Chapter 18: Renal and Urinary Systems
Learning Objectives
After completing this chapter, the learner should be able to:
- Define the basic terminology associated with conditions of the renal and urinary systems.
- Discuss risk factors, etiologic factors, pathogenesis, and clinical manifestations for renal and urinary conditions, including:
- Urinary incontinence
- Urinary tract infection
- Kidney stones
- Polycystic kidney disease
- Kidney failure
- Describe medical, surgical, and physical therapy interventions associated with renal and urinary conditions.
- Describe the pharmacological management of renal and urinary conditions.
- Discuss precautions, indications, and contraindications to be considered in physical therapy interventions for patients with renal and urinary conditions.
Chapter Contents
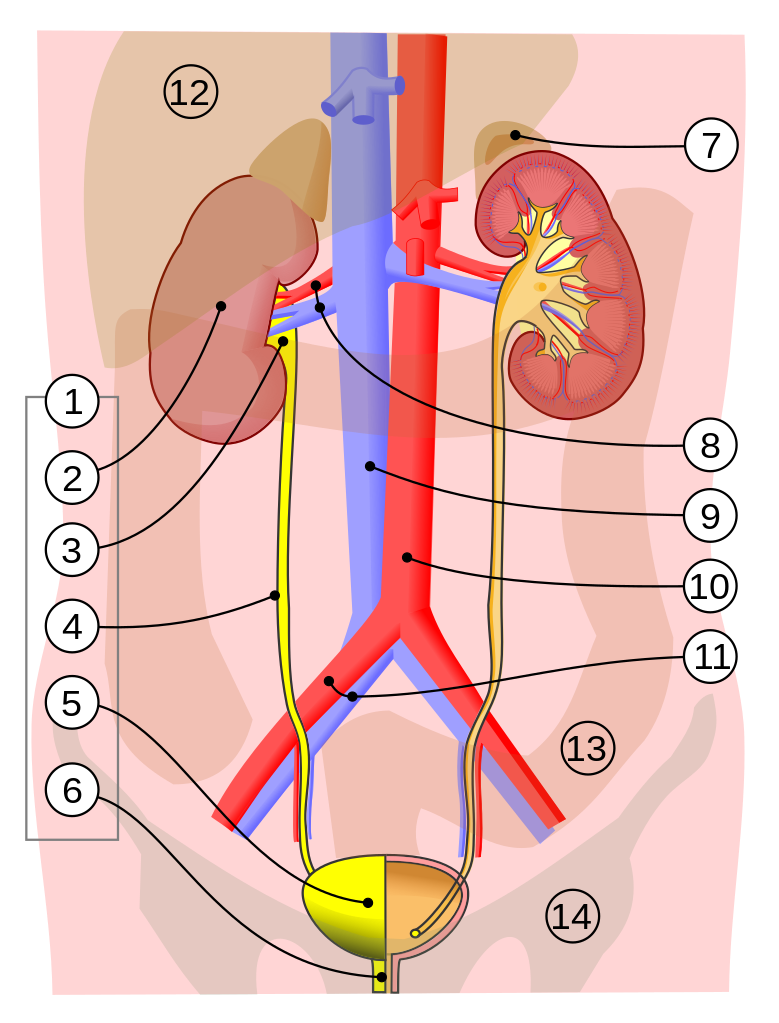
18.0 Organs and Structures
The urinary system, or renal system, functions to filter the blood and remove waste products from the body in urine. Blood is filtered through an elegant capillary system in the kidneys where waste products and excess fluid are removed. Kidney function is also important to regulate the sodium and potassium balance in the body, which has a direct effect on blood pressure. The kidneys are responsible for the production of erythropoietin, which controls red blood cell production in the bone marrow. The acid-base balance of the blood is controlled by the kidneys. The elimination of and conservation of fluids are also important kidney functions. Kidney function is vital to health and poorly functioning kidneys can lead to many different signs, symptoms, and dysfunctions.
General signs and symptoms of renal disease or dysfunction include overproduction or underproduction of urine, a change in urinary habits, abnormal coloration of urine, hypertension, fluid retention (lower extremity edema), shortness of breath, fatigue, confusion, nausea, weakness, cardiac arrhythmia, and back pain.
18.1 Urinary Incontinence
Urinary incontinence affects many people, women more often than men. It can be associated with other medical diagnoses such as serious neurological or neuromuscular conditions, but often it occurs in people not affected by serious conditions. Risk factors for urinary incontinence are included in the box.
Risk Factors for Urinary IncontinenceFemale: vaginal delivery in childbirth; pregnancy; hysterectomy
Male: enlarged prostate and/or prostate surgery
Age: risk increases with age
Obesity: risk increases with increased body weight
18.2 Urinary Tract Infections
Urinary tract infections (UTIs) are quite common in women. Fortunately, most are successfully treated with antibiotics. For a good overview of UTI, watch the following video:
Video:18.2 – 2 Source: YouTube
After watching the video, answer the following questions:
18.2.1 Complications of UTI
Urinary tract infections are generally responsive to antibiotics and are treated in a short period of time. Left untreated, UTI can lead to serious complications, including:
urosepsis: infection beginning in the urinary tract and spreading to other body parts via the blood stream; serious condition that can be fatal
systemic inflammatory response syndrome (SIRS): widespread inflammation that can lead to multi-organ failure and death
chronic kidney infection: can lead to long-term kidney damage and diminished urinary function
18.2.2 UTI and Physical Therapy
Patients can receive some helpful education and training in a physical therapy program for urinary issues, including UTI. Pelvic floor strengthening exercises (Kegels) are used to improve muscle tone and muscular control of the pelvic floor, including urinary sphincters and supportive musculature. Patients can be taught to control pelvic musculature through muscle re-education techniques. Breathing control and relaxation techniques can help in relieving tension in sphincters and related musculature to allow urine flow and urinary bladder emptying. Patient education can also include information on hygiene (women should wipe front to back; urination after sexual intercourse can help clean the lower urinary tract of potential infectious pathogens), diet (drinking plenty of fluids, particularly water), and symptom relief (hot packs on the back or pelvis (not to be used during pregnancy)). PTs and PTAs should reinforce healthy urinary habits in all patients and should attend to potential problems with urinary catheters, such as full urine bags or kinks in the tubing. PTs and PTAs should not empty urine bags without permission, as sometimes urinary output needs to be measured and tracked.
Image and Video Resources:
Section 18.0
Image 1: 18.0 – 1. Urinary system 2. Kidney 3. Renal pelvis 4. Ureter 5. Urinary bladder 6. Urethra (Left side with frontal section) 7. Adrenal gland 8. Renal artery and vein 9. Inferior vena cava 10. Abdominal aorta 11. Common iliac artery and vein 12. Liver 13. Large intestine 14. Pelvis. “Urinary system image” by Jordi March i Nogué is licensed under CC BY-SA 3.0. Wikipedia: Urinary system
Section 18.2
Video: 2 Source: YouTube
General Resources
Johns Hopkins Medicine: Anatomy of the Urinary System
National Institute of Diabetes and Digestive and Kidney Diseases: Urinary Tract: How it Works
Mayo Clinic: Urinary Tract Infection: Symptoms and Causes
Physio-Pedia: Urinary Tract Infection

