbidity and mortality from infection in developed areas of the world. In areas where antibiotics are less available, infection from bacterial infection continues to be a significant cause of death. The overuse and misuse of antibiotics has let to the development of “superbugs,” or strains of bacteria that are resistant to commonly used antibiotics.
For more information on bacteria, please watch the following video.
4.3 – Resource 04 – “Bacteria” by Khan Academy is licensed under Fair Use
4.3.1.1 Selected Bacterial Infections
4.3.1.1.1 Clostridioides difficile (C-diff)
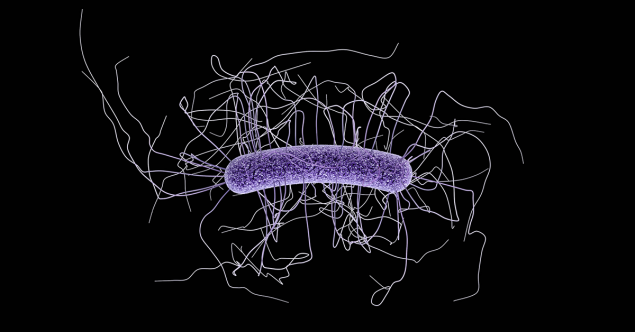
Clostridioides difficile, or C-diff is a bacterium that causes diarrhea and colitis. It is most common for C-diff to occur in people with immunodeficiency who have been taking antibiotics. Since normal bacteria in our guts helps to maintain overall colon health, disruption to that balance, as seen with antibiotic use, can result in the symptoms associated with C-diff, including severe diarrhea, abdominal pain, and fever. Most people carry C-diff in their intestinal tract, but the C-diff is in the inactive form. If it becomes activated through antibiotic use, it can cause a potentially deadly infection. Severe diarrhea can lead to dehydration and electrolyte imbalance, which can be disastrous in an elderly, immunocompromised individual. C-diff is most commonly transmitted from one patient to another in a hospital or residential facility through unwashed hands or contaminated objects or equipment. Treatment for C-diff includes ceasing causative antibiotic treatments and may include administering metronidazole, vancomycin, fidaxomicin, and fecal microbiota transplantation. Most people recover from an infection of C-diff, but it can be fatal in some cases.
C-diff has been highly associated with hospitalization and nursing homes, but it is becoming more prevalent in community-dwellers. It is vitally important that PTAs and all health care workers wash their hands and use every precaution to avoid transmitting this and other infectious diseases between patients.

4.3.1.1.2 Methicillin-Resistant Staphylococcus aureus (MRSA)
Methicillin-Resistant Staphylococcus aureus (MRSA) is a strain of bacteria that is resistant to commonly used antibiotics. S. aureus is present in the nose and on the skin of many people, and a small fraction of those people have MRSA in these areas with no ill effects most of the time. MRSA in an open skin lesion or elsewhere in the body can be quite problematic. The increase in MRSA is associated with the increased use of antibiotics and hospitalization of more immunocompromised individuals, and the increased use of catheters and other invasive equipment.
The MRSA infection spreads between people through skin-to-skin contact, through catheters and other hospital equipment, in athletic facilities on equipment and through shared towels and razors, and through injections of opioids and other drugs in the community. It has become more of a public health issue, as it has moved from being primarily a hospital-associated infection (HA-MRSA) to also being a community-associated infection (CA-MRSA). Those people with close contact with others, such as athletes, military personnel, and people living in nursing homes are at a higher than average risk for exposure to MRSA.
For health care workers, appropriate hand hygiene and protective equipment are essential to diminish the transmission of MRSA. To minimize the spread of MRSA in the community, athletes and others are encouraged to not share towels, clothing, or other personal items, such as razors. It is important for all people to maintain proper handwashing and be especially careful around dressings, clothing, and anything that comes in contact with a potentially infected wound or skin area.
MRSA most often causes infections of lesions on the skin or boils on the skin, but it can affect the lungs or any organ of the body or even cause septicemia and affect many organs. The most common symptoms of MRSA include a pimple, boil, or open sore on the skin that is red, swollen, painful and pus-filled. Fever may also be present. It is recommended that bumps or sores are covered with bandaging until a health care provider can determine whether MRSA is present or not. Treatment with appropriate antibiotics is usually instituted immediately, as MRSA can spread through the body quickly, and can be fatal. There are limited antibiotics available to treat a MRSA infection, but presently, linezolid, teicoplanin, and vancomycin are considered the drugs of choice. Intravenous administration is often used in these cases.
The CDC page on MRSA
4.3.1.1.3 Lyme Disease
Lyme disease is caused they the bacterium Borrelia burgdorferi and is transmitted to humans via the bite of infected blacklegged ticks, or deer ticks, which are common in the northeastern United States. Confirmed cases of Lyme disease have increased steadily over the past several decades.
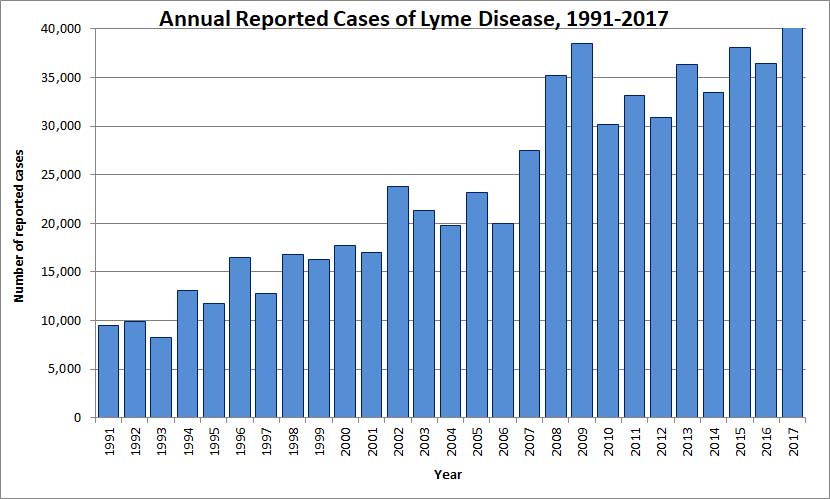
Long Description
Title: Annual Reported Cases of Lyme disease, 1991-2017
A vertical bar chart of “Annual Reported Cases of Lyme Disease” is shown with the X axis as time (1991 to 2917) and the Y axis as “Number of reported cases”. The first 3 years are less than 10,000 which then grows linearly to 35,000 to 40,000 by 2015, 2016 and 2017. 2008 and and 2009 are outliers of 35,000 and 38,000.
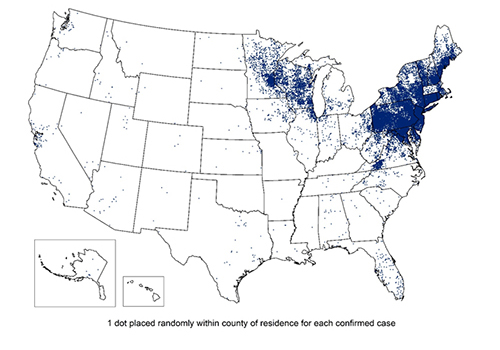
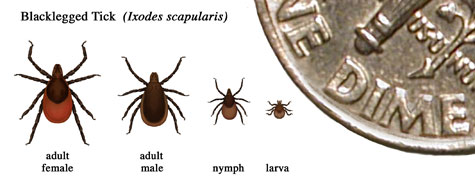
It is most common for a nymphal tick transmit the bacterium to a human, as these very small ticks often go unnoticed. Adult ticks can also transmit Lyme disease, but these larger ticks are usually detected and removed before they bite and infect humans.
Common signs and symptoms of Lyme disease are usually quite vague in the first 3 to 30 days following infection. These symptoms include fever, chills, headache, muscle and joint aches and swollen lymph nodes. A rash (erythema migrans) occurs in 70-80 percent of infected individuals several days after the tick bite occurred. The rash usually first appears at the site of the bite and sometimes has a bull’s-eye appearance. It is usually painless but might feel warm and may appear on any part of the body. The rash can appear in many different forms, all are red, and none blister. Sometimes, there is no rash at all.

Later signs and symptoms, which can occur days to months after the tick bite, include:
- Severe headaches and neck stiffness
- Additional EM rashes on other areas of the body
- Arthritis with severe joint pain and swelling, particularly the knees and other large joints.
- Facial palsy (loss of muscle tone or droop on one or both sides of the face)
- Intermittent pain in tendons, muscles, joints, and bones
- Heart palpitations or an irregular heart beat (Lyme carditis)
- Episodes of dizziness or shortness of breath
- Inflammation of the brain and spinal cord
- Nerve pain
- Shooting pains, numbness, or tingling in the hands or feet
- Problems with short-term memory
4.3 – Resource11 – Later signs and symptoms, which can occur days to months after the tick bite – “Signs and Symptoms of Untreated Lyme Disease” by CDC, Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases is in the Public Domain
Content source: Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Vector-Borne Diseases (DVBD)
Lyme disease is diagnosed through signs and symptoms and history of possible exposure to infected ticks. Blood tests are available for assistance in the diagnosis. The CDC presently recommends a 2-step laboratory blood test to most accurately diagnose the condition.
Antibiotics, such as doxycycline, amoxicillin and cefuroxime axetil are the most commonly prescribed oral medications to treat Lyme disease during the early stages. If the neurological system or cardiac system is involved, intravenous administration of antibiotics could be necessary. Patients in the later stages (disseminated) Lyme disease generally have less favorable outcomes than those who are treated in the early stages.
Some patients describe long-term effects of Lyme disease (fatigue, joint pain, muscle aches). The term “post-treatment Lyme disease syndrome,” (PTLDS) is used to describe this condition. Content source: Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Vector-Borne Diseases (DVBD) CDC page on Lyme Disease
4.3.2 Viruses
Viral infections can, like bacterial infections, have overall effects on the body in varying degrees. Viruses are much smaller than bacteria, and they work differently in the body. A virus-host relationship is truly parasitic, with the virus entering the host cell and using either the cell’s DNA or RNA for reproduction. Viruses reproduce within the cell and are released from the cell, often destroying the cell in the process. The released virons infect neighboring cells, where they reproduce, and the process continues.
For a more detailed explanation of viruses and how they affect cells, please watch the following video.
4.3 – Resource 12 – “Viruses” by Khan Academy is licensed under Fair Use
There are many different viral infections common to the human population. Rhinovirus (common cold), influenza (flu), herpes viruses (cold sores, genital sores), varicella (chickenpox and shingles), measles, mumps, hepatitis A-E viruses, Epstein-Barr (mononucleosis), human papilloma virus (HPV), and human immunosuppressive virus (HIV). Many viral infections are associated with fever, malaise, skin rash, and other symptoms associated with the area of infection. For example, in the case of hepatitis, jaundice (yellowing of the skin and eyes) is a common symptom, which is caused by liver malfunction, resulting in hyperbilirubinemia. If the infection occurs in the respiratory tract, as in rhinovirus or flu, coughing, runny nose, and watery eyes can occur. In mumps, infection in the parotic and salivary glands causes the characteristic enlargement of the neck area.
Viruses are transmitted to susceptible hosts through various means. Mother-to-child transmission is possible through the placenta, during the birth process, or through breast feeding. Examples of this vertical transmission mode include HIV and HPV. Body fluid transmission is the vehicle for transmission of many viruses, such as HPV, HIV, Epstein-Barr, and Ebola. Airborne or droplet transmission occurs in viruses including rhinovirus, influenza, measles, and mumps. Ingestion of contaminated food or water causes viral infections such as norovirus. Animals can transmit viruses to humans. Examples include: West Nile virus and H1N1 (birds), rabies (mammals), swine flu (pigs), and Zika and dengue fever (mosquitoes).
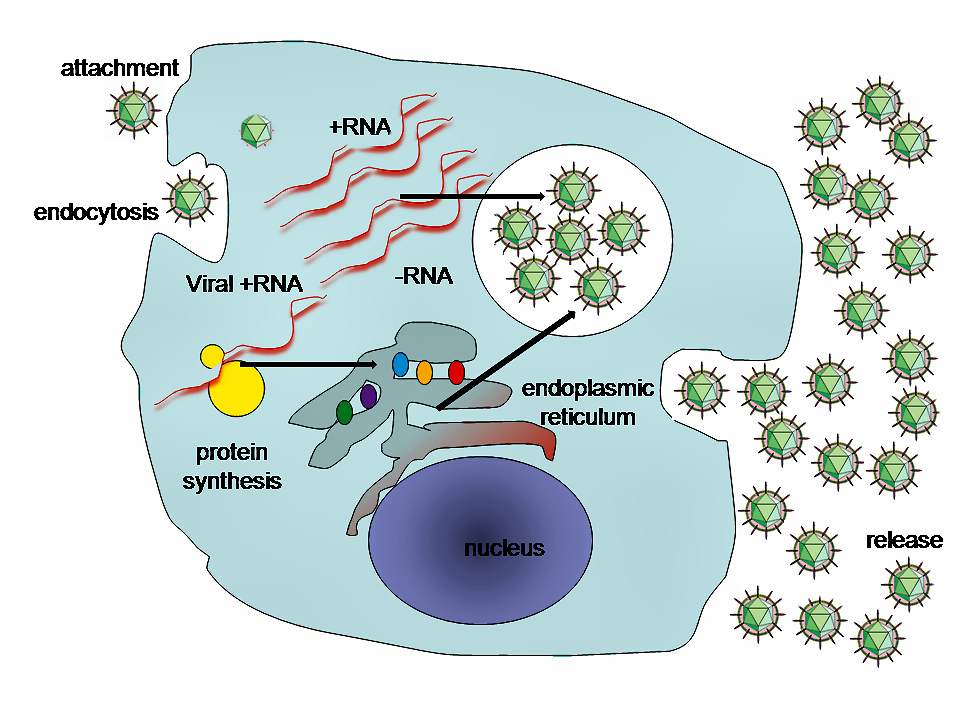
A simplified diagram of the Hepatitis C virus replication cycle.
The long-term effects of viral infection are quite variable. Common colds caused by rhinoviruses rarely induce more than a mild annoyance in humans. Other viruses, such as Ebola and Marburg viruses, can cause death in a matter of days. Some viruses remain dormant in the body for years, and can re-emerge later in life, such as the varicella virus, where chicken pox can re-emerge as shingles. The hepatitis viruses can cause chronic liver disease and are linked to liver cancer. HPV is linked to cervical cancer.
Even viral infections that are not problematic for the greater population can be very problematic for immunocompromised individuals. The very young and the very old, people with autoimmune diseases, people with cancer and those undergoing chemotherapy or radiation therapy, people who take steroidal medications, and people with any kind of chronic disease or organ transplantation are much more susceptible to viral infections, and have a much weaker immune response, so that an infection such as influenza can be fatal.
Medical interventions for viral infection are also varied, depending upon the virus and the general health condition of the infected individual. For otherwise healthy people, common viruses, such as rhinovirus and influenza are treated only symptomatically. Anti-viral drugs are available for more serious infections and for those people with depressed immune function. Rabies is one viral disorder that must be treated prior to the virus becoming active. A fast-acting shot (rabies immune globulin) is administered as soon as possible to prevent the virus from infecting the body’s cells, followed by a series of rabies vaccines to help the body learn to identify and fight the rabies virus.
Vaccination is an important component in diminishing the effect of many viruses on the population. Vaccines are available for influenza, HPV, hepatitis, measles, mumps, rubella, polio, and varicella. All health care workers should be fully vaccinated and adhere to all precautions, including hand-washing, to decrease the chance of infection to, from, and between patients.
Long Description
Title: Overview of Viral Infections
An illustration of the human body shows internal organs, the brain, throat, spots on the skin and swollen neck.
Encephalitis/meningitis – points to brain
- JC virus
- Measles
- LCM virus
- Arbovirus
- Rabies
Pharyngitis – points to throat
- Adenovirus
- Epstein-Barr virus
- Cytomegalovirus
Common Cold – points to throat
- Rhinovirus
- Parainfluenza virus
- Respiratory syncytial virus
Gingivostomatitis – points to throat
- Herpes simplex type 1
Myelitis- points to liver
- Poliovirus
- HTLV-I
Gastroenteritis – points to spleen and intestines
- Adenovirus
- Rotavirus
- Norovirus
- Astrovirus
- Coronavirus
Parotitis – points to swollen side of throat
- Mumps virus
Pancreatitis – points to pancreas
- Coxsackie B virus
Eye infections – points to eyes
- Rhinovirus
- Parainfluenza virus
- Respiratory syncytial virus
Cardiovascular – points to heart
- Coxsackie B virus
Hepatitis – points to liver
- Hepatitis virus types A, B, C, D and E>
Sexually transmitted diseases
- Herpes simplex type 2
- Human papillomavirus
- HIV
Pneumonia – points to lungs
- Influenza virus, Types A and B
- Parainfluenza virus
- Respiratory syncytial virus
- Adenovirus
- SARS coronavirus
Skin infections – points to dots on skin/arm
- Varicella zoster virus
- Human herpesvirus 6
- Smallpox
- Molluscum contagiosum
- Human papillomavirus
- Parvovirus B19
- Rubella
- Measles
- Coxsackie A virus
4.3.2.1 Selected Viral Infections
4.3.2.1.1 Respiratory Syncytial Virus (RSV)
RSV is a very common virus which, for most people, causes cold-like symptoms for a week or two and is followed by complete recovery. For very young infants, the elderly, and people with compromised immune responses, the virus can be quite problematic, however. It is the most common cause of bronchitis in babies and is a significant factor in respiratory illness in older adults. CDC page on RSV
RSV is transmitted through coughing, sneezing, and talking, and through direct and indirect contact with an infected person. The symptoms of RSV can be treated with over-the-counter ibuprofen or acetaminophen. Dehydration is a concern, particularly for vulnerable populations. In severe cases, hospitalization might be necessary, and interventions, such as supplemental oxygen might be necessary.
No specific antiviral medications or preventative vaccines for RSV are available, but research to develop these is ongoing. CDC page on RSV Symptoms
4.3.2.1.2 Measles
For a short lesson from the CDC on the basic pathophysiology of measles, view the following video..
Measles is a viral condition that is highly contagious, both before and after the characteristic rash appears. According to the CDC, 90% of nonvaccinated people who have close contact with a person who has measles, will become infected. CDC: Measles Transmission Measles is transmitted via coughing, sneezing, talking, and through direct and indirect contact. The measles virus remains active in the air or on surfaces for several hours, so it is easily spread from person to person.
Signs and symptoms of measles include cough, coryza (runny nose), conjunctivitis (red, watery eyes, fever, and macular-papular rash (flat red spots) on the body. Kaplik spots generally appear in the mouth a few days before the rash appears on the rest of the body.
Measles will often “run it’s course” in less than 2 weeks, but for some, measles will have life-long, or even deadly effects. Common associated problems with measles include ear infections and diarrhea. Less common, but more serious problems include pneumonia, which can be fatal, or encephalitis, which can cause permanent hearing loss, brain damage, or death.
As with other forms of infection, the most vulnerable groups are at the highest risk for complications. Children under the age of 5, the elderly, pregnant women, and people who have a weakened immune response are at especially high risk.
Measles is preventable through a vaccination (MMR) that has been successfully administered for more than 50 years. Because of widespread acceptance and use of vaccination, measles was declared eliminated in the US in 2000 CDC: Measles History. There has been a large increase in the number of measles cases in the US since 2010 due to (1) misinformation leading to decreased vaccinations in children; (2) lack of continued immunity in those vaccinated many years ago; and (3) increased international travel (most cases of measles in the US have been trace to an origin outside the country) . For the most recent information on states reporting measles cases (measles has been reported in Pennsylvania) and other important information on the recent resurgence in measles, see the CDC website.


4.3.2.1.3 Mumps
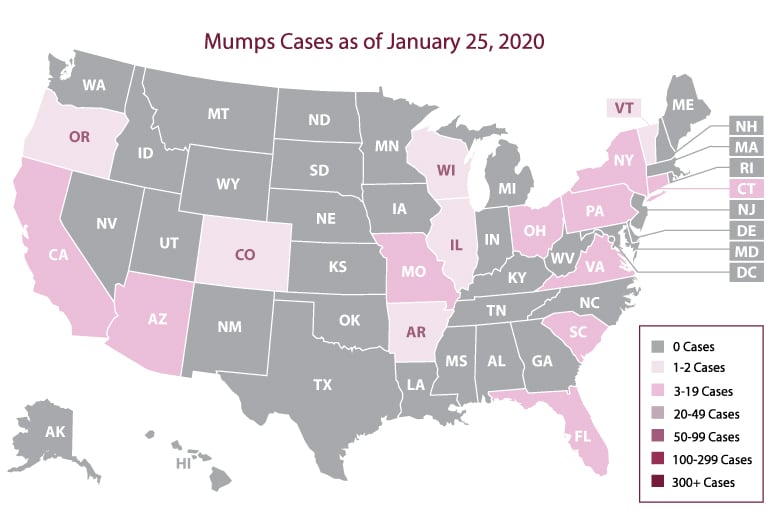
Mumps infections are very rare in the United States, since the MMR (measles, mumps, rubella) vaccination is available and widely utilized. The CDC is aware of several recent outbreaks in communities across the United States. Close-knit communities, such as schools, universities, church groups, and families are most susceptible.
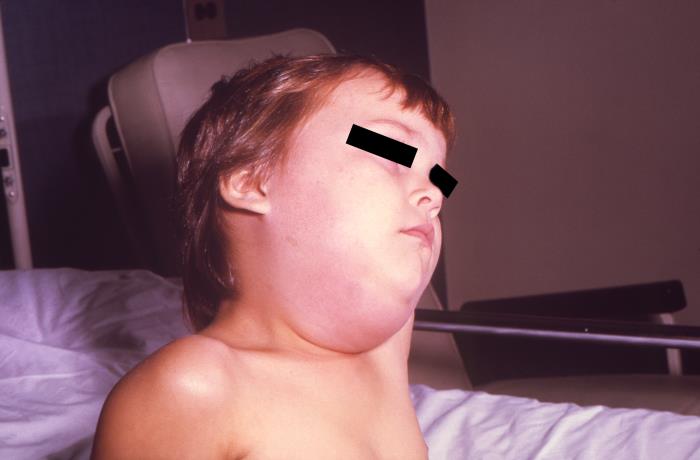
Mumps is caused by the mumps virus and affects children more often than adults. The virus is transmitted through direct contact with saliva or touching infected individuals or contaminated objects. It is also commonly transmitted through respiratory droplets in the air spread through coughing, sneezing and talking.. The initial symptoms of mumps include fever, headache, and general malaise, and within a few days, swelling of the parotid and salivary glands begins. Sore throat and painful swallowing are also common. Some people can be only mildly affected, while others can experience serious complications, including meningitis, encephalitis, hearing loss, and inflammation of the pancreas, and inflammation of the testicles in males and the ovaries in females. Most people will recover from mumps within 2 weeks.
CDC page on Mumps.
4.3.2.1.4 Hand, Foot, and Mouth Disease (enterovirus group)
Hand, foot, and mouth disease is transmitted between humans through airborne particles, close personal contact, lack of hand hygiene, and contact with contaminated objects and surfaces. This disease affects children under the age of 5 most often but can affect adults. Symptoms of the disease include fever, malaise, decreased appetite, sore throat, and characteristic rashes of the feet and hands, and blistering in the mouth and throat. Red spots and blistering can occur anywhere on the body. Fingernail and toenail loss occur in some individuals. Most people with healthy immune responses will completely recover from a bout with hand, foot and mouth disease, but more serious outcomes are possible, especially in the very young, very old or others with poorly functioning immune systems. Encephalitis and meningitis can occur with hand, foot, and mouth disease, and either could lead to long-term neurological disorders or death.
CDC page on Hand, Foot and Mouth Disease


4.3.2.1.5 COVID-19
COVID-19, which stands for coronavirus disease, identified in 2019, is also is known as SARS-CoV-2. SARS (severe acute respiratory syndrome) infections caused an outbreak in 2003, and is the same root-virus as COVID-19 . COVID-19 is responsible for a world-wide pandemic in 2020 and 2021 and remains present in all areas of the world. COVID-19 is highly communicable through airborne droplets and aerosol particles transmitted through talking, coughing, sneezing, and singing. Prolonged exposure with an infected individual is correlated to higher infection rates, as well. The incubation period for COVID-19 is 2-14 days, with the 3 days prior to symptoms being them most highly contagious period. People remain infectious for up to ten days after the onset of symptoms in moderate cases and up to twenty days in severe cases.
Common symptoms and symptoms of severe disease caused by COVID-19 are illustrated below.
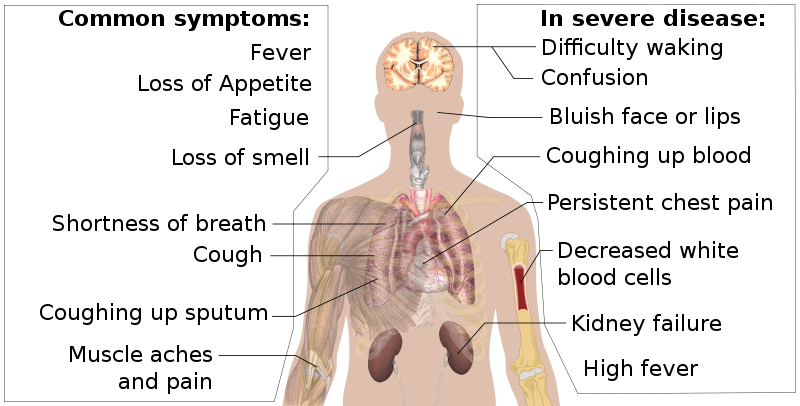
Long Description
Common symptoms and symptoms of severe disease by COVID-19
An illustration of the human body shows internal organs, the brain, throat, muscles in arm, kidneys and blood in arm.
Common symptoms
- Fever
- Loss of Appetite
- Fatigue
- Loss of smell – points to upper throat
- Shortness of breathe
- Cough – points to lungs
- Coughing up sputum – points to lungs
- Muscle aches and pain – points to muscles/joints
In severe disease
- Difficulty waking – points to brain
- Confusion – points to brain
- Bluish face or lips – points to face
- Coughing up blood – points to lungs
- Persistent chest pain – points to heart
- Decreased white blood cells points to blood in arm
- Kidney failure – points to kidneys
- High fever
The course of the disease is quite variable. Many people who are infected with COVID-19 are asymptomatic and can be transmitting the disease without even knowing they are infected. Some people develop mild cold-like or flu-like symptoms and recover with little or no long-term consequences. Some people experience severe symptoms, requiring hospitalization, ICU intervention, and ventilatory assistance. Andy many people have died from the disease. People who are elderly or have compromised immune systems from other conditions (autoimmune disease, diabetes, obesity) are particularly at risk for developing severe symptoms, but many people with none of these risk factors have also been very ill or died with COVID-19 infections.
“Long COVID” is a term applied to symptoms lasting more than 12 weeks following a COVID infection. The most common long-COVID symptom is fatigue. Other symptoms include shortness of breath, cough, chest pain, cardiomyopathy, headaches, sensory loss , and cognitive impairment. Long COVID is being studied, so results are preliminary, but it does appear that many individuals are experiencing long-term effects following COVID infections. For more information on long COVID, watch the video below:
youtube.com/watch?v=c8b_TMXOzEk
Pathophysiology of COVID-19
4.3.3 Fungi
Fungal infections, also known as mycoses, have become important health care considerations as antibiotic use has increased and the number of people living with diminished immune responses has increased. Fungi are simple singular or multicellular organisms that are normally found in many parts of the body. An infection is most often an opportunistic infection, where normally residing yeasts or molds in the body are not able to be controlled by the immune response. Mycoses usually occur in immunosuppressed individuals in or people who are taking antibiotics. Fungal organisms commonly infect the epithelial cells of the skin, nails, respiratory tract and urogenital tract, and less commonly affect other body systems. These organisms are parasitic in nature, using normal body cells and their substrates to help them live and reproduce. It is possible for some forms of mycoses (e.g. ringworm and athlete’s foot) to be transmitted from person to person, but most are not transmitted this way.
Antifungal creams are effective on most skin and nail infections. Other infections in the lungs or elsewhere can require hospitalization and medications to address complications.
4.3.3.1 Selected Fungal Infections
4.3.3.1.1 Ringworm
Ringworm (tinea) infections can occur in the skin, nails, or almost anywhere in the body. These are common infections spread through direct contact. Tinea pedis (athlete’s foot), tinea capitis (ringworm on the scalp), and tinea curis (jock itch) are some of the most common forms.
4.3.3.1.2 Candidiasis
Many different candida yeast species normally live in the body, most abundantly on the skin and in the mouth, throat, gut and vagina. There are usually no adverse effects of these organisms, but if there is a situation where the immune system is compromised, such as antibiotic use or presence of other disease or condition, such as malnutrition or alcoholism, candida yeasts can cause infection anywhere in the body. Commonly, candidiasis infections (usually just referred to as “yeast infections”) occur in the vagina, or as “thrush” in the mouth (oropharyngeal candidiasis). In invasive candidiasis, the organisms enter the bloodstream and cause infections in the brain, heart, kidneys, or other organs.
According to the CDC, one particular form of candidiasis, Candida auris, is of particular concern and a serious global health threat. This infection causes severe illness and is resistant to multiple antifungal medications.
4.3.3.1.3 Histoplasmosis
Histoplasmosis is an infection caused by the Histoplama fungus. Spores for this fungus are found in the air in areas where there is an abundance of bat or bird droppings. In the US, the Ohio Valley and the Mississippi Valley regions are the most common places to find Histoplasma in the environment. Spores are transmitted to humans through the air, and the infection is usually found in the respiratory tracts of affected individuals. Many people who encounter the histoplasma fungus will not experience symptoms at all. Common symptoms for those who do experience symptoms include fever, chills, malaise, cough and chest pain. Most people will recover from the infection within a month with no residual effects, but those with immunosuppression can experience long-term lung infection or central nervous system involvement, causing encephalitis or meningitis. Rarely, histoplasmosis takes the form of “disseminated histoplasmosis,” in which many organs are affected. This form can be fatal.
4.3.3.1.4 Parasites (plasmodia: malaria)
Parasites are organisms that live on or within another organism, gaining nutrients from the organism in a harmful way. There are three main classes of parasites that can cause disease in humans: protozoa, helminths, and ectoparasites.
4.3.3.1.5 Protozoa
Protozoa are single-celled organisms that can be transmitted to humans through arthropod vectors (bite of mosquito or fly), or through fecal-oral routes through contaminated food or water or through direct contact.
4.3.3.1.6 Giardia
Giardia is a common protozoan intestinal parasite that is round in human excrement and is most often transmitted through drinking water or in recreational water, such as swimming pools or lakes. An infected person will exhibit signs and symptoms of gastro-intestinal disturbance, such as diarrhea, vomiting, and abdominal cramping or pain. Giardiasis is usually self-limited with symptoms lasting a few days to several weeks. It is most dangerous to young children, the elderly and others with compromised immune function who are likely to suffer ill-effects from dehydration and weight loss.
4.3.3.1.7 Malaria
Malaria is a major concern for many people in underdeveloped countries and for people in the US, mainly when they travel to countries in sub-Saharan Africa and South Asia. Malaria caused by the plasmodia parasite and is transmitted between humans through mosquitoes. A mosquito picks up the parasite from biting one infected individual and then transmits it to another when it bites again. The life cycle of malaria is depicted in the graphic below.
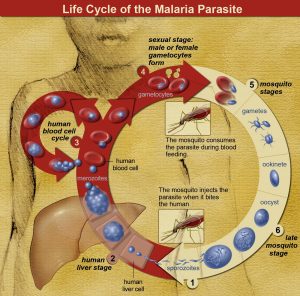
Malaria is a dangerous, and sometimes deadly, disease. Signs and symptoms include high fevers, chills, and severe flu-like symptoms. The liver and eventually the blood are involved in the human infection with malaria, with the blood stage being associated with the symptoms of the disease. As with other infectious diseases, the less robust the immune functioning of the individual, the more likely they are to suffer the worst consequences of the disease.
Malaria can be successfully treated with medications specific to the infecting species, the geographic site of infection, and the severity of infection. Preventative measures are important for travelers to countries where malaria is endemic. Preventative medications are available and everyone who travels should wear protective clothing and use insect repellant. Bed nets are available for sleeping, especially where air conditioning and window screens are not available.
Long Description
Life Cycle of the Malaria Parasite
A circle represents the life cycle of the malaria parasite starting at the bottom with number 1.
- Mosquito injects the parasite (sporozoites) when it bites the human
- Human liver stage via liver cells.
- Human blood cell cycle: merozoites infect human blood cells
- Sexual stage: male or female gametocytes form
- Mosquito consumes the parasite during blood feeding
- Mosquito stages
- gamete
- ookinete
- oocyst
- Late mosquito stage
4.3.3.1.8 Helminths
Helminths are intestinal worms, including roundworms, hookworms, and whipworms. These worms are usually found in the soil or water in tropical climates. They are transmitted through larvae found in human feces that penetrate the skin through the feet. Eggs can also be ingested through water or food contamination. Signs and symptoms of infection can include anemia, vitamin or other nutritional deficiency, impaired growth and intestinal blockage. Infection can be treated, usually very quickly and easily, through specific medications. Prevention is also important. Adequate clean fresh water is essential for human hygiene, washing and preparation of food, and of course, drinking. It is recommended that people wear shoes in areas likely to contain helminths.
4.3.3.1.9 Ectoparasites

Scabies: note burrowing “bug” in upper right corner
Ectoparasites are parasites that live primarily on the outside of the host, mostly on the skin or in the hair of humans. Common ectoparasites include crab louse (pubic lice), pediculosis (head lice) and scabies. These parasites are spread through direct and indirect contact, as on a fomite, such as a hat, head rest, carpet, bed sheet or towel. These organisms are multicellular “bugs” that are easily transmitted through groups of people living in close quarters, schools, gyms, and families. Infections can be annoying, causing itchiness and associated infection risk from scratching, but all are easily treated once diagnosed. Since these organisms are macroscopic as adults, they can often be seen with the naked eye or with simple magnification. People with these conditions should avoid contact with others until the condition is controlled.
4.3.3.1.10 Prion Disease
Prions are poorly understood protein variants that can become pathogenic and affect the central nervous system. Although the risk of being infected by a prion, the diseases associated with prion infection are very serious.
4.3.3.1.11 Creutzfeldt-Jakob disease (CJD)
The classic form of CJD is rare, occurring in approximately one person per million in the US and around the world. It seems a normal prion in the brain transforms into an abnormal prion that attacks normal brain cells. It causes severe neurodegeneration and muscle wasting. It is always fatal, with death occurring within a year of diagnosis. Most cases (85%) are caused by spontaneous mutation of a normal prion into a pathogenic prion. The remainder of the cases are caused by inherited genes. Most cases of CJD occur in people over the age of 50. The only known form of transmission between people can occur in invasive surgical procedures, such as brain surgery. CDC page on Creutzfeldt-Jakob Disease
4.3.3.1.12 Bovine Spongiform Encephalopathy (BSE or Mad Cow Disease)
BSE is a prion infection that affects cattle, but can, on rare occasions, be transmitted to humans. The abnormal prion causes deadly neurodegeneration in cattle and in humans, which is considered to be a variant of CJD (vCJD). Since vCJD was first reported in 1996, a total of only 231 patients with this disease, including 3 secondary, blood transfusion-related cases, have been reported worldwide. The risk to human health from BSE in the United States is extremely low. CDC page on Mad Cow Disease
Antifungal Medications
There are many types of antifungal medications, some over the counter, some prescription. There are 3 main types of antifungal medications and they work in different ways.
- Azoles (fluconazole or Diflucan®), synthetic (human-made) antifungals that keep fungi from growing.
- Echinocandins (micafungin or Mycamine®), newer semi-synthetic antifungals that attack and damage the fungus wall.
- Polyenes (nystatin or Bio-Statin®), organic (naturally occurring) antifungal treatments that destroy the fungus cell.
The most common side effects of antifungal medications include itchy or irritated skin and GI problems, such as diarrhea and stomach ache. More serious side effects are rare, but can occur. These include liver damage and severe allergic reaction.
Read “Hiding in Plain Sight: How You Can Fight Bacterial Contamination in Your Clinic.” Answer the following questions.
- Name the two places identified in the article where bacteria are likely to “hide.”
- According to the article, when should a PTA perform appropriate hand hygiene?
- Name one instance when hand washing with antibacterial soap is preferred over the application of alcohol based hand sanitizer (ABHS).
Infection Resources:
Section 4.1
Section 4.2
Resource 01 – Chain of Infection – “File:Logarithmic time scale – milliseconds to years.svg” by Genieieiop is licensed under CC BY-SA 4.0
Section 4.3
Resource 01 – “File:Bacterial morphology diagram.svg” by LadyofHats is in the Public Domain
Resource 02 – “File:E. coli fimbriae.png” by (Image: Manu Forero), Bacterial Fimbriae Designed to Stay with the Flow. Gross L, PLoS Biology Vol. 4/9/2006, e314. doi:10.1371/journal.pbio.0040314 is licensed under CC BY 2.5
Resource 03 – “File:EMpylori.jpg” by Yutaka Tsutsumi, M.D. Professor Department of Pathology Fujita Health University School of Medicine is in the Public Domain
Resource 04 – “Bacteria” by Khan Academy is licensed under Fair Use
Resource 05 – “File:Clostridium difficile CDC.jpg” by CDC/ James Archer is licensed under CC BY-NC-SA 4.0
Resource 06 – Clostridioides difficile infection – “File:Pseudomembranous colitis.JPG” by Donated by the pathologist at work. is in the Public Domain
Resource 07 – “The number of cases of Lyme disease report to CDC has increased steadily over the past 25 years.” by CDC, Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases is licensed under CC BY 4.0
Resource 08 – Reported cases of Lyme disease- United States 2017. Although Lyme disease has been reported in every part of the US, the vast number of cases occur in the northeast. – “Reported cases of Lyme disease” by CDC, Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases is licensed under CC BY 4.0
Resource 09 – Relative sizes of ticks at different life stages. – “Transmission of Lyme disease” by CDC, Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases is licensed under CC BY 4.0
Resource 10 – Bulls-eye rash associated with Lyme disease. – “File:Erythema migrans – erythematous rash in Lyme disease – PHIL 9875.jpg” by CDC/ James Gathany, Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases is in the Public Domain
Resource11 – Later signs and symptoms, which can occur days to months after the tick bite – “Signs and Symptoms of Untreated Lyme Disease” by CDC, Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases is in the Public Domain
Resource 12 – “Viruses” by Khan Academy is licensed under Fair Use
Resource 13 – A simplified diagram of the Hepatitis C virus replication cycle. – “File:HepC replication.png” by GrahamColm is in the Public Domain
Resource 14 – Simplistic overview of the main viral infections and the most notable involved species – “File:Viral infections and involved species.png” by Mikael Häggström is in the Public Domain
Resource 15 – This photograph depicts the face of a young boy with measles, which was captured on the third day of its characteristic rash. – “the face of a young boy with measles” by CDC, Centers for Disease Control and Prevention, Office of the Associate Director for Communications, Division of Public Affairs is in the Public Domain
Resource 16 – This image depicts an intraoral view of a patient, who had presented to a clinical setting exhibiting redness and edema of the oropharynx, and small red spots, on the soft palate mucosa. A diagnosis of Koplik’s spots on the soft palate and oropharynx was made, due to pre-eruptive measles, on day-3 of the illness. – “an intraoral view of a patient, who had presented to a clinical setting exhibiting redness and edema of the oropharynx” by CDC, Centers for Disease Control and Prevention, Office of the Associate Director for Communications, Division of Public Affairs is in the Public Domain
Resource 17 – Mumps Cases and Outbreaks – “Mumps Cases and Outbreaks” by CDC, Centers for Disease Control and Prevention, Office of the Associate Director for Communications, Division of Public Affairs is in the Public Domain
Resource 18 – This image depicts a child with a mumps infection. Note the characteristic swollen neck region due to an enlargement of the boy’s salivary glands. – “a child with a mumps infection” by CDC, Centers for Disease Control and Prevention, Office of the Associate Director for Communications, Division of Public Affairs is in the Public Domain
Resource 19 – Lesions caused by the Hand, Foot and Mouth Virus on a 11 month old male. – “File:Hand Foot Mouth Disease.png” by MidgleyDJ is licensed under CC BY-SA 3.0
Resource 20 – Lesions caused by the Hand, Foot and Mouth Virus on a 36 year old male. – “File:Hand Foot Mouth Disease Adult 36Years.jpg” by KlatschmohnAcker is licensed under CC BY-SA 3.0
Resource 21 – Malaria, Life Cycle of the Malaria Parasite – “File:Life Cycle of the Malaria Parasite.jpg”National Institutes of Health (NIH) is in the Public Domain
Resource 22 – “File:Scabies-burrow.jpg” by Michael Geary is in the Public Domain
Resource 23 – https://my.clevelandclinic.org/health/drugs/21715-antifungals

