10.2 – Fat-Soluble Vitamins
Learning Objectives
- Explore the functions and dietary sources of fat-soluble vitamins.
- Describe the risks associated with deficiencies and excesses of fat-soluble vitamins.
Vitamin A Functions and Health Benefits
Vitamin A is a generic term for a group of similar compounds called retinoids. Retinol is the form of vitamin A found in animal-derived foods and is converted in the body to the biologically active forms of vitamin A: retinal and retinoic acid (thus retinol is sometimes referred to as “preformed vitamin A”). About 10 percent of plant-derived carotenoids, including beta-carotene, can be converted in the body to retinoids and are another source of functional vitamin A. Carotenoids are pigments synthesized by plants that give them their yellow, orange, and red color. Over six hundred carotenoids have been identified and, with just a few exceptions, all are found in the plant kingdom. There are two classes of carotenoids—the xanthophylls, which contain oxygen, and the carotenes, which do not.
In plants, carotenoids absorb light for use in photosynthesis and act as antioxidants. Beta-carotene, alpha-carotene, and beta-cryptoxanthin are converted to some extent to retinol in the body. The other carotenoids, such as lycopene, are not. Many biological actions of carotenoids are attributed to their antioxidant activity, but they likely act by other mechanisms, too.
Vitamin A is fat-soluble and is packaged into chylomicrons in the small intestine, and transported to the liver. The liver stores and exports vitamin A as needed; it is released into the blood and is transported to cells. Carotenoids are not absorbed as well as vitamin A, but similar to vitamin A, they do require fat in the meal for absorption. In intestinal cells, carotenoids are packaged into the lipid-containing chylomicrons and then transported to the liver. In the liver, carotenoids are repackaged into lipoproteins, which transport them to cells.
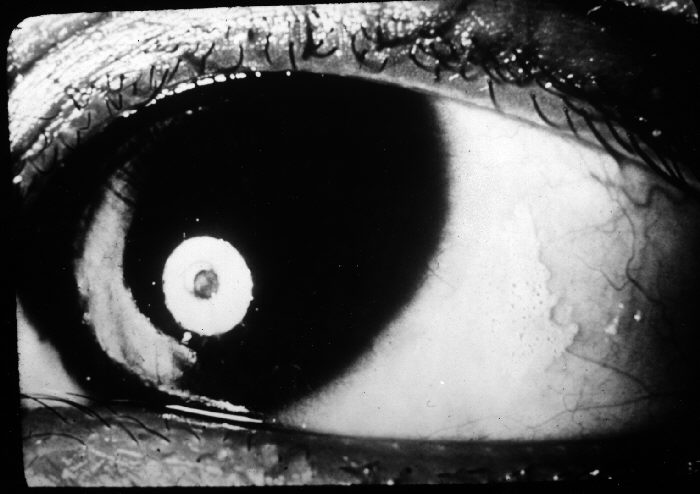
The retinoids are aptly named as their most notable function is in the retina of the eye where they aid in vision, particularly in seeing under low-light conditions. This is why night blindness is the most definitive sign of vitamin A deficiency. Vitamin A has several important functions in the body, including maintaining vision and a healthy immune system. Many of vitamin A’s functions in the body are similar to the functions of hormones (for example, vitamin A can interact with DNA, causing a change in protein function). Vitamin A assists in maintaining healthy skin and the linings and coverings of tissues; it also regulates growth and development. As an antioxidant, vitamin A protects cellular membranes, helps in maintaining glutathione levels, and influences the amount and activity of enzymes that detoxify free radicals.
Vision
Retinol that is circulating in the blood is taken up by cells in the eye retina, where it is converted to retinal and is involved in the eye’s ability to see under low light conditions. A deficiency in vitamin A thus results in a decrease in the detection of low-level light, a condition referred to as night-blindness.
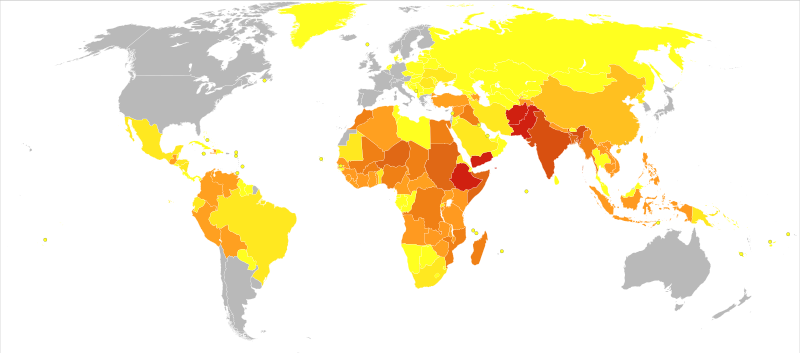
Insufficient intake of dietary vitamin A over time can also cause complete vision loss. In fact, vitamin A deficiency is the number one cause of preventable blindness worldwide. Vitamin A not only supports the vision function of eyes but also maintains the coverings and linings of the eyes. Vitamin A deficiency can lead to the dysfunction of the linings and coverings of the eye (eg. bitot spots), causing dryness of the eyes, a condition called xerophthalmia. The progression of this condition can cause ulceration of the cornea and eventually blindness.
| 0 to 28 | 31 to 78 | 85 to 85 | 85 to 141 | 144 to 257 | 258 to 376 | 432 to 455 | 558 to 558 | 586 to 883 |
|---|---|---|---|---|---|---|---|---|
Immunity
The common occurrence of advanced xerophthalmia in children who died from infectious diseases led scientists to hypothesize that supplementing vitamin A in the diet for children with xerophthalmia might reduce disease-related mortality. In Asia in the late 1980s, targeted populations of children were administered vitamin A supplements, and the death rates from measles and diarrhea declined by up to 50 percent. Vitamin A supplementation in these deficient populations did not reduce the number of children who contracted these diseases, but it did decrease the severity of the diseases so that they were no longer fatal. Soon after the results of these studies were communicated to the rest of the world, the World Health Organization (W.H.O.) and the United Nations Children’s Fund (U.N.I.C.E.F.) commenced worldwide campaigns against vitamin A deficiency. U.N.I.C.E.F. estimates that the distribution of over half a billion vitamin A capsules prevents 350,000 childhood deaths annually.1
In the twenty-first century, science has demonstrated that vitamin A greatly affects the immune system. What we are still lacking are clinical trials investigating the proper doses of vitamin A required to help ward off infectious disease and how large of an effect vitamin A supplementation has on populations that are not deficient in this vitamin. This brings up one of our common themes in this text—micronutrient deficiencies may contribute to the development, progression, and severity of a disease, but this does not mean that an increased intake of these micronutrients will solely prevent or cure disease. The effect, as usual, is cumulative and depends on the diet as a whole, among other things.
1 Sommer A. Vitamin A Deficiency and Clinical Disease: An Historical Overview. J Nutr. 2008; 138, 1835–39. http://jn.nutrition.org/content/138/10/1835.long. Accessed June 30, 2019.
Growth and Development
Vitamin A acts similarly to some hormones in that it is able to change the number of proteins in cells by interacting with DNA. This is the primary way that vitamin A affects growth and development. Vitamin A deficiency in children is linked to growth retardation; however, vitamin A deficiency is often accompanied by protein malnutrition and iron deficiency, thereby confounding the investigation of vitamin A’s specific effects on growth and development.
In the fetal stages of life, vitamin A is important for limb, heart, eye, and ear development and in both deficiency and excess, vitamin A causes birth defects. Furthermore, both males and females require vitamin A in the diet to effectively reproduce.
Cancer
Vitamin A’s role in regulating cell growth and death, especially in tissues that line and cover organs, suggests it may be effective in treating certain cancers of the lung, neck, and liver. It has been shown in some observational studies that vitamin A-deficient populations have a higher risk for some cancers. However, vitamin A supplements have actually been found to increase the risk of lung cancer in people who are at high risk for the disease (i.e., smokers, ex-smokers, workers exposed to asbestos). The Beta-Carotene and Retinol Efficacy Trial (C.A.R.E.T.) involving over eighteen thousand participants who were at high risk for lung cancer found that people who took supplements containing very high doses of vitamin A (25,000 international units) and beta-carotene had a 28 percent higher incidence of lung cancer midway through the study, which was consequently stopped.2
2 Goodman GE, et al. The Beta-Carotene and Retinol Efficacy Trial: Incidence of Lung Cancer and Cardiovascular Disease Mortality During 6-year Follow-up after Stopping Beta-Carotene and Retinol Supplements. J Natl Cancer Inst. 2004; 96(23), 1743–50. http://jnci.oxfordjournals.org/content/96/23/1743.long. Accessed June 30, 2019.
Vitamin A Toxicity
Vitamin A toxicity, or hypervitaminosis A, is rare. Typically it requires you to ingest ten times the R.D.A. of preformed vitamin A in the form of supplements (it would be hard to consume such high levels from a regular diet) for a substantial amount of time, although some people may be more susceptible to vitamin A toxicity at lower doses. The signs and symptoms of vitamin A toxicity include dry, itchy skin, loss of appetite, swelling of the brain, and joint pain. In severe cases, vitamin A toxicity may cause liver damage and coma.
Vitamin A is essential during pregnancy, but doses above 3,000 micrograms per day (10,000 international units) have been linked to an increased incidence of birth defects. Pregnant women should check the amount of vitamin A contained in any prenatal or pregnancy multivitamin she is taking to assure the amount is below the U.L..
Dietary Reference Intakes for Vitamin A
There is more than one source of vitamin A in the diet. There is preformed vitamin A, which is abundant in many animal-derived foods, and there are carotenoids, which are found in high concentrations in vibrantly colored fruits and vegetables and some oils.
Some carotenoids are converted to retinol in the body by intestinal cells and liver cells. However, only minuscule amounts of certain carotenoids are converted to retinol, meaning fruits and vegetables are not necessarily good sources of vitamin A.
The R.D.A. for vitamin A includes all sources of vitamin A. The R.D.A. for vitamin A is given in mcg of retinol activity requirements (R.A.E.) to take into account the many different forms it is available in. The human body converts all dietary sources of vitamin A into retinol. Therefore, 1 mcg of retinol is equivalent to 12 mcg of beta-carotene, and 24 mcg of alpha-carotene or beta-cryptoxanthin. For example, 12 micrograms of fruit- or vegetable-based beta-carotene will yield 1 microgram of retinol. Currently, vitamin A listed in food and on supplement labels use international units (I.U.s). The following conversions are listed below3:
- 1 I.U. retinol = 0.3 mcg R.A.E.
- 1 I.U. beta-carotene from dietary supplements = 0.15 mcg R.A.E.
- 1 I.U. beta-carotene from food = 0.05 mcg R.A.E.
- 1 I.U. alpha-carotene or beta-cryptoxanthin = 0.025 mcg R.A.E.
The R.D.A. for vitamin A is considered sufficient to support growth and development, reproduction, vision, and immune system function while maintaining adequate stores (good for four months) in the liver.
3 Dietary Supplement Fact Sheet: Vitamin A. National Institutes of Health, Office of Dietary Supplements.. Updated October 5, 2018. Accessed June 30, 2019.
Table 10.2.1: Dietary Reference Intakes for Vitamin A.
| Age Group | R.D.A. Males and Females (micrograms R.A.E. per Day) | |
|---|---|---|
| Infants (0–6 months) | 400* | 600 |
| Infants (7–12 months) | 500* | 600 |
| Children (1–3 years) | 300 | 600 |
| Children (4–8 years) | 400 | 900 |
| Children (9–13 years) | 600 | 1,700 |
| Adolescents (14–18 years) | Males: 900 | 2,800 |
| Adolescents (14–18 years) | Females: 700 | 2,800 |
| Adults (> 19 years) | Males: 900 | 3,000 |
| Adults (> 19 years) | Females: 700 | 3,000 |
*Denotes adequate intake*
Dietary Sources of Vitamin A and Beta-Carotene
Preformed vitamin A is found only in foods from animals, with the liver being the richest source because that’s where vitamin A is stored (see Table 10.2.2). The dietary sources of carotenoids will be given in the following text.
Table 10.2.2: Vitamin A Content of Various Foods
| Food | Serving | Vitamin A (I.U.) | Percent Daily Value |
|---|---|---|---|
| Beef liver | 3 oz. | 27,185 | 545 |
| Chicken liver | 3 oz. | 12,325 | 245 |
| Milk, skim | 1 c. | 500 | 10 |
| Milk, whole | 1 c. | 249 | 5 |
| Cheddar cheese | 1 oz. | 284 | 6 |
Source: Dietary Supplement Fact Sheet: Vitamin A. National Institutes of Health, Office of Dietary Supplements. Updated September 5, 2012. Accessed October 7, 2017.
In the United States, the most consumed carotenoids are alpha-carotene, beta-carotene, beta-cryptoxanthin, lycopene, lutein, and zeaxanthin. See Table 10.2.3 for the carotenoid content of various foods.
Table 10.2.3: Vitamin A Content of Various Foods
| Food | Serving | Vitamin A (I.U.) | Percent Daily Value |
|---|---|---|---|
| Pumpkin, canned | 1c. | 17.00 | 11.70 |
| Carrot juice | 1c. | 22.00 | 10.20 |
| Carrots, cooked | 1c. | 13.00 | 5.90 |
| Carrots, raw | 1 medium | 5.10 | 2.10 |
| Winter squash, baked | 1c. | 5.70 | 1.40 |
| Collards, cooked | 1c. | 11.60 | 0.20 |
| Tomato | 1 medium | 0.55 | 0.10 |
| Tangerine | 1 medium | 0.13 | 0.09 |
| Peas, cooked | 1c. | 1.20 | 0.09 |
Vitamin D Functions and Health Benefits
Vitamin D refers to a group of fat-soluble vitamins derived from cholesterol. Vitamins D2 (ergocalciferol) and D3 (calcitriol) are the only ones known to have biological actions in the human body. The skin synthesizes vitamin D when exposed to sunlight. In fact, for most people, more than 90 percent of their vitamin D3 comes from casual exposure to the U.V.B. rays in sunlight. Anything that reduces your exposure to the sun’s U.V.B. rays decreases the amount of vitamin D3 your skin synthesizes. That would include long winters, your home’s altitude, whether you are wearing sunscreen, and the color of your skin (including tanned skin). Do you ever wonder about an increased risk of skin cancer by spending too much time in the sun? Do not fret. Less than thirty minutes of sun exposure to the arms and legs will increase blood levels of vitamin D3 more than orally taking 10,000 I.U. (250 micrograms) of vitamin D3.
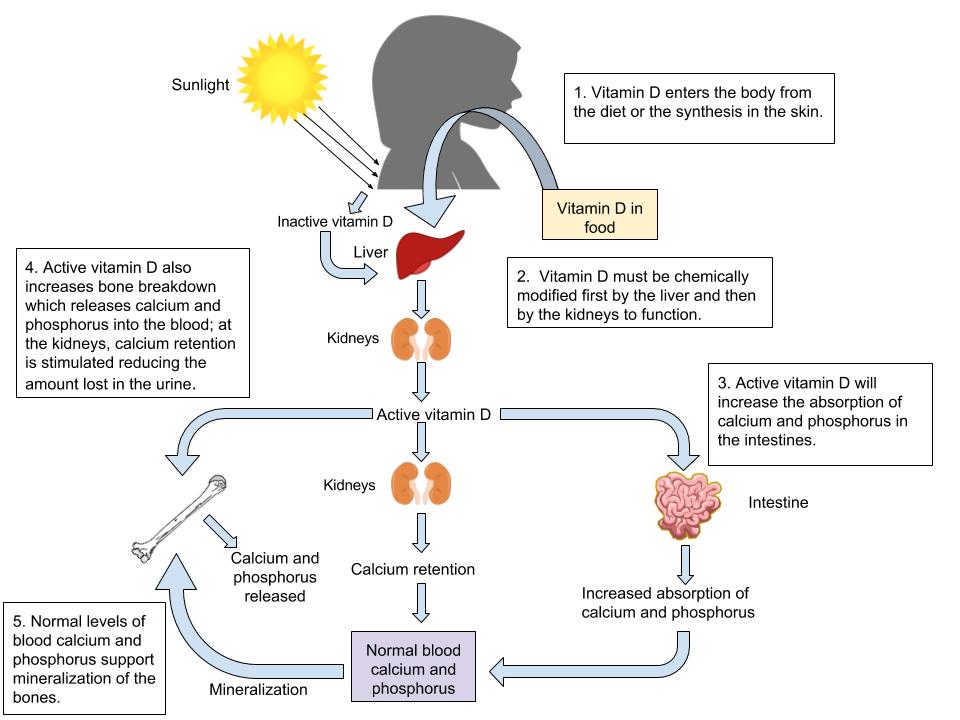
Vitamin D’s Functional Role
Activated vitamin D3 (calcitriol) regulates blood calcium levels in concert with parathyroid hormone. In the absence of an adequate intake of vitamin D, less than 15 percent of calcium is absorbed from foods or supplements. The effects of calcitriol on calcium status are critical for bone health. A deficiency of vitamin D in children causes a bone disease called nutritional rickets. Rickets is very common among children in developing countries and is characterized by soft, weak, deformed bones that are exceptionally susceptible to fracture. causes a similar disease called osteomalacia, which is characterized by low bone mineral density (B.M.D.). Osteomalacia has the same symptoms and consequences as osteoporosis and often coexists with osteoporosis. Vitamin D deficiency may be common in the population, especially in the elderly population, dark-skinned populations, and in the many people who live in the northern latitudes where sunlight exposure is much decreased during the long winter season.

Health Benefits
Observational studies have shown that people with low levels of vitamin D in their blood have lower bone mineral density and an increased incidence of osteoporosis. In contrast, diets with high intakes of salmon, which contains a large amount of vitamin D, are linked with better bone health. Unfortunately, the current evidence doesn’t demonstrate an improvement of bone density with the use of large dose Vitamin D supplements. 4 Unless diagnosed by a physician, safe sun exposure (10-30 minutes of mid-day sun on the arms and legs two to three times per week)and food sources of Vitamin D are your best plan of action.
Many other health benefits have been linked to vitamin D, from decreased cardiovascular disease to the prevention of infection. Furthermore, evidence from laboratory studies conducted in cells, tissues, and animals suggest vitamin D prevents the growth of certain cancers, blocks inflammatory pathways, reverses atherosclerosis, increases insulin secretion, and blocks viral and bacterial infection and many other things. Vitamin D deficiency has been linked to an increased risk of autoimmune diseases. Immune diseases, rheumatoid arthritis, multiple sclerosis, and Type 1 diabetes have been observed in populations with inadequate vitamin D levels. Additionally, vitamin D deficiency is linked to an increased incidence of hypertension. Until the results come out from the VITAL study, the bulk of scientific evidence touting other health benefits of vitamin D is from laboratory and observational studies and requires confirmation in clinical intervention studies. Again, this is an example of how what we see in observational and lab studies may not relate to interventional studies. To date, interventional studies have been inconclusive regarding supplementation and these other potential roles of Vitamin D in the body.
4 Bolland, MJ, Grey, A, and Avenell, A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes & Endocrinology.2018; 6 (11), 847-858. Accessed June 30, 2019.
Vitamin D Toxicity
Although vitamin D toxicity is rare, too much can cause high levels of calcium concentrations or hypercalcemia. Hypercalcemia can lead to a large amount of calcium to be excreted through the urine which can cause kidney damage. Calcium deposits may also develop in soft tissues such as the kidneys, blood vessels, or other parts of the cardiovascular system. However, it is important to know that the synthesis of vitamin D from the sun does not cause vitamin D toxicity due to the skin production of vitamin D3 being a tightly regulated process.
Dietary Reference Intake for Vitamin D
The Institute of Medicine R.D.A.s for vitamin D for different age groups is listed in Table 10.2.4. For adults, the R.D.A. is 600 international units (I.U.s), which is equivalent to 15 micrograms of vitamin D. The National Osteoporosis Foundation recommends slightly higher levels and that adults under age fifty get between 400 and 800 international units of vitamin D every day, and adults fifty and older get between 800 and 1,000 international units of vitamin D every day. According to the I.O.M., the tolerable upper intake level (U.L.) for vitamin D is 4,000 international units per day. Toxicity from excess vitamin D is rare, but certain diseases such as hyperparathyroidism, lymphoma, and tuberculosis make people more sensitive to the increases in calcium caused by high intakes of vitamin D.
Table 10.2.4: Dietary Reference Intakes for Vitamin D.
| Age Group | R.D.A. (m.c.g. Per Day) | U.L. (m.c.g. Per Day) |
|---|---|---|
| Infant (0–6 months) | 10* | 25 |
| Infants (6–12 months) | 10* | 25 |
| Children (1–3 years) | 15 | 50 |
| Children (4–8 years) | 15 | 50 |
| Children (9–13 years) | 15 | 50 |
| Adolescents (14–18 years) | 15 | 50 |
| Adults (19–71 years) | 15 | 50 |
| Adults (> 71 years) | 20 | 50 |
*Denotes adequate intake*
Table 10.2.5: Dietary Sources of Vitamin D.
| Food | Serving Size | Vitamin D (I U) | Percent Daily Value |
|---|---|---|---|
| Swordfish | 3 oz. | 566 | 142 |
| Salmon | 3 oz. | 447 | 112 |
| Tuna fish, canned in water, drained | 3 oz. | 154 | 39 |
| Orange juice fortified with vitamin D | 1 c. | 137 | 34 |
| Milk, nonfat, reduced fat, and whole, vitamin D- fortified | 1 c. | 115-124 | 29-31 |
| Margarine, fortified | 1 tbsp. | 60 | 15 |
| Sardines, canned in oil, drained | 2 e. | 46 | 12 |
| Beef liver | 3 oz. | 42 | 11 |
| Egg, large | 1 e. | 41 | 10 |
Vitamin E Functions and Health Benefits
Vitamin E occurs in eight chemical forms, of which alpha-tocopherol appears to be the only form that is recognized to meet human requirements. Alpha-tocopherol and vitamin E’s other constituents are fat-soluble and primarily responsible for protecting cell membranes against lipid destruction caused by free radicals, therefore making it an antioxidant. When alpha-tocopherol interacts with a free radical it is no longer capable of acting as an antioxidant unless it is enzymatically regenerated. Vitamin C helps to regenerate some of the alpha-tocopherol, but the remainder is eliminated from the body. Therefore, to maintain vitamin E levels, you must ingest it as part of your diet.
Insufficient levels are rare (signs and symptoms of such conditions are not always evident) but are primarily the result of nerve degeneration. People with malabsorption disorders, such as Crohn’s disease or cystic fibrosis, and babies born prematurely, are at higher risk for vitamin E deficiency.
Vitamin E has many other important roles and functions in the body such as boosting the immune system by helping to fight off bacteria and viruses. It also enhances the dilation of blood vessels and inhibits the formation of blood clotting. Despite vitamin E’s numerous beneficial functions when taken in recommended amounts, large studies do not support the idea that taking higher doses of this vitamin will increase its power to prevent or reduce disease risk.5,6
Fat in the diet is required for vitamin E absorption as it is packaged into lipid-rich chylomicrons in intestinal cells and transported to the liver. The liver stores some of the vitamin E or packages it into lipoproteins, which deliver it to cells.
5 Goodman M, Bostlick RM, Kucuk O, Jones DP. Clinical trials of antioxidants as cancer prevention agents: past, present, and future. Free Radic Biol Med. 2011; 51(5), 1068–84. https://www.ncbi.nlm.nih.gov/pubmed/21683786. Accessed June 30, 2019.
6 McGinley C, Shafat A. Donnelly AE. Does antioxidant vitamin supplementation protect against muscle damage? Sports Med. 2009; 39(12), 1011–32. https://www.ncbi.nlm.nih.gov/pubmed/19902983. Accessed June 30, 2019.
Cardiovascular Disease
Vitamin E reduces the oxidation of LDLs, and it was therefore hypothesized that vitamin E supplements would protect against atherosclerosis. However, large clinical trials have not consistently found evidence to support this hypothesis. In fact, in the “Women’s Angiographic Vitamin and Estrogen Study,” postmenopausal women who took 400 international units (264 milligrams) of vitamin E and 500 milligrams of vitamin C twice per day had higher death rates from all causes.7
Other studies have not confirmed the association between increased vitamin E intake from supplements and increased mortality. There is more consistent evidence from observational studies that a higher intake of vitamin E from foods is linked to a decreased risk of dying from a heart attack.
7 Waters DD, et al. Effects of Hormone Replacement Therapy and Antioxidant Vitamin Supplements on Coronary Atherosclerosis in Postmenopausal Women: A Randomized Controlled Trial. JAMA. 2002; 288(19), 2432–40. https://jamanetwork.com/journals/jama/fullarticle/195531. Accessed June 30, 2019.
Cancer
The large clinical trials that evaluated whether there was a link between vitamin E and cardiovascular disease risk also looked at cancer risk. These trials called the HOPE-TOO Trial and Women’s Health Study, did not find that vitamin E at doses of 400 international units (264 milligrams) per day or 600 international units (396 milligrams) every other day reduced the risk of developing any form of cancer. 8,9
8 Lonn, E. et al. HOPE and HOPE-TOO Trial Investigators. Effects of Long-Term Vitamin E Supplementation on Cardiovascular Events and Cancer. JAMA. 2005; 293, 1338–47. http://jama.ama-assn.org/content/293/11/1338.long., Accessed June 30, 2019.
9 Lee IM, et al. Vitamin E in the Primary Prevention of Cardiovascular Disease and Cancer: The Women’s Health Study. JAMA.2005; 294, 56–65. http://jama.ama-assn.org/content/294/1/56.long. Accessed June 30, 2019.
Eye Conditions
Oxidative stress plays a role in age-related loss of vision, called macular degeneration. Age-related macular degeneration (A.M.D.) primarily occurs in people over age fifty and is the progressive loss of central vision resulting from damage to the center of the retina, referred to as the macula. There are two forms of A.M.D., dry and wet, with wet being the more severe form.
In the dry form, deposits form in the macula; the deposits may or may not directly impair vision, at least in the early stages of the disease. In the wet form, abnormal blood vessel growth in the macula causes vision loss. Clinical trials evaluating the effects of vitamin E supplements on A.M.D. and cataracts (clouding of the lens of an eye) did not consistently observe a decreased risk for either. However, scientists do believe vitamin E in combination with other antioxidants such as zinc and copper may slow the progression of macular degeneration in people with early-stage disease.
Dementia
The brain’s high glucose consumption makes it more vulnerable than other organs to oxidative stress. Oxidative stress has been implicated as a major contributing factor to dementia and Alzheimer’s disease. Some animal and non-interventional studies suggest vitamin E supplements might have a role in the prevention or treatment of Alzheimer’s disease and cognitive decline. However, a 2017 Cochrane review, concluded that to date the interventional trials did not reduce the number of people who developed dementia with the addition of Vitamin E.
More studies are needed to better assess the dose and dietary requirements of vitamin E and, for that matter, whether other antioxidants lower the risk of dementia, a disease that not only devastates the mind, but also puts a substantial burden on loved ones, caretakers, and society in general.10
10 Farina N, Llewellyn D, Isaac M, Tabet N. Vitamin E for Alzheimer’s dementia and mild cognitive impairment. Cochrane Database of Systematic Reviews 2017, Issue 4. Art. No.: CD002854. DOI: 10.1002/14651858.CD002854.pub5 Accessed May 24, 2019
Vitamin E Toxicity
Currently, researchers have not found any adverse effects from consuming vitamin E in food. Although that may be the case, supplementation of alpha-tocopherol in animals has shown to cause hemorrhage and disrupt blood coagulation. Extremely high levels of vitamin E can interact with vitamin K-dependent clotting factors causing inhibition of blood clotting.11
Vitamin E supplements often contain more than 400 international units, which is almost twenty times the R.D.A.. The U.L. for vitamin E is set at 1,500 international units for adults. There is some evidence that taking vitamin E supplements at high doses has negative effects on health. As mentioned, vitamin E inhibits blood clotting and a few clinical trials have found that people taking vitamin E supplements have an increased risk of stroke. In contrast to vitamin E from supplements, there is no evidence that consuming foods containing vitamin E compromises health.
Dietary Reference Intakes for Vitamin E
The Recommended Dietary Allowances (R.D.A.s) and Tolerable Upper Intake Levels (U.L.s) for different age groups for vitamin E are given in Table 10.2.6.
Table 10.2.6: Dietary Reference Intakes for Vitamin E.
| Age Group | R.D.A. Males and Females (m.g. Per Day) | U.L. |
|---|---|---|
| Infants (0–6 months) | 4* | None |
| Infants (7–12 months) | 5* | None |
| Children (1–3 years) | 6 | 200 |
| Children (4–8 years) | 7 | 300 |
| Children (9–13 years) | 11 | 600 |
| Adolescents (14–18 years) | 15 | 800 |
| Adults (> 19 years) | 15 | 1,000 |
Dietary Sources of Vitamin E
Add some nuts to your salad and make your own dressing to get a healthy dietary dose of vitamin E.

Vitamin E is found in many foods, especially those higher in fat, such as nuts and oils. Some spices, such as paprika and red chili pepper, and herbs, such as oregano, basil, cumin, and thyme, also contain vitamin E. (Keep in mind spices and herbs are commonly used in small amounts in cooking and therefore are a lesser source of dietary vitamin E.) See Table 10.2.7 for a list of foods and their vitamin E contents.
Everyday Connection
To increase your dietary intake of vitamin E from plant-based foods try a spinach salad with tomatoes and sunflower seeds, and add a dressing made with sunflower oil, oregano, and basil.
Table 10.2.7: Dietary Sources of Vitamin E.
| Food | Serving Size | Vitamin E (M G) | Percent Daily Value |
|---|---|---|---|
| Sunflower seeds | 1 oz. | 7.4 | 37 |
| Almonds | 1 oz. | 6.8 | 34 |
| Sunflower oil | 1 Tbsp | 5.6 | 28 |
| Hazelnuts 1 oz. | 1 oz. | 4.3 | 22 |
| Peanut butter | 2 Tbsp. | 2.9 | 15 |
| Peanuts 1 oz. | 1 oz. | 2.2 | 11 |
| Corn oil 1 Tbsp. | 1 Tbsp. | 1.9 | 10 |
| Kiwi | 1 medium | 1.1 | 6 |
| Tomato | 1 medium | 0.7 | 4 |
| Spinach | 1 c. raw | 0.6 | 3 |
Vitamin K Functions and Health Benefits
Vitamin K refers to a group of fat-soluble vitamins that are similar in chemical structure. Vitamin K is critical for blood function acting as coenzymes which play an essential role in blood coagulation (aka blood clotting). Blood-clotting proteins are continuously circulating in the blood. Upon injury to a blood vessel, platelets stick to the wound forming a plug. Without vitamin K, blood would not clot.
A deficiency in vitamin K causes bleeding disorders. It is relatively rare, but people who have liver or pancreatic disease, celiac disease, or malabsorption conditions are at higher risk for vitamin K deficiency. Signs and symptoms include nosebleeds, easy bruising, broken blood vessels, bleeding gums, and heavy menstrual bleeding in women. The function of the anticoagulant drug warfarin is impaired by excess vitamin K intake from supplements. Calcium additionally plays a role in the activation of blood-clotting proteins.
Bone Health
Vitamin K is also required for maintaining bone health. It modifies the protein osteocalcin, which is involved in the bone remodeling process. All the functions of osteocalcin and the other vitamin K-dependent proteins in bone tissue are not well understood and are under intense study. Some studies do show that people who have diets low in vitamin K also have an increased risk for bone fractures.
Dietary Reference Intake and Food Sources for Vitamin K
The A.I. of vitamin K for adult females is 90 micrograms per day, and for males, it is 120 micrograms per day. A U.L. for vitamin K has not been set. The Food and Nutrition Board (F.N.B.) has not established an U.L. for vitamin K because it has a low potential for toxicity. According to the F.N.B., “no adverse effects associated with vitamin K consumption from food or supplements have been reported in humans or animals.”11
11 Institute of Medicine. Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington, DC: National Academy Press; 2001.
Table 10.2.8: Dietary Reference Intakes for Vitamin K.
| Age Group | R.D.A. (micrograms per day) |
|---|---|
| Infants (0–6 months) | 2.0* |
| Infants (6–12 months) | 2.5* |
| Children (1–3 years) | 30 |
| Children (4–8 years) | 55 |
| Children (9–13 years) | 60 |
| Adolescents (14–18 years) | 75 |
| Adult Males (> 19 years) | 120 |
| Adult Females (> 19 years) | 90 |
Dietary Sources of Vitamin K
Vitamin K is present in many foods. It is found in highest concentrations in green vegetables such as broccoli, cabbage, kale, parsley, spinach, and lettuce. Additionally, vitamin K can be synthesized via bacteria in the large intestine. The exact amount of vitamin K synthesized by bacteria that is actually absorbed in the lower intestine is not known, but likely contributes less than 10 percent of the recommended intake. Newborns have low vitamin K stores and it takes time for the sterile newborn gut to acquire the good bacteria it needs to produce vitamin K. So, it has become a routine practice to inject newborns with a single intramuscular or oral dose of vitamin K. This practice had basically eliminated vitamin K-dependent bleeding disorders in babies. In populations where parents refuse this practice, physicians are seeing increased rates of blood clotting problems in newborns.
12 Schulte, R et al. Rise in late-onset vitamin K deficiency bleeding in young infants because of omission or refusal of prophylaxis at birth. Pediatr Neurol. 2014; 50(6):564-8. DOI: 10.1016/j.pediatrneurol.2014.02.013. Accessed June 30, 2019.
Table 10.2.9: Dietary Sources of Vitamin K.
| Food | Serving Size | Vitamin K (Micrograms) | Percent Daily Value |
|---|---|---|---|
| Broccoli | ½ c. | 160 | 133 |
| Asparagus | 4 spears | 34 | 28 |
| Cabbage | ½ c. | 56 | 47 |
| Spinach | ½ c. | 27 | 23 |
| Green peas | ½ c. | 16 | 13 |
| Cheese | 1 oz. | 10 | 8 |
| Ham | 3 oz. | 13 | 11 |
| Ground beef | 3 oz. | 6 | 5 |
| Bread | 1 slice | 1.1 | < 1 |
| Orange | 1 e. | 1.3 | 1 |
Summary of Fat-soluble Vitamins
Table 10.2.10: Fat-soluble Vitamins
| Vitamin | Sources | Recommended Intake for adults | Major functions | Deficiency diseases and symptoms | Groups at risk of deficiency | Toxicity | U.L. |
|---|---|---|---|---|---|---|---|
| Vitamin A (retinol, retinal, retinoic acid, carotene, beta-carotene) | Retinol: beef and chicken liver, skim milk, whole milk, cheddar cheese; Carotenoids: pumpkin, carrots, squash, collards, peas | 700-900 mcg/day | Antioxidant, vision, cell differentiation, reproduction, immune function | Xerophthalmia, night blindness, eye infections; poor growth, dry skin, impaired immune function | People living in poverty (especially infants and children), premature infants, pregnant and lactating women people who consume low-fat or low-protein diets | Hypervitaminosis A: Dry, itchy skin, hair loss, liver damage, joint pain, fractures, birth defects, swelling of the brain | 3000 mcg/day |
| Vitamin D | Swordfish, salmon, tuna, orange juice (fortified), milk (fortified), sardines, egg, synthesis from sunlight | 600-800 I.U./day (15-20 mcg/day) | Absorption and regulation of calcium and phosphorus, maintenance of bone | Rickets in children: abnormal growth, misshapen bones, bowed legs, soft bones; osteomalacia in adults | Breastfed infants, older adults people with limited sun exposure, people with dark skin | Calcium deposits in soft tissues, damage to the heart, blood vessels, and kidneys | 4000 I.U./day (100 mcg/day) |
| Vitamin E | Sunflower seeds, almonds, hazelnuts,peanuts | 15 mg/day | Antioxidant, protects cell membranes | Broken red blood cells, nerve damage | People with poor fat absorption, premature infants | Inhibition of vitamin K clotting factors | 1000 mcg/day from supplemental sources |
| Vitamin K | Vegetable oils, leafy greens, synthesis by intestinal bacteria | 90-120 mcg/day | Synthesis of blood clotting proteins and proteins needed for bone health and cell growth | Hemorrhage | Newborns, people on long term antibiotics | Anemia, brain damage | N D |
key Takeaways
- See the Table above for a summary of the fat-soluble vitamins.
Contributors
University of Hawai’i at Mānoa Food Science and Human Nutrition Program: Allison Calabrese, Cheryl Gibby, Billy Meinke, Marie Kainoa Fialkowski Revilla, and Alan Titchenal

