5.5 – Looking Closely at Diabetes
Learning Objective
- Summarize the long-term health implications and the dietary approaches to living with type 1 and type 2 diabetes.
Diabetes is one of the top three diseases in the United States. The International Diabetes Atlas 9th edition estimates that, globally, 463 million adults (9.3% of the world adult population) aged over 20 years were living with diabetes in 2019.1 Diabetes caused 1.5 million deaths in 2012. Higher-than-optimal blood glucose caused an additional 2.2 million deaths, by increasing the risks of cardiovascular and other diseases. Forty-three percent of these 3.7 million deaths occur before the age of 70 years. The percentage of deaths attributable to high blood glucose or diabetes that occurs prior to age 70 is higher in low- and middle-income countries than in high-income countries.2
Diabetes is a metabolic disease of insulin deficiency and glucose over-sufficiency. Like other diseases, genetics, nutrition, environment, and lifestyle are all involved in determining a person’s risk of developing diabetes. One sure way to decrease your chances of getting diabetes is to maintain optimal body weight by adhering to a diet that is balanced in carbohydrate, fat, and protein intake and getting the recommended amount of activity each day. There are three different types of diabetes: type 1 diabetes, type 2 diabetes, and gestational diabetes.
1 Saeedi, P. et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Research and Clinical Practice. 2019; 157 Accessed June 11, 2021.
2Global Report on Diabetes. World Health Organization. 2016. Accessed Feb 20, 2020
Type 1 Diabetes
Type 1 diabetes is a metabolic disease in which insulin-secreting cells in the pancreas are killed by an abnormal response of the immune system, causing a lack of insulin in the body. Its onset typically occurs before the age of thirty but can happen at any age. The only way to prevent the deadly symptoms of this disease is to inject insulin under the skin. Before this treatment was discovered, people with type 1 diabetes died rapidly after disease onset. Death was the result of extremely high blood-glucose levels affecting brain function and leading to coma and death. Up until 1921, patients with type 1 diabetes, the majority of them children, spent their last days in a ward where they lapsed into a coma awaiting death. One of the most inspiring acts in medical history is that of the scientists who discovered, isolated, and purified insulin and then went on to find out that it relieved the symptoms of type 1 diabetes, first in dogs and then in humans. Frederick Banting, Charles Best, and James Collip went into a hospital ward in Toronto, Canada, and injected comatose children with insulin. Before they completed their rounds children were already awakening to the cheers of their families.
A person with type 1 diabetes usually has a rapid onset of symptoms that include hunger, excessive thirst and urination, and rapid weight loss. Because the main function of glucose is to provide energy for the body when insulin is no longer present there is no message sent to cells to take up glucose from the blood. Instead, cells use fat and proteins to make energy, resulting in weight loss. If type 1 diabetes goes untreated, individuals with the disease will develop a life-threatening condition called ketoacidosis. This condition occurs when the body uses fats and not glucose to make energy, resulting in a build-up of ketone bodies in the blood. Ketoacidosis includes the symptoms of vomiting, dehydration, rapid breathing, and confusion, and eventually coma and death. Upon insulin injection, these severe symptoms are treated and death is avoided. Unfortunately, while insulin injection prevents death, it is not considered a cure. People who have this disease must learn to match insulin quantities to the amount of carbohydrate and activity they are getting each day to prevent the development of serious complications. People with type 1 diabetes are advised to count the carbohydrates they eat, to consume healthy-carbohydrate foods, and to check their blood glucose levels multiple times per day. These guidelines are aimed at preventing large fluctuations in blood glucose. Frequent exercise also helps manage blood-glucose levels. Type 1 diabetes accounts for between 5 and 10 percent of diabetes cases.
Research continues to focus on a cure for type 1 diabetes. But until there is a cure, the most exciting advancement to date are devices that pair an insulin pump with a device that continually monitors an individual’s blood glucose level and uses mathematical algorithms to function as an artificial pancreas. These “closed-loop systems”, once perfected, have the potential to free individuals with diabetes from the daily management of their diabetes and relieve them of the fears of complications.
Type 2 Diabetes
The other 90 to 95 percent of diabetes cases are type 2 diabetes. Type 2 diabetes is defined as a metabolic disease of insulin insufficiency, but it is also caused by muscle, liver, and fat cells no longer responding to the insulin in the body (Figure 5.5.1 ). In brief, cells in the body have become resistant to insulin and no longer receive the full physiological message of insulin to take up glucose from the blood. Thus, similar to patients with type 1 diabetes, those with type 2 diabetes also have high blood glucose levels.
For individuals with type 2 diabetes, the onset of symptoms is more gradual and less noticeable than for those with type 1 diabetes. The symptoms are increased thirst and urination, unexplained weight loss, and hunger. The first stage of type 2 diabetes is characterized by high glucose and insulin levels. This is because the insulin-secreting cells in the pancreas attempt to compensate for insulin resistance by making more insulin. In the second stage of type 2 diabetes, the insulin-secreting cells in the pancreas become exhausted and die. At this point, people with type 2 diabetes also have to be treated with insulin injections. The goal of diabetes prevention is to prevent or slow down how quickly the second stage happens. As with type 1 diabetes, chronically high glucose levels cause big detriments to health over time, so another goal for patients with type 2 diabetes is to properly manage their blood glucose levels. The front-line approach for treating type 2 diabetes includes eating a healthy diet and increasing physical activity.

Figure 5.5.1: Type 2 diabetes is a metabolic disease characterized by high blood glucose levels.
The Centers for Disease Control Prevention (CDC) estimates that as of 2015, more than 30 million Americans have diabetes, which is 9.4 percent of the population.1 In 2017, the total cost of diagnosed diabetes in the United States was estimated at $327 billion dollars.2 The incidence of Type 2 diabetes has more than doubled in America in the past thirty years and the rise is partly attributed to the increase in obesity in this country. Genetics, environment, nutrition, and lifestyle all play a role in determining a person’s risk for Type 2 diabetes. We have the power to change some of the determinants of disease, but not others. The Diabetes Prevention Trial that studied lifestyle and drug interventions in more than three thousand participants who were at high risk for Type 2 diabetes found that intensive lifestyle intervention reduced the chances of getting Type 2 diabetes by 58 %.3
Video 5.5.1: Do You Have High Blood Sugar?
A more in-depth view of blood sugar and your health.
“What is Diabetes?”
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
Published on Aug 3, 2016
Having more than one risk factor for type 2 diabetes substantially increases a person’s chances of developing the disease. Metabolic syndrome refers to a medical condition in which people have three or more risk factors for type 2 diabetes and cardiovascular disease (Figure 4.5.2 ). According to the International Diabetes Federation (IDF), people are diagnosed with this syndrome if they have central (abdominal) obesity and any two of the following health parameters4:
- triglycerides greater than 150 mg/dL
- high-density lipoproteins (HDL) lower than 40 mg/dL
- systolic blood pressure above 100 mmHg, or diastolic above 85 mmHg
- fasting blood glucose levels greater than 100 mg/dL.
1 Centers for Disease Control and Prevention. Another 84 million have pre-diabetes. Diabetes Research and Statistics Accessed February 22, 2019.
2 “The Cost of Diabetes.” Accessed February 22, 2019
3 Knowler, W. C. et al. “Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin.” N Engl J Med 346, no. 6 (2002): 393–403.Accessed June 19, 2019.
4 International Diabetes Federation. “The IDF Consensus Worldwide Definition of the Metabolic Syndrome.” Accessed June 19, 2019.
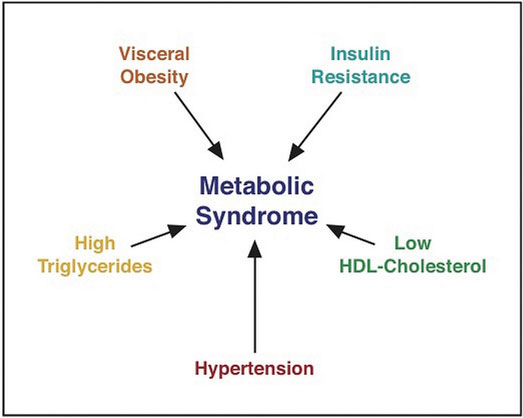
The five different causes of metabolic syndrome listed in this image are: High Triglycerides, Hypertension, Low HDL-Cholesterol, Insulin Resistance, and Visceral Obesity.
The I.D.F. estimates that between 20 and 25 percent of adults worldwide have metabolic syndrome. Studies vary, but people with metabolic syndrome have between a 9 and 30 times greater chance of developing Type 2 diabetes than those who do not have the syndrome.5
5 International Diabetes Federation. “The IDF Consensus Worldwide Definition of the Metabolic Syndrome.” Accessed June 19, 2019.
Gestational Diabetes
During pregnancy, some women develop gestational diabetes. Gestational diabetes is characterized by high blood glucose levels and insulin resistance. The exact cause is not known but does involve the effects of pregnancy hormones on how cells respond to insulin. Gestational diabetes can cause pregnancy complications and it is common practice for healthcare practitioners to screen pregnant women for this metabolic disorder. The disorder normally ceases when the pregnancy is over, but women who had gestational diabetes carry a lifetime risk of progression to type 2 diabetes of up to 60 percent.6 Gestational diabetes not only affects the health of a pregnant woman but also is associated with an increased risk of obesity and type 2 diabetes in her child.
6 Noctor E, Dunne FP. Type 2 diabetes after gestational diabetes: The influence of changing diagnostic criteria. World J Diabetes. 2015;6(2):234–244. DOI:10.4239/wjd.v6.i2.234. Accessed June 19, 2019.
Pre-diabetes
As the term infers, prediabetes is a metabolic condition in which people have moderately high glucose levels, but do not meet the criteria for diagnosis as a diabetic. “The Center for Disease Control and Prevention states that over eighty-four million Americans – more than 1 out of 3 – have pre-diabetes and are at increased risk for type 2 diabetes and cardiovascular disease. Of those with pre-diabetes, 90% do not know they have it.”7
“You can have prediabetes for years but have no clear symptoms, so it often goes undetected until serious health problems such as type 2 diabetes show up. It’s important to talk to your doctor about getting your blood sugar tested if you have any of the risk factors for prediabetes, which include:
- Being overweight
- Being 45 years or older
- Having a parent, brother, or sister with type 2 diabetes
- Being physically active less than 3 times a week
- Ever having gestational diabetes (diabetes during pregnancy) or giving birth to a baby who weighed more than 9 pounds
- Having polycystic ovary syndrome
Race and ethnicity are also a factor: African Americans, Hispanic/Latino Americans, American Indians, Pacific Islanders, and some Asian Americans are at higher risk.”7
Take the type 2 diabetes risk test here.
7Center for Disease Control and Prevention. Pre-Diabetes-Your Chance to Prevent Type 2 Diabetes. Accessed June 19, 2019
Long-Term Health Consequences of Diabetes
The long-term health consequences of uncontrolled diabetes are severe. They are the result of chronically high glucose concentrations in the blood accompanied by other metabolic abnormalities such as high blood lipid levels. People with diabetes are between two and four times more likely to die from cardiovascular disease. Diabetes is the number one cause of new cases of blindness, lower-limb amputations, and kidney failure. Many people with diabetes develop peripheral neuropathy, characterized by muscle weakness, loss of feeling, and pain in the lower extremities. More recently, there is scientific evidence to suggest people with diabetes are also at increased risk for Alzheimer’s disease. The good news is that complication rates are dropping as more people with diabetes are diagnosed earlier and are able to work with their health care teams to manage their diabetes and keep blood glucose levels closer to the normal range.
Video 5.5.2: Diabetes and Associated Complications
Watch this video to learn more about the whole-body complications associated with diabetes.
“Diabetes & Associated Complications”
Boehringer Ingelheim
Published on Sep 7, 2009
Diabetes Treatment
Keeping blood glucose levels in the target range (70–130 mg/dL before a meal) requires careful monitoring of blood glucose levels with a blood glucose meter, strict adherence to a healthy diet, and increased physical activity. People with type 1 diabetes begin insulin injections as soon as they are diagnosed. People with type 2 diabetes may require oral medications and/or insulin injections to maintain blood glucose levels in the target range. The symptoms of high blood glucose, also called hyperglycemia, are difficult to recognize and are mostly not apparent until levels become very high. The symptoms are increased thirst and frequent urination. Individuals may have an increased risk of infections as well. Having too low blood glucose levels, known as hypoglycemia, is also detrimental to health. Hypoglycemia is more common in people with type 1 diabetes and is most often caused by injecting too much insulin or injecting it at the wrong time. The symptoms of hypoglycemia are more acute including shakiness, sweating, nausea, hunger, clamminess, fatigue, confusion, irritability, stupor, seizures, and coma. Hypoglycemia can be rapidly and simply treated by eating foods containing about ten to twenty grams of fast-releasing carbohydrates. If symptoms are severe a person is either treated by emergency care providers with an intravenous solution of glucose or given an injection of glucagon, which mobilizes glucose from glycogen in the liver. Some people who do not have diabetes may experience reactive hypoglycemia. This is a condition in which people are sensitive to the intake of sugars, refined starches, and high GI foods. Individuals with reactive hypoglycemia have some symptoms of hypoglycemia. Symptoms are caused by a higher than normal increase in blood insulin levels. This rapidly decreases blood-glucose levels to a level below what is required for proper brain function.
The major determinants of type 2 diabetes that can be changed are overnutrition and a sedentary lifestyle. Therefore, reversing or improving these factors by lifestyle interventions markedly improve the overall health of type 2 diabetics and lower blood glucose levels. In fact, it has been shown that when people are overweight, losing as little as nine pounds (four kilograms) decreases blood-glucose levels in type 2 diabetics. The Diabetes Prevention Trial demonstrated that by adhering to a diet containing between 1,200 and 1,800 kilocalories per day with a dietary fat intake goal of less than 25 percent and increasing physical activity to at least 150 minutes per week, people at high risk for Type 2 diabetes achieved a weight loss of 7 percent and significantly decreased their chances of developing Type 2 diabetes. Since the trial ended, research has shown that almost any method of losing and maintaining weight loss through changes in lifestyle will prevent diabetes. The CDC has developed the National Diabetes Prevention Program, a partnership of public and private organizations to reduce the burden of diabetes in the U.S population.
The American Diabetes Association (ADA) has a website that provides information and tips for helping people with diabetes answer the question, “What Can I Eat” (see Interactive 5.5.1). In regard to carbohydrates, the ADA recommends people with diabetes keep track of the carbohydrates they eat and set a limit. These dietary practices will help keep blood glucose levels in the target range.
Interactive 5.5.1
The ADA has a website containing great information and tips on how to eat a healthy diet that helps keep blood glucose levels in the target range. Visit this What can I eat? to learn more about how to prevent serious complications of this disease.
In addition, see the infographic below for a summary of all of the different types of eating patterns that are being used in diabetes.8
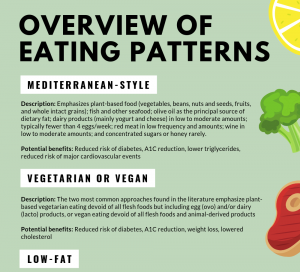
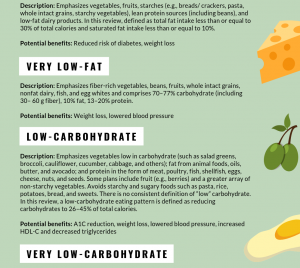
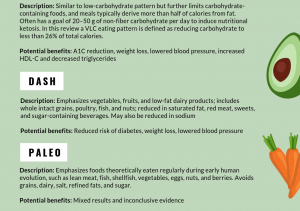
This infographic was adapted from the American Diabetes Association Consensus Report on Nutrition Therapy for Adults with Diabetes or Prediabetes. Permission granted for use from authors.
8McDermott, J, and Brown, A. Diatribe.org. What to Eat with Diabetes or Prediabetes: ADA’s New Nutrition Guidelines 5/9/19. Accessed June 19, 2019.
An unfortunate problem is that most people with diabetes find it difficult to make lifestyle interventions long-term. In order to make long-term lifestyle changes, individuals need to build a significant support system and have regular access to health care. Health insurance companies do not provide continued financial support for lifestyle guidance and primary care physicians often do not make referrals to a Registered Dietitian Nutritionist. This shifts the way diabetes is treated away from lifestyle intervention toward medications, as the goal still remains to manage blood-glucose levels. Numerous oral medications are available on the market and are often prescribed to people with type 2 diabetes in combination.
Knowler, W. C. et al. “Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin.” N Engl J Med 346, 6, 2002: 393–403.
Key Takeaways
- Diabetes is a disease of insulin deficiency and glucose over-sufficiency. Like other diseases, genetics, nutrition, environment, and lifestyle are all involved in determining a person’s risk of developing diabetes.
- Type 1 diabetes was once a death sentence, but now can be treated with insulin injections. Type 1 diabetes is still a death sentence in countries around the world where refrigeration and health care access is lacking.
- Insulin injections do not cure Type 1 diabetes, and people with diabetes can suffer many disease complications. Diabetes complications can be prevented by strictly managing blood-glucose levels, adhering to a healthy diet, and increasing physical activity.
- The incidence of type 2 diabetes has more than doubled in the United States and around the world in the past thirty years and the rise is partly attributed to the increase in obesity. Incidence has risen faster in low and middle-income countries. The front-line approach for treating people with type 2 diabetes includes eating a healthy diet and increasing physical activity.
- The long-term health consequences of diabetes are severe. They are the result of chronically high glucose concentrations in the blood and other metabolic abnormalities such as high blood lipid levels.
Discussion Starters
- If you owned a grocery store what are some practices you could introduce to combat the epidemic of Type 2 diabetes in this country?
- What are some options for you to intervene in your lifestyle and decrease your risk for type 2 diabetes?
- Do you know your risk for diabetes? Have any of your relatives been diagnosed with diabetes or pre-diabetes?

