10.3 – Water-Soluble Vitamins
Learning Objectives
- Explore the functions and dietary sources of water-soluble vitamins.
- Describe the risks associated with deficiencies and excesses of water-soluble vitamins.
Most of the water-soluble vitamins play a different kind of role in energy metabolism; they are required as functional parts of enzymes involved in energy release and storage. Vitamins and minerals that make up a part of enzymes are referred to as coenzymes and cofactors, respectively. Coenzymes and cofactors are required by enzymes to catalyze (speed up) a specific reaction. They assist in converting a substrate to an end-product. Coenzymes and cofactors are essential in catabolic (to breakdown) pathways and play a role in many anabolic (to build up) pathways too. In addition to being essential for metabolism, many vitamins and minerals are required for blood renewal and function. At insufficient levels in the diet these vitamins and minerals impair the health of blood and consequently the delivery of nutrients in and wastes out, amongst its many other functions. In this section we will focus on the vitamins that take part in metabolism and blood function and renewal.

Vitamin C
Vitamin C, also commonly called ascorbic acid, is a water-soluble micronutrient essential in the diet for humans, although most other mammals can readily synthesize it. Vitamin C’s ability to easily donate electrons makes it a highly effective antioxidant. It is effective in scavenging free radicals. It protects lipids both by disabling free radicals and by aiding in the regeneration of vitamin E.
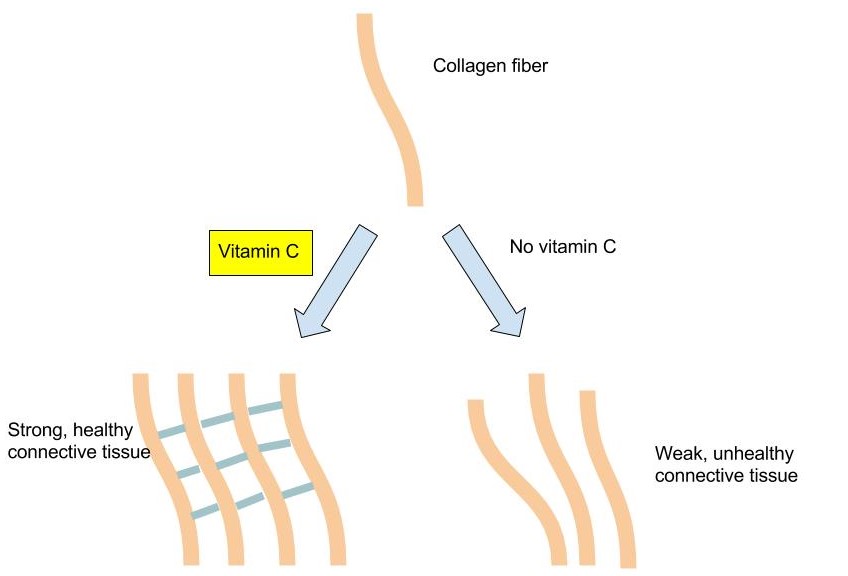
In addition to its role as an antioxidant, vitamin C is a required part of several enzymes like signaling molecules in the brain, some hormones, and amino acids. Vitamin C is also essential for the synthesis and maintenance of collagen. Collagen is the most abundant protein in the body and used for different functions such as the structure for ligaments, tendons, and blood vessels and also scars that bind wounds together. Vitamin C acts as the glue that holds the collagen fibers together and without sufficient levels in the body, collagen strands are weak and abnormal. (Figure 10.3.2 )
Vitamin C levels in the body are affected by the amount in the diet, which influences how much is absorbed and how much the kidney allows to be excreted, such that the higher the intake, the more vitamin C is excreted. Vitamin C is not stored in any significant amount in the body, but once it has reduced a free radical, it is very effectively regenerated and therefore it can exist in the body as a functioning antioxidant for many weeks.
The classic condition associated with vitamin C deficiency is scurvy. The signs and symptoms of scurvy include skin disorders, bleeding gums, painful joints, weakness, depression, and increased susceptibility to infections. Scurvy is prevented by having an adequate intake of fruits and vegetables rich in vitamin C.

Cardiovascular Disease
Vitamin C’s ability to prevent disease has been debated for many years. Overall, higher dietary intakes of vitamin C (via food intake, not supplements), are linked to decreased disease risk. A review of multiple studies published in the January issue of Nutrition Research concludes there is a limited role for vitamin C supplementation in certain population groups (older people, individuals with lower Vitamin C status, those at higher risk of cardiovascular disease) to improve cardiovascular health.1 Vitamin C levels in the body have been shown to correlate well with fruit and vegetable intake, and higher plasma vitamin C levels are linked to a reduced risk of some chronic diseases.
1 Ashor AW et al. Limited evidence for a beneficial effect of vitamin C supplementation on biomarkers of cardiovascular diseases: an umbrella review of systematic reviews and meta-analyses. Nutr Res. 2019. 61,1-12. Accessed June 30, 2019.
Cancer and Vitamin C
There is some evidence that a higher vitamin C intake is linked to a reduced risk of cancers of the mouth, throat, esophagus, stomach, colon, and lung, but not all studies confirm this is true. As with the studies on cardiovascular disease, the reduced risk of cancer is the result of eating foods rich in vitamin C, such as fruits and vegetables, not from taking vitamin C supplements. In these studies, the specific protective effects of vitamin C cannot be separated from the many other beneficial chemicals in fruits and vegetables.
Immunity and Vitamin C
Vitamin C does have several roles in the immune system, and many people increase vitamin C intake either from diet or supplements when they have a cold. Many others take vitamin C supplements routinely to prevent colds. Contrary to this popular practice, however, there is no good evidence that vitamin C prevents a cold. A review of more than fifty years of studies published in 2004 in the Cochrane Database of Systematic Reviews concluded that taking vitamin C routinely does not prevent colds in most people, but it does slightly reduce cold severity and duration. Moreover, taking megadoses (up to 4 grams per day) at the onset of a cold provides no benefits.2
Gout is a disease caused by elevated circulating levels of uric acid and is characterized by recurrent attacks of tender, hot, and painful joints. There is some evidence that a higher intake of vitamin C reduces the risk of gout.
2 Hemilä H, Chalker E.Vitamin C for Preventing and Treating the Common Cold. Cochrane Database of Systematic Reviews. 2013; 4. Accessed June 30, 2019.
Vitamin C Toxicity
High doses of vitamin C have been reported to cause numerous problems, but the only consistently shown side effects are gastrointestinal upset and diarrhea. To prevent these discomforts the I.O.M. has set a U.L. for adults at 2,000 milligrams per day (greater than twenty times the R.D.A.).
At very high doses in combination with iron, vitamin C has sometimes been found to increase oxidative stress, reaffirming that getting your antioxidants from foods is better than getting them from supplements, as that helps regulate your intake levels. There is some evidence that taking vitamin C supplements at high doses increases the likelihood of developing kidney stones, however, this effect is most often observed in people that already have multiple risk factors for kidney stones.
Dietary Reference Intake for Vitamin C
The R.D.A.s and U.L.s for different age groups for vitamin C are listed in Table 10.3.1. They are considered adequate to prevent scurvy. Vitamin C’s effectiveness as a free radical scavenger motivated the Institute of Medicine (I.O.M.) to increase the R.D.A. for smokers by 35 milligrams, as tobacco smoke is an environmental and behavioral contributor to free radicals in the body.
Table 10.3.1: Dietary Reference Intakes for Vitamin C.
| Age Group | R.D.A. Males and Females (Milligrams Per Day) | U.L. |
|---|---|---|
| Infants (0–6 months) | 40* | None |
| Infants (7–12 months) | 50* | None |
| Children (1–3 years) | 15 | 400 |
| Children (4–8 years) | 25 | 650 |
| Children (9–13 years) | 45 | 1200 |
| Adolescents (14–18 years) | 75 (males), 65 (females) | 1800 |
| Adults (> 19 years) | 90 (males), 75 (females) | 2,000 |
Dietary Sources of Vitamin C
Citrus fruits are great sources of vitamin C and so are many vegetables. In fact, British sailors in the past were often referred to as “limeys” as they carried sacks of limes onto ships to prevent scurvy. Vitamin C is not found in significant amounts in animal-based foods. Because vitamin C is water-soluble, it leaches away from foods considerably during cooking, freezing, thawing, and canning. Up to 50 percent of vitamin C can be boiled away. Therefore, to maximize vitamin C intake from foods, you should eat fruits and vegetables raw or lightly steamed. For the vitamin C content of various foods, see Table 10.3.2 .
Table 10.3.2: Vitamin C Content of Various Foods
| Food | Serving | Vitamin C (milligrams) | Percent Daily Value |
|---|---|---|---|
| Orange juice | 6 oz. | 93 | 155 |
| Grapefruit juice | 6 oz. | 70 | 117 |
| Orange | 1 medium | 70 | 117 |
| Strawberries | 1 c. | 85 | 164 |
| Tomato | 1 medium | 17 | 28 |
| Sweet red pepper | ½ c. raw | 95 | 158 |
| Broccoli | ½ c. cooked | 51 | 65 |
| Romaine lettuce | 2 c. | 28 | 47 |
| Cauliflower | 1 c. boiled | 55 | 86 |
| Potato | 1 medium, baked | 17 | 28 |
Thiamin (B1)
Thiamin is especially important in glucose metabolism. It acts as a cofactor for enzymes that break down glucose for energy production (Figure 10.3.4). Thiamin plays a key role in nerve cells as the glucose that is catabolized by thiamin is needed for an energy source. Additionally, thiamin plays a role in the synthesis of neurotransmitters and is therefore required for RNA, DNA, and A.T.P. synthesis.

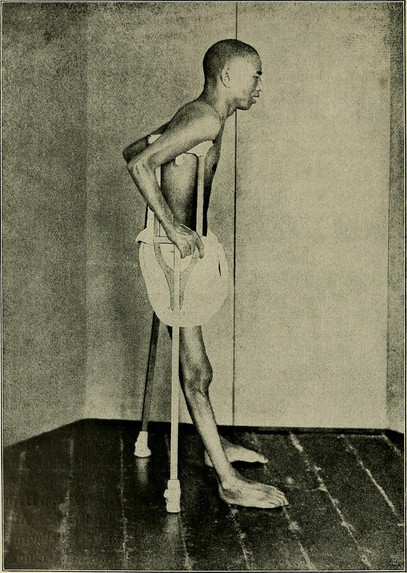
The brain and heart are most affected by a deficiency in thiamin. Thiamin deficiency, also known as beriberi, can cause symptoms of fatigue, confusion, movement impairment, pain in the lower extremities, swelling, and heart failure. It is prevalent in societies whose main dietary staple is white rice. During the processing of white rice, the bran is removed, along with what were called in the early nineteenth century, “accessory factors,” that are vital for metabolism. Dutch physician Dr. Christiaan Eijkman cured chickens of beriberi by feeding them unpolished rice bran in 1897. By 1912, Sir Frederick Gowland Hopkins determined from experiments with animals that the “accessory factors,” eventually renamed vitamins, are needed in the diet to support growth, since animals fed a diet of pure carbohydrates, proteins, fats, and minerals failed to grow.3 Eijkman and Hopkins were awarded the Nobel Prize in Physiology (or Medicine) in 1929 for their discoveries in the emerging science of nutrition.
Another common thiamin deficiency known as Wernicke-Korsakoff syndrome can cause similar symptoms as beriberi such as confusion, loss of coordination, vision changes, hallucinations, and may progress to coma and death. This condition is specific to alcoholics as diets high in alcohol can cause thiamin deficiency. Other individuals at risk include individuals who also consume diets typically low in micronutrients such as those with eating disorders, the elderly and individuals who have gone through gastric bypass surgery.4
3 Frederick Gowland Hopkins and his Accessory Food Factors. Encyclopedia Brittanica Blog. http://www.britannica.com/blogs/2011/06/frederick-gowland-hopkins-accessory-food-factors/.Published June 20, 2011. Accessed June 30, 2019.
4 Fact Sheets for Health Professionals: Thiamin. National Institute of Health, Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/Thiamin-HealthProfessional/. Updated August 22, 2018. Accessed June 30, 2019.
Dietary Reference Intakes of Thiamin
The R.D.A.s and U.L.s for different age groups for thiamin are listed in Table 10.3.3. There is no U.L. for thiamin because there have not been any reports on toxicity when excess amounts are consumed from food or supplements.
Table 10.3.3: Dietary Reference Intakes for Thiamin.
| Age Group | R.D.A. Males and Females (Milligrams Per Day) |
|---|---|
| Infants (0–6 months) | 0.2 * |
| Infants (7–12 months) | 0.3 |
| Children (1–3 years) | 0.5 |
| Children (4–8 years) | 0.6 |
| Children (9–13 years) | 0.9 |
| Adolescents (14–18 years) | 1.2 (males), 1.0 (females) |
| Adults (> 19 years) | 1.2 (males), 1.1 (females) |
Source: Health Professional Fact Sheet: Thiamin. National Institutes of Health, Office of Dietary Supplements. Updated February 11, 2016 . Accessed October 5, 2017.
Dietary Sources of Thiamin
Whole grains, meat, and fish are great sources of thiamin. The United States as well as many other countries fortify their refined bread and cereals. For the thiamin content of various foods, see Table 10.3.4 .
Table 10.3.4: Thiamin Content of Various Foods
| Food | Serving | Thiamin (milligrams) | Percent Daily Value |
|---|---|---|---|
| Breakfast cereals, fortified | 1 serving | 1.5 | 100 |
| White rice, enriched | ½ c. | 1.4 | 73 |
| Porkchop, broiled | 3 oz. | 0.4 | 27 |
| Black beans, boiled | ½ c. | 0.4 | 27 |
| Tuna, cooked | 3 oz. | 0.2 | 13 |
| Brown rice, cooked, not enriched | ½ c. | 0.1 | 7 |
| Whole wheat bread | 1 slice | 0.1 | 7 |
| 2% Milk | 8 oz. | 0.1 | 7 |
| Cheddar cheese | 1 ½ oz | 0 | 0 |
| Apple, sliced | 1 c. | 0 | 0 |
Source: Health Professional Fact Sheet: Thiamin. National Institutes of Health, Office of Dietary. Updated February 11, 2016 . Accessed October 5, 2017.
Riboflavin (B2)
Riboflavin is an essential component of flavoproteins, which are coenzymes involved in many metabolic pathways of carbohydrate, lipid, and protein metabolism. Flavoproteins aid in the transfer of electrons in the electron transport chain. Furthermore, the functions of other B-vitamin coenzymes, such as vitamin B6 and folate, are dependent on the actions of flavoproteins. The “flavin” portion of riboflavin gives a bright yellow color to riboflavin, an attribute that helped lead to its discovery as a vitamin. When riboflavin is taken in excess amounts (supplement form) the excess will be excreted through your kidneys and show up in your urine. Although the color may alarm you, it is harmless. There are no adverse effects of high doses of riboflavin from foods or supplements that have been reported.
Riboflavin deficiency, sometimes referred to as ariboflavinosis, is often accompanied by other dietary deficiencies (most notably protein) and can be common in people that suffer from alcoholism. This deficiency will usually also occur in conjunction with deficiencies of other B vitamins because the majority of B vitamins have similar food sources. Its signs and symptoms include dry, scaly skin, cracking of the lips and at the corners of the mouth, sore throat, itchy eyes, and light sensitivity.
Dietary Reference Intakes of Riboflavin
The R.D.A.s for different age groups for riboflavin are listed in Table 10.3.5. There is no U.L. for riboflavin because no toxicity has been reported when an excess amount has been consumed through foods or supplements.
Table 10.3.5: Dietary Reference Intakes for Riboflavin.
| Age Group | R.D.A. Males and Females (Milligrams Per Day) |
|---|---|
| Infants (0–6 months) | 0.3 * |
| Infants (7–12 months) | 0.4* |
| Children (1–3 years) | 0.5 |
| Children (4–8 years) | 0.6 |
| Children (9–13 years) | 0.9 |
| Adolescents (14–18 years) | 1.3 (males), 1.0 (females) |
| Adults (> 19 years) | 1.3 (males), 1.1 (females) |
Source: Fact Sheet for Health Professionals, Riboflavin. National Institute of Health, Office of Dietary Supplements. Updated February 11, 2016. Accessed October 22, 2017.
Dietary Sources of Riboflavin
Riboflavin can be found in a variety of different foods but it is important to remember that it can be destroyed by sunlight. Milk is one of the best sources of riboflavin in the diet and was once delivered and packaged in glass bottles. This packaging has changed to cloudy plastic containers or cardboard to help block the light from destroying the riboflavin in milk. For the riboflavin content of various foods (Table 10.3.6 ).
Table 10.3.6: Riboflavin Content of Various Foods
| Food | Serving | Riboflavin (milligrams) | Percent Daily Value |
|---|---|---|---|
| Beef liver | 3 oz. | 2.9 | 171 |
| Breakfast cereals, fortified | 1 serving | 1.7 | 100 |
| Instant oats, fortified | 1 c. | 1.1 | 65 |
| Plain yogurt, fat free | 1 c. | 0.6 | 35 |
| 2% milk | 8 oz. | 0.5 | 29 |
| Beef, tenderloin steak | 3 oz. | 0.4 | 24 |
| Portabella mushrooms, sliced | ½ c. | 0.3 | 18 |
| Almonds, dry roasted | 1 oz. | 0.3 | 18 |
| Egg, scrambled | 1 large | 0.2 | 12 |
| Quinoa | 1 c. | 0.2 | 12 |
| Salmon, canned | 3 oz. | 0.2 | 12 |
| Spinach, raw | 1 c. | 0.1 | 6 |
| Brown rice | ½ c. | 0 | 0 |
Source: Fact Sheet for Health Professionals, Riboflavin. National Institute of Health, Office of Dietary Supplements. Updated February 11, 2016. Accessed October 22, 2017.
Niacin (B3)
Niacin is a component of the coenzymes N.A.D.H. and N.A.D.P.H., which are involved in the catabolism and/or anabolism of carbohydrates, lipids, and proteins. N.A.D.H. is the predominant electron carrier and transfers electrons to the electron-transport chain to make A.T.P.. N.A.D.P.H. is also required for the anabolic pathways of fatty-acid and cholesterol synthesis. In contrast to other vitamins, niacin can be synthesized by humans from the amino acid tryptophan in a process requiring enzymes dependent on riboflavin, vitamin B6, and iron. Niacin is made from tryptophan only after tryptophan has met all of its other needs in the body. The contribution of tryptophan-derived niacin to niacin needs in the body varies widely and a few scientific studies have demonstrated that diets high in tryptophan have very little effect on niacin deficiency. Niacin deficiency is commonly known as pellagra and the symptoms include fatigue, decreased appetite, and indigestion. These symptoms are then commonly followed by the four D’s: diarrhea, dermatitis, dementia, and sometimes death.

Dietary Reference Intakes of Niacin
The R.D.A.s and U.L.s for different age groups for Niacin are listed in Table 10.3.7 . Because Niacin needs can be met from tryptophan, The R.D.A. is expressed in niacin equivalents (N.E.s). The conversions of N.E., Niacin, and tryptophan are: 1 mg N.E.= 60 milligram tryptophan= 1 mg niacin
Table 10.3.7: Dietary Reference Intakes for Niacin.
| Age Group | R.D.A. Males and Females (Milligrams Per Day) | U.L. |
|---|---|---|
| Infants (0–6 months) | 2* | Not possible to establish |
| Infants (7–12 months) | 4* | Not possible to establish |
| Children (1–3 years) | 6 | 10 |
| Children (4–8 years) | 8 | 15 |
| Children (9–13 years) | 12 | 20 |
| Adolescents (14–18 years) | 16 (males), 14 (females) | 30 |
| Adults (> 19 years) | 16 (males), 14 (females) | 35 |
Micronutrient Information Center: Niacin. Oregon State University, Linus Pauling Institute. Updated in July 2013. Accessed October 22, 2017.
Dietary Sources of Niacin
Niacin can be found in a variety of different foods such as yeast, meat, poultry, red fish, and cereal. In plants, especially mature grains, niacin can be bound to sugar molecules which can significantly decrease the niacin bioavailability. For the niacin content of various foods, see Table 10.3.8.
Table 10.3.8: Niacin Content of Various Foods
| Food | Serving | Niacin (milligrams) | Percent Daily Value |
|---|---|---|---|
| Chicken | 3 oz. | 7.3 | 36.5 |
| Tuna | 3 oz. | 8.6 | 43 |
| Turkey | 3 oz. | 10.0 | 50 |
| Salmon | 3 oz. | 8.5 | 42.5 |
| Beef (90% lean) | 3 oz. | 4.4 | 22 |
| Cereal (unfortified) | 1 c. | 5 | 25 |
| Cereal (fortified) | 1 c. | 20 | 100 |
| Peanuts | 1 oz. | 3.8 | 19 |
| Whole wheat bread | 1 slice | 1.3 | 6.5 |
| Coffee | 8 oz. | 0.5 | 2.5 |
Source: Micronutrient Information Center: Niacin. Oregon State University, Linus Pauling Institute. Updated in July 2013. Accessed October 22, 2017.
Pantothenic Acid (B5)
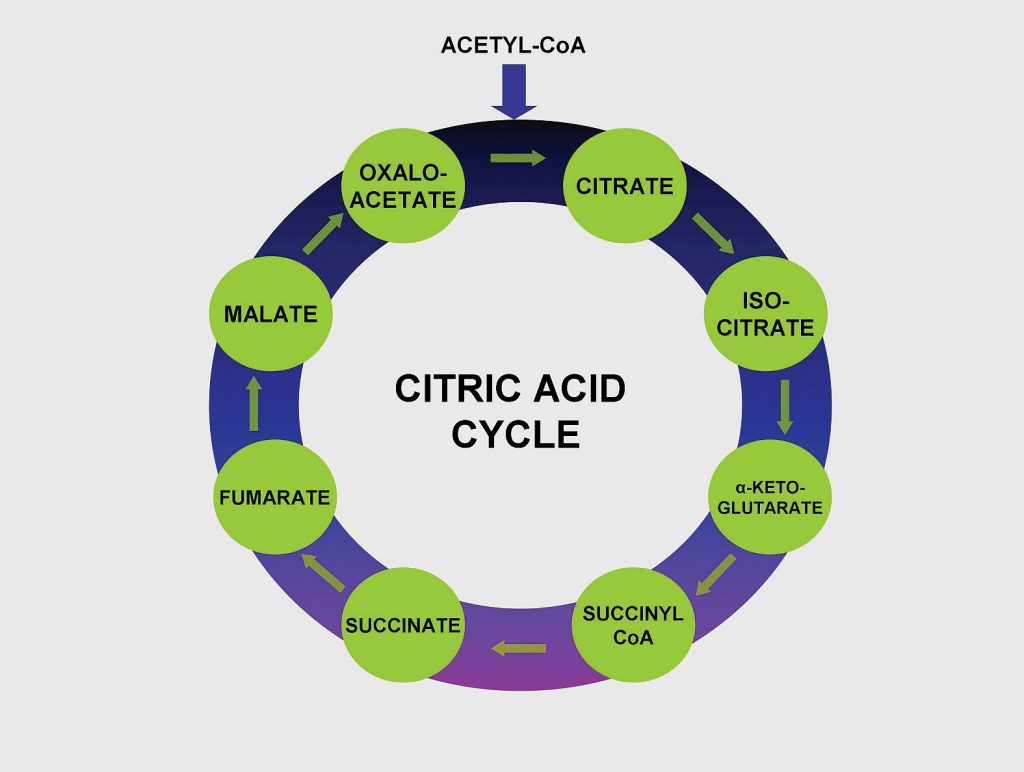
Pantothenic acid forms coenzyme A, which is the main carrier of carbon molecules in a cell. Acetyl-CoA is the carbon carrier of glucose, fatty acids, and amino acids into the citric acid cycle (Figure 10.3.8). Coenzyme A is also involved in the synthesis of lipids, cholesterol, and acetylcholine (a neurotransmitter). A Pantothenic Acid deficiency is exceptionally rare. Signs and symptoms include fatigue, irritability, numbness, muscle pain, and cramps. You may have seen pantothenic acid on many ingredients lists for skin and hair care products; however there is no good scientific evidence that pantothenic acid improves human skin or hair.
Dietary Reference Intake for Pantothenic Acid
Because there is little information on the requirements for pantothenic acids, the Food and Nutrition Board (F.N.B.) has developed Adequate Intakes (A.I.) based on the observed dietary intakes in healthy population groups. The A.I. for different age groups for pantothenic acid is listed in Table 10.3.9.
Table 10.3.9: Dietary Reference Intakes for Pantothenic Acid.
| Age Group | A.I. Males and Females (Milligrams Per Day) |
|---|---|
| Infants (0–6 months) | 1.7 |
| Infants (7–12 months) | 1.8 |
| Children (1–3 years) | 2 |
| Children (4–8 years) | 3 |
| Children (9–13 years) | 4 |
| Adolescents (14–18 years) | 5 |
| Adults (> 19 years) | 5 |
Source: Micronutrient Information Center: Pantothenic Acid. Oregon State University, Linus Pauling Institute. Updated in July 2013. Accessed October 22, 2017.
Dietary Sources of Pantothenic Acid
Pantothenic Acid is widely distributed in all types of food, which is why a deficiency in this nutrient is rare. Pantothenic Acid gets its name from the Greek word “pantothen” which means “from everywhere”. For the pantothenic acid content of various foods, see Table 10.3.10 .
Table 10.3.10: Pantothenic Acid Content of Various Foods
| Food | Serving | Pantothenic Acid (milligrams) | Percent Daily Value |
|---|---|---|---|
| Sunflower seeds | 1 oz. | 2 | 20 |
| Fish, trout | 3 oz. | 1.9 | 19 |
| Yogurt, plain nonfat | 8 oz. | 1.6 | 16 |
| Lobster | 3 oz. | 1.4 | 14 |
| Avocado | ½ fruit | 1 | 10 |
| Sweet potato | 1 medium | 1 | 10 |
| Milk | 8 fl oz. | 0.87 | 8.7 |
| Egg | 1 large | 0.7 | 7 |
| Orange | 1 whole | 0.3 | 3 |
| Whole wheat bread | 1 slice | 0.21 | 2.1 |
Source: Micronutrient Information Center: Pantothenic Acid. Oregon State University, Linus Pauling Institute. Updated in July 2013. Accessed October 22, 2017.
Biotin
Biotin is required as a coenzyme in the citric acid cycle and in lipid metabolism. It is also required as an enzyme in the synthesis of glucose and some nonessential amino acids. A specific enzyme, biotinidase, is required to release biotin from protein so that it can be absorbed in the gut. There is some bacterial synthesis of biotin that occurs in the colon; however this is not a significant source of biotin. Biotin deficiency is rare, but can be caused by eating large amounts of raw egg whites over an extended period of time. This is because a protein in egg whites tightly binds to biotin making it unavailable for absorption. A rare genetic disease-causing malfunction of the biotinidase enzyme also results in biotin deficiency. Symptoms of biotin deficiency are similar to those of other B vitamins, but may also include hair loss when severe.
Dietary Reference Intakes of Biotin
Because there is little information on the requirements for biotin, the F.N.B. has developed Adequate Intakes (A.I.) based on the observed dietary intakes in healthy population groups. The A.I. for different age groups for biotin is listed in Table 10.3.11.
Table 10.3.11: Dietary Reference Intakes for Biotin.
| Age Group | A.I. Males and Females (Micrograms Per Day) |
|---|---|
| Infants (0–6 months) | 5 |
| Infants (7–12 months) | 6 |
| Children (1–3 years) | 8 |
| Children (4–8 years) | 12 |
| Children (9–13 years) | 20 |
| Adolescents (14–18 years) | 25 |
| Adults (> 19 years) | 30 |
Source: Fact Sheet for Health Professionals: Biotin. National Institute of Health, Office of Dietary Supplements. Updated October 3, 2017. Accessed November 10, 2017.
Dietary Sources of Biotin
Biotin can be found in foods such as eggs, fish, meat, seeds, nuts, and certain vegetables. For the pantothenic acid content of various foods, see Table 10.3.12.
Table 10.3.12: Biotin Content of Various Foods
| Food | Serving | Biotin (micrograms) | Percent Daily Value |
|---|---|---|---|
| Eggs | 1 large | 10 | 33.3 |
| Salmon, canned | 3 oz. | 5 | 16.6 |
| Pork chop | 3 oz. | 3.8 | 12.6 |
| Sunflower seeds | ¼ c. | 2.6 | 8.6 |
| Sweet potato | ½ c. | 2.4 | 8 |
| Almonds | ¼ c. | 1.5 | 5 |
| Tuna, canned | 3 oz. | 0.6 | 2 |
| Broccoli | ½ c. | 0.4 | 1.3 |
| Banana | ½ c. | 0.2 | 0.6 |
Source: Fact Sheet for Health Professionals: Biotin. National Institute of Health, Office of Dietary Supplements. Updated October 3, 2017. Accessed November 10, 2017.
Vitamin B6 (Pyridoxine)
Vitamin B6 is the coenzyme involved in a wide variety of functions in the body. One major function is the nitrogen transfer between amino acids which plays a role in amino-acid synthesis and catabolism. Also, it functions to release glucose from glycogen in the catabolic pathway of glycogenolysis and is required by enzymes for the synthesis of multiple neurotransmitters and hemoglobin (Figure 10.3.9).
Vitamin B6 is also a required coenzyme for the synthesis of hemoglobin. A deficiency in vitamin B6 can cause anemia, but it is of a different type than that caused by insufficient folate, cobalamin, or iron; although the symptoms are similar. The size of red blood cells is normal or somewhat smaller but the hemoglobin content is lower. This means each red blood cell has less capacity for carrying oxygen, resulting in muscle weakness, fatigue, and shortness of breath. Other deficiency symptoms of vitamin B6 can cause dermatitis, mouth sores, and confusion.

The vitamin B6 coenzyme is needed for a number of different reactions that are essential for amino acid synthesis, catabolism for energy, and the synthesis of glucose and neurotransmitters.
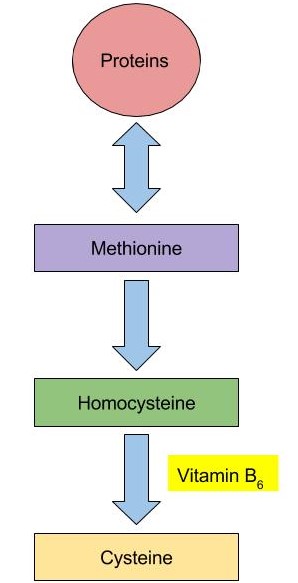
Vitamin B6 coenzyme is essential for the conversion of amino acid methionine into cysteine. With low levels of Vitamin B6, homocysteine will build up in the blood. High levels of homocysteine increase the risk of heart disease.
Vitamin B6 Toxicity
Currently, there are no adverse effects that have been associated with a high dietary intake of vitamin B6, but large supplemental doses can cause severe nerve impairment. To prevent this from occurring, the U.L. for adults is set at 100 mg/day.
Dietary Reference Intakes of Vitamin B 6
The R.D.A.s and U.L.s for different age groups for vitamin B6 are listed in Table 10.3.13.
Table 10.3.13: Dietary Reference Intakes for vitamin B6.
| Age Group | R.D.A. Males and Females (Milligrams Per Day) | U.L. |
|---|---|---|
| Infants (0–6 months) | 0.1* | Not possible to determine |
| Infants (7–12 months) | 0.3* | Not possible to determine |
| Children (1–3 years) | 0.5 | 30 |
| Children (4–8 years) | 0.6 | 40 |
| Children (9–13 years) | 1 | 60 |
| Adolescents (14–18 years) | 1.3 (males), 1.2 (females) | 80 |
| Adults ( > 19 years) | 1.3 | 100 |
Source: Dietary Supplement Fact Sheet: Vitamin B6. National Institute of Health, Office of Dietary Supplements. Updates February 11, 2016. Accessed October 22, 2017.
Dietary Sources of Vitamin B6
Vitamin B6 can be found in a variety of foods. The richest sources include fish, beef liver and other organ meats, potatoes, and other starchy vegetables and fruits. For the Vitamin B6 content of various foods, see Table 10.3.14.
Table 10.3.13: B6 Content of Various Foods
| Food | Serving | Vitamin B6 (milligrams) | Percent Daily Value |
|---|---|---|---|
| Chickpeas | 1 c. | 1.1 | 55 |
| Tuna, fresh | 3 oz. | 0.9 | 45 |
| Salmon | 3 oz. | 0.6 | 30 |
| Potatoes | 1 c. | 0.4 | 20 |
| Banana | 1 medium | 0.4 | 20 |
| Ground beef patty | 3 oz. | 0.3 | 10 |
| White rice, enriched | 1 c. | 0.1 | 5 |
| Spinach | ½ c | 0.1 | 5 |
Dietary Supplement Fact Sheet: Vitamin B6. National Institute of Health, Office of Dietary Supplements. Updates February 11, 2016. Accessed October 22, 2017.
Folate
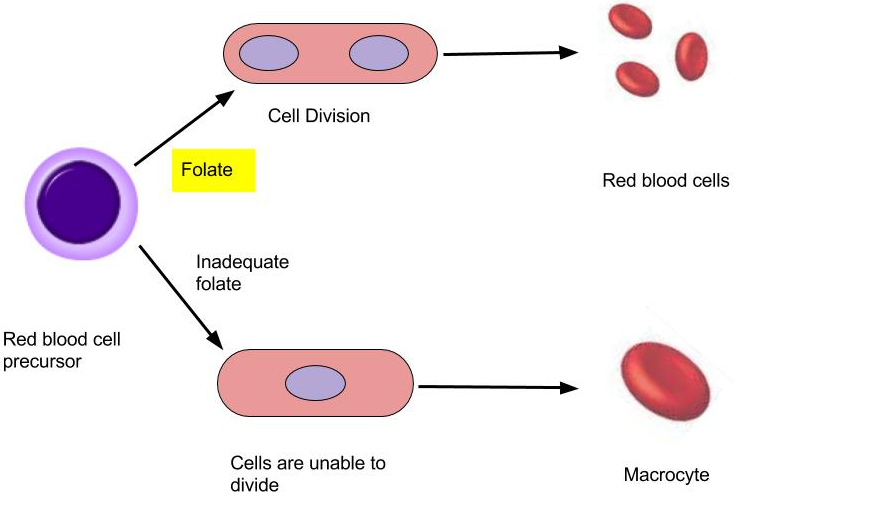
Folate is a required coenzyme for the synthesis of the amino acid methionine, and for making RNA and DNA. Therefore, rapidly dividing cells are most affected by folate deficiency. Red blood cells, white blood cells, and platelets are continuously being synthesized in the bone marrow from dividing stem cells. When folate is deficient, cells cannot divide normally A consequence of folate deficiency is macrocytic or megaloblastic anemia. Macrocytic and megaloblastic mean “big cell,” and anemia refers to fewer red blood cells or red blood cells containing less hemoglobin. Macrocytic anemia is characterized by larger and fewer red blood cells. It is caused by red blood cells being unable to produce DNA and RNA fast enough—cells grow but do not divide, making them large in size. (Figure 10.3.11).
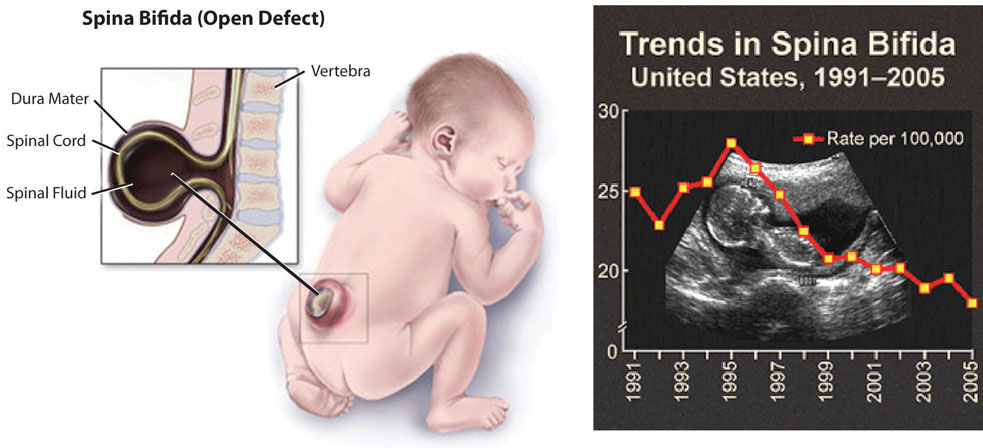
Folate is especially essential for the growth and specialization of cells of the central nervous system. Children whose mothers were folate-deficient during pregnancy have a higher risk of neural-tube birth defects. Folate deficiency is causally linked to the development of spina bifida, a neural-tube defect that occurs when the spine does not completely enclose the spinal cord. Spina bifida can lead to many physical and mental disabilities (Figure 10.3.12 ). Observational studies show that the prevalence of neural-tube defects was decreased after the fortification of enriched cereal grain products with folate in 1996 in the United States (and 1998 in Canada) compared to before grain products were fortified with folate.
Additionally, results of clinical trials have demonstrated that neural-tube defects are significantly decreased in the offspring of mothers who began taking folate supplements one month prior to becoming pregnant and throughout the pregnancy. In response to the scientific evidence, the Food and Nutrition Board of the Institute of Medicine (I.O.M.) raised the R.D.A. for folate to 600 micrograms per day for pregnant women. Some were concerned that higher folate intakes may cause colon cancer, however scientific studies refute this hypothesis.
Dietary Reference Intakes of Folate
The R.D.A.s and U.L.s for different age groups for folate are listed in Table 10.3.15 . Folate is a compound that is found naturally in foods. Folic acid however is the chemical structure form that is used in dietary supplements as well as enriched foods such as grains. The F.N.B. has developed dietary folate equivalents (D.F.E.) to reflect the fact that folic acid is more bioavailable and easily absorbed than folate found in food. The conversions for the different forms are listed below.
- 1 mcg D.F.E. = 1 mcg food folate
- 1mcg D.F.E. = 0.6 mcg folic acid from fortified foods or dietary supplements consumed with foods
- 1 mcg D.F.E. = 0.5 mcg folic acid from dietary supplements taken on an empty stomach
Table 10.3.15: Dietary Reference Intakes for Folate.
| Age Group | R.D.A. Males and Females (micrograms D.F.E. Per Day) | U.L. |
|---|---|---|
| Infants (0–6 months) | 65* | Not possible to determine |
| Infants (7–12 months) | 80* | Not possible to determine |
| Children (1–3 years) | 150 | 300 |
| Children (4–8 years) | 200 | 400 |
| Children (9–13 years) | 300 | 600 |
| Adolescents (14–18 years) | 400 | 800 |
| Adults (> 19 years) | 400 | 1000 |
Source: Dietary Supplement Fact Sheet: Folate. National Institute of Health, Office of Dietary Supplements. Updated April 20, 2016. Accessed October 22, 2017.
Dietary Sources of Folate
Folate is found naturally in a wide variety of food especially in dark leafy vegetables (foliage), fruits, and animal products. The U.S. Food and Drug Administration (FDA) began requiring manufacturers to fortify enriched bread, cereals, flours, and cornmeal to increase the consumption of folate in the American diet. For the folate content of various foods, see Table 10.3.16.
Table 10.3.16: Folate Content of Various Foods
| Food | Serving | Folate (micrograms D.F.E.) | Percent Daily Value |
|---|---|---|---|
| Beef Liver | 3 oz. | 215 | 54 |
| Fortified breakfast cereals | ¾ c. | 400 | 100 |
| Spinach | ½ c. | 131 | 33 |
| White rice, enriched | ½ c. | 90 | 23 |
| Asparagus | 4 spears | 85 | 20 |
| White bread, enriched | 1 slice | 43 | 11 |
| Broccoli | 2 spears | 45 | 10 |
| Avocado | ½ c. | 59 | 15 |
| Orange juice | 6 oz. | 35 | 9 |
| Egg | 1 large | 22 | 6 |
Dietary Supplement Fact Sheet: Folate. National Institute of Health, Office of Dietary Supplements. Updated April 20, 2016. Accessed October 22, 2017.
Vitamin B12 (Cobalamin)
Vitamin B12 contains cobalt, making it the only vitamin that contains a metal ion. Vitamin B12 is an essential part of coenzymes. It is necessary for fat and protein catabolism, for folate coenzyme function, and for hemoglobin synthesis. An enzyme requiring vitamin B12 is needed by a folate-dependent enzyme to synthesize DNA. Thus, a deficiency in vitamin B12 has similar consequences to health as folate deficiency. In children and adults, vitamin B12 deficiency causes macrocytic anemia, and in babies born to cobalamin-deficient mothers there is an increased risk for neural-tube defects. In order for the human body to absorb vitamin B12, the stomach, pancreas, and small intestine must be functioning properly. Cells in the stomach secrete a protein called intrinsic factor that is necessary for vitamin B12 absorption, which occurs in the small intestine. Impairment of secretion of this protein either caused by an autoimmune disease or by chronic inflammation of the stomach (such as that occurring in some people with H.pylori infection), can lead to the disease pernicious anemia, a type of macrocytic anemia. Vitamin B12 malabsorption is most common in the elderly, who may have impaired functioning of digestive organs, a normal consequence of aging. Pernicious anemia is treated by large oral doses of vitamin B12 or by putting the vitamin under the tongue, where it is absorbed into the bloodstream without passing through the intestine. In patients that do not respond to oral or sublingual treatment, vitamin B12 is given by injection.
Vitamin B12 Relationship with Folate and Vitamin B6
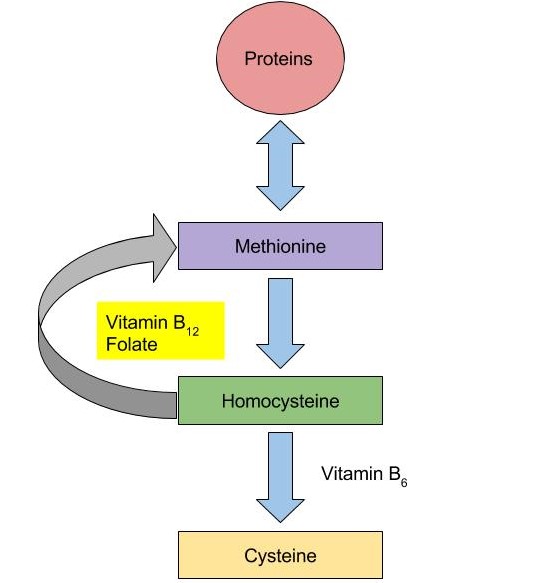
Vitamin B12 and folate play key roles in converting homocysteine to amino acid methionine. As mentioned in Figure 10.3.13, high levels of homocysteine in the blood increases the risk of heart disease. Low levels of vitamin B12, folate or vitamin B6 will increase homocysteine levels, therefore, increasing the risk of heart disease.
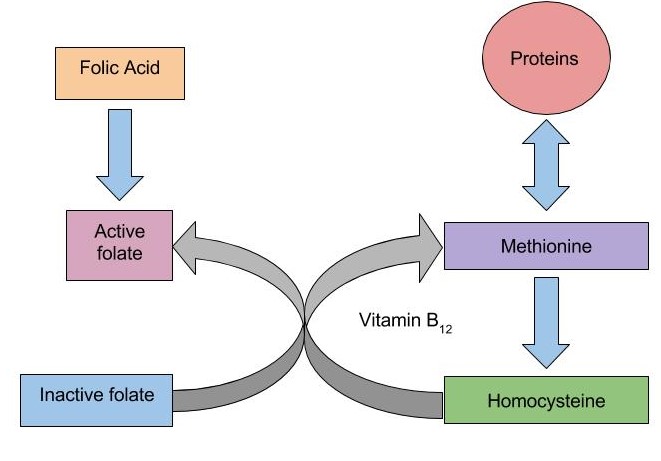
When there is a deficiency in vitamin B12, inactive folate (from food) is unable to be converted to active folate and used in the body for the synthesis of DNA. Folic Acid, however (that comes from supplements or fortified foods) is available to be used as active folate in the body without vitamin B12. Therefore, if there is a deficiency in vitamin B12, macrocytic anemia may occur. With the fortification of foods incorporated into people’s diets, the risk of an individual developing macrocytic anemia is decreased.
Dietary Reference Intakes of Vitamin B 12
The R.D.A.s and U.L.s for different age groups for Vitamin B12 are listed in Table 10.3.17.
Table 10.3.17: Dietary Reference Intakes for Vitamin B 12.
| Age Group | R.D.A. Males and Females (micrograms Per Day) |
|---|---|
| Infants (0–6 months) | 0.4* |
| Infants (7–12 months) | 0.5* |
| Children (1–3 years) | 0.9 |
| Children (4–8 years) | 1.2 |
| Children (9–13 years) | 1.8 |
| Adolescents (14–18 years) | 2.4 |
| Adults (> 19 years) | 2.4 |
Source: Dietary Fact Sheet: Vitamin B12. National Institute of Health, Office of Dietary Supplements. Updated February 11, 2016. Accessed October 28, 2017.
Dietary Sources of B12
Vitamin B12 is found naturally in animal products such as fish, meat, poultry, eggs, and milk products. Although vitamin B12 is not generally present in plant foods, fortified breakfast cereals are also a good source of vitamin B12. For the vitamin B12 content of various foods, see Table 10.3.18.
Table 10.3.18: B12 Content of Various Foods
| Food | Serving | B12 (micrograms) | Percent Daily Value |
|---|---|---|---|
| Clams | 3 oz. | 84.1 | 1,402 |
| Salmon | 3 oz. | 4.8 | 80 |
| Tuna, canned | 3 oz. | 2.5 | 42 |
| Breakfast cereals, fortified | 1 serving | 1.5 | 25 |
| Beef, top sirloin | 3 oz. | 1.4 | 23 |
| Milk, low-fat | 8 fl oz. | 1.2 | 18 |
| Yogurt, low-fat | 8 oz. | 1.1 | 18 |
| Cheese, swiss | 1 oz. | 0.9 | 15 |
| Egg | 1 large | 0.6 | 10 |
Source: Dietary Fact Sheet: Vitamin B12. National Institute of Health, Office of Dietary Supplements. Updated February 11, 2016. Accessed October 28, 2017.
Choline
Choline is a water-soluble substance that is not classified as a vitamin because it can be synthesized by the body. However, the synthesis of choline is limited and therefore it is recognized as an essential nutrient. Choline is needed to perform functions such as the synthesis of the neurotransmitter acetylcholine, the synthesis of phospholipids used to make cell membranes, lipid transport, and also homocysteine metabolism. A deficiency in choline may lead to impaired brain development in the fetus during pregnancy, and in adults cause fatty liver and muscle damage.
Dietary Reference Intakes of Choline
There is insufficient data on choline so the F.N.B. has developed A.I.s for all ages in order to prevent fatty liver disease. The A.I. and U.L. for different age groups for choline are listed in Table 10.3.19.
Table 10.3.19: Dietary Reference Intakes for Choline.
| Age Group | A.I. Males and Females (Milligrams Per Day) | U.L. |
|---|---|---|
| Infants (0–6 months) | 125 | None |
| Infants (7–12 months) | 150 | None |
| Children (1–3 years) | 200 | 1000 |
| Children (4–8 years) | 250 | 1000 |
| Children (9–13 years) | 375 | 2000 |
| Adolescents (14–18 years) | 550 (males), 400 (females) | 3000 |
| Adults (> 19 years) | 550 (males), 425 (females) | 3500 |
Source: Fact Sheet for Health Professionals: Choline. National Institute of Health, Office of Dietary Supplements. Updated January 25, 2017. Accessed October 28, 2017.
Dietary Sources of Choline
Choline can be found in a variety of different foods. The main dietary sources of choline in the United States consist of primarily animal-based products. For the Choline content of various foods, see Table 10.3.20.
Table 10.3.20: Choline Content of Various Foods
| Food | Serving | Choline (milligrams) | Percent Daily Value |
|---|---|---|---|
| Egg | 1 large | 147 | 27 |
| Soybeans | ½ cup | 107 | 19 |
| Chicken breast | 3 oz. | 72 | 13 |
| Mushrooms, shiitake | ½ c. | 58 | 11 |
| Potatoes | 1 large | 57 | 10 |
| Kidney beans | ½ c. | 45 | 8 |
| Peanuts | ¼ c. | 24 | 4 |
| Brown rice | 1 c. | 19 | 3 |
Source: Fact Sheet for Health Professionals: Choline. National Institute of Health, Office of Dietary Supplements. Updated January 25, 2017. Accessed October 28, 2017.
Summary of Water-Soluble Vitamins
| Vitamin | Sources | Recommended Intake for Adults | Functions | Deficiency Diseases and Symptoms | Groups at Risk of Deficiency | Toxicity | U.L. |
|---|---|---|---|---|---|---|---|
| Vitamin C (ascorbic acid) | Orange juice, grapefruit juice, strawberries, tomato, sweet red pepper | 75-90 mg/day | Antioxidant, collagen synthesis, hormone and neurotransmitter synthesis | Scurvy, bleeding gums, joint pain, poor wound healing, | Smokers, alcoholics, elderly | Kidney stones, GI distress, diarrhea | 2000 mg/day |
| Thiamin (B1) | Pork, enriched and whole grains, fish, legumes | 1.1-1.2 mg/day | Coenzyme: assists in glucose metabolism, RNA, DNA, and A.T.P. synthesis | Beriberi: fatigue, confusion, movement impairment, swelling, heart failure | Alcoholics, older adults, eating disorders | None reported | N D |
| Riboflavin (B2) | Beef liver, enriched breakfast cereals, yogurt, steak, mushrooms, almonds, eggs | 1.1-1.3 mg/day | Coenzyme: assists in glucose, fat and carbohydrate metabolism, electron carrier, other B vitamins are dependent on | Ariboflavinosis: dry scaly skin, mouth inflammation and sores, sore throat, itchy eyes, light sensitivity | None | None reported | N D |
| Niacin (B3) | Meat, poultry, fish, peanuts, enriched grains | 14-16 NE/day | Coenzyme: assists in glucose, fat, and protein metabolism, electron carrier | Pellagra: diarrhea, dermatitis, dementia, death | Alcoholics | Nausea, rash, tingling extremities | 35 mg/day from fortified foods and supplements |
| Pantothenic Acid (B5) | Sunflower seeds, fish, dairy products, widespread in foods | 5 mg/day | Coenzyme: assists in glucose, fat, and protein metabolism, cholesterol and neurotransmitter synthesis | Muscle numbness and pain, fatigue, irritability | Alcoholics | Fatigue, rash | N D |
| B6 (Pyridoxine) | Meat, poultry, fish, legumes, nuts | 1.3-1.7 mg/day | Coenzyme; assists in amino-acid synthesis, glycogneolysis, neurotransmitter and hemoglobin synthesis | Muscle weakness, dermatitis, mouth sores, fatigue, confusion | Alcoholics | Nerve damage | 100 mg/day |
| Biotin | Egg yolks, fish, pork, nuts and seeds | 30 mcg/day | Coenzyme; assists in glucose, fat, and protein metabolism, amino-acid synthesis | Muscle weakness, dermatitis, fatigue, hair loss | Those consuming raw egg whites | None reported | N D |
| Folate | Leafy green vegetables, enriched grains, orange juice | 400 mcg/day | Coenzyme; amino acid synthesis, RNA, DNA, and red blood cell synthesis | Diarrhea, mouth sores, confusion, anemia, neural-tube defects | Pregnant women, alcoholics | Masks B12 deficiency | 1000 mcg/day from fortified foods and supplements |
| B12 (cobalamin) | Meats, poultry, fish | 2.4 mcg/day | Coenzyme; fat and protein catabolism, folate function, red-blood-cell synthesis | Muscle weakness, sore tongue, anemia, nerve damage, neural-tube defects | Vegans, elderly | None reported | N D |
| Choline | Egg yolk, wheat, meat, fish, synthesis in the body | 425-550 mg/day | Synthesis of neurotransmitters and cell membranes, lipid transport | Non-alcoholic fatty liver disease, muscle damage, interfered brain development in fetus | None | Liver damage, excessive sweating, hypotension | 3500 mg/day |
Do B-Vitamin Supplements Provide an Energy Boost?
Although some marketers claim taking a vitamin that contains one-thousand times the daily value of certain B vitamins boosts energy and performance, this is a myth that is not backed by science. The “feeling” of more energy from energy-boosting supplements stems from the high amount of added sugars, caffeine, and other herbal stimulants that accompany the high doses of B vitamins. As discussed, B vitamins are needed to support energy metabolism and growth, but taking in more than required does not supply you with more energy. A great analogy of this phenomenon is the gas in your car. Does it drive faster with a half-tank of gas or a full one? It does not matter; the car drives just as fast as long as it has gas. Similarly, depletion of B vitamins will cause problems in energy metabolism, but having more than is required to run metabolism does not speed it up. Buyers of B-vitamin supplements beware; B vitamins are not stored in the body and all excess will be flushed down the toilet along with the extra money spent.
B vitamins are naturally present in numerous foods, and many other foods are enriched with them. In the United States, B-vitamin deficiencies are rare; however, in the nineteenth century, some vitamin-B deficiencies plagued many people in North America. Niacin deficiency, also known as pellagra, was prominent in poorer Americans whose main dietary staple was refined cornmeal. Its symptoms were severe and included diarrhea, dermatitis, dementia, and even death. Some of the health consequences of pellagra are the result of niacin being in insufficient supply to support the body’s metabolic functions.
Key Takeaways
- See the Table above for a summary of the water-soluble vitamins.
Contributors
University of Hawai’i at Mānoa Food Science and Human Nutrition Program: Allison Calabrese, Cheryl Gibby, Billy Meinke, Marie Kainoa Fialkowski Revilla, and Alan Titchenal

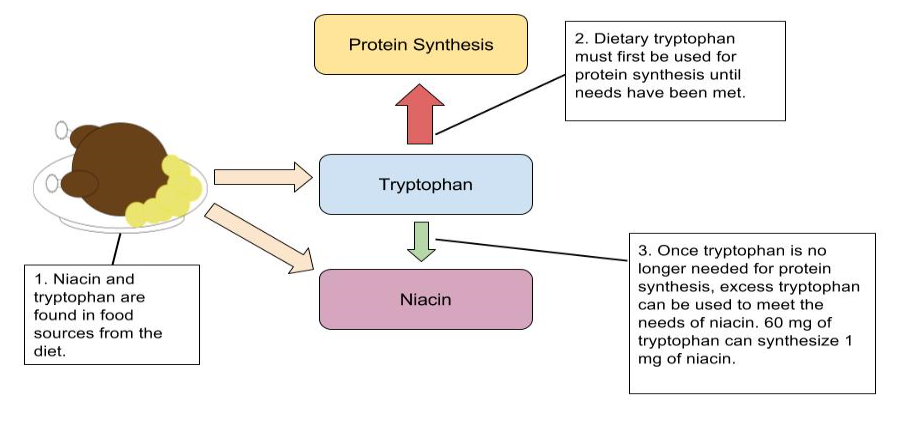 an illustration depicting the conversion of tryptophan to niacin in 3 steps. 1. Niacin and tryptophan are found in food sources from the diet. 2. Dietary tryptophan must first be used for protein synthesis until needs have been met. 3. Once tryptophan is no longer needed for protein synthesis, excess tryptophan can be used to meet the needs of niacin. 60 milligrams of tryptophan can synthesize 1 milligram of niacin
an illustration depicting the conversion of tryptophan to niacin in 3 steps. 1. Niacin and tryptophan are found in food sources from the diet. 2. Dietary tryptophan must first be used for protein synthesis until needs have been met. 3. Once tryptophan is no longer needed for protein synthesis, excess tryptophan can be used to meet the needs of niacin. 60 milligrams of tryptophan can synthesize 1 milligram of niacin